|
Causes
Certain diseases of the eye are associated with zonular weakness or insufficiency. The most common one is pseudoexfoliation. “In patients with pseudoexfoliation, when you look at the eye, it looks like part of the lens capsule is peeling. We have realized that these are actually deposits of material on the lens capsule, but it looks like a layer flaking off the lens capsule, hence the name,” says Uday Devgan, MD, a surgeon from Los Angeles.
Pseudoexfoliation can almost always be seen preoperatively. It can make the zonules very weak and can also affect pupil dilation.
There are varying degrees of pseudoexfoliation. Some cases are very mild with a few subtle signs, and cataract surgery can be uneventful. Then, in some cases of severe pseudoexfoliation, when the surgeon attempts to remove the cataract, the zonules can fail and the whole cataract can fall into the back of the vitreous.
“To determine the severity of pseudoexfoliation preoperatively, assess how well the pupil dilates, and compare the anterior chamber depth to the axial length of the eye,” Dr. Devgan says. “In the normal eye, the zonules hold the lens (the cataract) in place. If the zonules are weak, that cataract tends to push forward and push the back of the iris toward the front of the eye. As it pushes, it shallows the anterior chamber, so the warning sign is presence of a shallow anterior chamber in an eye where you wouldn’t expect it. Usually, shallow anterior chambers are associated with short, tiny eyes. When you have a normal-sized eye, but the anterior chamber is shallow, that may be a sign.”
Some patients with pseudoexfoliation have frank phacodonesis. “If we see that preoperatively, it is a big issue. Then, in very severe cases, the zonules are so compromised already that we see a gap where the zonules are absent or missing or the cataract itself is decentered,” he adds.
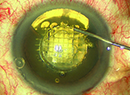
In the OR, at the beginning of the case, one of the first signs of weak or insufficient zonules is a lens capsule that is not taut. “Normally, the lens capsule is taut like the head of a drum. If a drum is taut, it can be easily penetrated with a sharp instrument,” Dr. Devgan says.
|
Management
Once it has been determined that a patient has zonular weakness, the surgeon must decide whether to proceed with surgery while being extra cautious, or whether to use adjunctive devices to help support the capsule. According to Richard Hoffman, MD, who is in practice in Eugene, Ore., there are basically two devices to choose from: a capsular tension ring or capsule support hooks.
Dr. Hoffman notes that he used to prefer capsular tension rings, but is now moving more toward using the hooks. “You can also use a combination of both,” he says. “You can put the capsular tension ring in before you start the phacoemulsification and then support the capsule with capsule hooks in extreme cases. Even in eyes that have had significant phacodonesis, lately I have just been using capsule hooks.”
Capsular tension rings support the zonules centrifugally but they don’t necessarily support the up and down movement of the lens. “I actually started using capsule hooks in patients who had zonular weakness and had previous vitrectomies because there is no vitreous support behind the lens and you get a lot of anterior and posterior movement of the capsule either during the chopping maneuvers or during the phaco. This seemed to support the zonules better than just a capsular tension ring,” says Dr. Hoffman.
Additionally, Dr. Hoffman notes that it can be difficult to remove the cortex if a capsular tension ring is used at the beginning of the procedure. For this reason, many surgeons tend to place the ring at the end of the procedure or near the end. “However, if you use a capsular tension ring, it is going to be most valuable at the beginning of the procedure, but it makes removal of the cortex a little more challenging,” he adds.
Dr. Chang agrees. For severe zonular laxity, he uses capsule retractors to stabilize the capsular bag. “One can use flexible iris retractors for this purpose, but capsule retractors have a much longer tip that better supports the periphery of the capsular bag. The retractors provide numerous advantages for phaco. They support the bag in the axial direction, they provide rotational stability so that the nucleus can be rotated without stripping the weakened zonules, and they restrain the capsular equator from being aspirated into the phaco tip. Finally, compared to a capsular tension ring, capsule retractors do not impede aspiration of the cortex,” he says.
He typically delays implantation of a capsular tension ring until after the cortex is evacuated, but prior to removal of the capsular retractors. “In this way, the bag is supported and stabilized against the decentering forces of the capsular tension ring as it opens,” he explains.
Another option is an Ahmed ring segment, which is a smaller segment of a capsular tension ring, Dr. Hoffman says. “Especially if a patient has a subluxed lens, I will put in an Ahmed ring segment. You can support a ring segment with a hook to support that quadrant of the lens. I will usually use the capsule hooks, then if I need to sew in a segment, I will do that after I’ve removed the cataract,” he explains.
|
“The reason I put a capsular tension ring in at the end of the procedure is twofold. First, I think it decreases the severity of anterior capsule phimosis. It may help support the zonules so that patients are less likely to have late lens subluxations but it does not guarantee the avoidance of that. Patients still get subluxations of their capsular bag and their lens with the capsular tension ring in place, but it’s possible that it might delay the onset of that. The main reason is that there are a small percentage of patients with pseudoexfoliation who undergo cataract surgery, and there is not much zonular weakness immediately after surgery. Then, seven to 10 years after their surgery, the zonules come loose, and their lens subluxes. If there is a capsular tension ring in the capsular bag, it makes it very easy to sew the bag to the sclera. You don’t have to worry about where the haptics are. That’s my reason now for putting capsular tension rings in my pseudoexfoliation patients, usually at the end of the procedure,” he explains.
Only patients with pseudoexfoliation experience late subluxations. “With trauma patients, pretty much what they have the week after surgery is what they are going to have for the rest of their life. It is unlikely that they will get progressive zonular degradation and late lens subluxations,” Dr. Hoffman adds.
Dr. Devgan says that he prefers the Mackool Capsule Support hooks, made by multiple manufacturers. Capsule support hooks go through the side-port incisions to hold and stabilize the capsule. “Once the cataract is removed, if there is a focal area of zonular weakness, and you don’t anticipate it getting worse in the future, you can put in a capsular tension ring. The ring distributes the forces more evenly and helps stabilize the capsule. In some situations where there is a more significant amount of weakness, you may have to put in a capsular tension ring that has a little eyelet in it, such as a Cionni ring. The eyelet allows you to tie a suture through it and to fixate the lens and the whole capsular bag to the sclera,” he explains.
He notes that the capsular bag is not salvageable in some patients and must be removed before the procedure. “Then, you will have to sew a lens in either to the back of the iris or trans-sclerally or maybe put an anterior chamber lens inside the eye. The key is to not be surprised and to try to identify things ahead of time. Be very alert when you first start the capsulorhexis, and look for weakness. If it’s there, prepare for it,” he says.
If the zonules are weak due to trauma, the patient will most likely have a good outcome because he or she is unlikely to suffer additional trauma in the future. “In contrast, pseudoexfoliation is a progressive disease over time, and I’ve only seen the ball roll downhill. However, you can make it roll downhill a little slower,” Dr. Devgan adds.
Because patients with severe pseudoexfoliation can get late dislocation of the entire lens, Dr. Devgan places a capsular tension ring or uses a three-piece lens design, because they are more amenable to suture fixation. “If a patient’s lens starts to decenter five years after surgery, I can go back in the eye and suture that lens in place to the back of the iris or the sclera,” he adds.
Other Tips
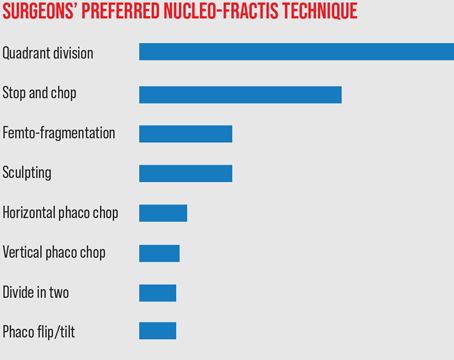
Dr. Hoffman notes that if he has a pseudoexfoliation patient whose capsule does not wrinkle significantly during the capsulorhexis, then he proceeds with surgery without any adjunctive devices. He recommends bringing the nuclear fragments up into the anterior chamber to phaco them, because that puts less stress on the zonules. Additionally, avoiding excessive downward pressure on the lens during decompression following hydrodissection, and doing horizontal chopping rather than vertical chopping or sculpting puts less stress on the zonules. “You can get through many of these cases without using the devices if the zonules are in decent shape and you are very careful and gentle with your maneuvers inside the eye,” he says.
Dr. Devgan notes that one trick for performing a capsulorhexis in a patient with weak zonules is to hold the capsule with one forceps with your left hand as you tear it with your right hand. “Then, it will be easier to complete the capsulorhexis. Alternatively, you could use a femtosecond laser as long as the pupil dilation is good,” he says.
According to Dr. Chang, in a patient with weak zonules, phaco chop provides particular advantages because the nucleus is immobilized by the phaco tip against the centripetal force of the chopper. Compared to sculpting techniques, this reduction in stress on the zonules is very evident when chopping is visualized from the Miyake-Apple view in cadaver eyes. REVIEW