Artificial tears are a mainstay in the management of dry-eye symptoms, and there are numerous over-the-counter artificial tear products on the market today. Patients are often overwhelmed by the choices and do not understand the differences between them. When helping patients choose a tear, the most important considerations are the underlying cause of the dry eye and how often the patient is instilling drops.
“Self-selection of medications is not a good idea,” says John Sheppard, MD, professor of ophthalmology, microbiology and molecular biology at Eastern Virginia Medical School. “Invariably, when patients bring in their drops, they will be the Wal-Mart or Safeway brand of tears, which are by far the most inferior tears on the market. Or, worse yet, they will use a topical vasoconstrictor like Visine, which induces vascular fragility, rebound vasodilation and dependence upon the vasoconstrictor to maintain a quiet, white-looking eye. Many times, patients will present using drops every 30 minutes or every hour, and this has a deleterious effect on lifestyle and well-being.”
When choosing an artificial tear for patients, experts generally consider three questions: Based on disease severity and dosing, is the optimum artificial tear for this patient preserved or not preserved? Does the patient have more of an aqueous deficiency, mixed disease or an evaporative form of dry eye? How severe is it?
Preservatives
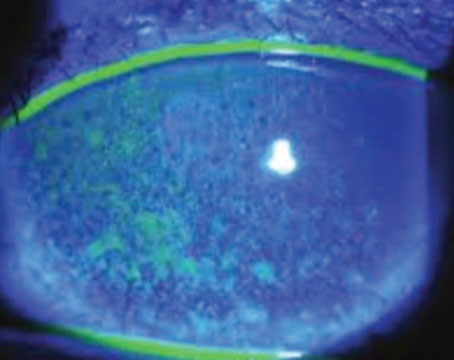
In recent years, there has been debate about whether the preservatives used in artificial tears are safe. While there are obvious advantages to the use of preservatives, several recent studies have highlighted the toxic effects of benzalkonium chloride. For example, a recent study conducted at the University of Illinois at Chicago found that topical application of BAK to the eye causes corneal neurotoxicity, inflammation and reduced aqueous tear production.1
|
Fortunately, patients with severe dry eye or patients who are hypersensitive to preservatives now have excellent choices of a totally preservative-free drop, according to Dr. Sheppard. “There are good choices from a wide variety of manufacturers, and they come in a single-dose unit (SDU) with a twist-off cap,” he says. “In theory, you take one dose, and you dispose of it. Careful handling of the SDU will allow multiple uses because many are re-cappable, and as long as you don’t contaminate the tip by touching your fingers, eyelids or eyelashes, then it can be reused at least over the course of one day. However, I don’t recommend that practice to unreliable patients,” he says.
If a patient requires a preservative-free preparation, Dr. Sheppard notes that a few good choices are Refresh (Allergan), TheraTears, Soothe (Bausch + Lomb) and Systane (Alcon). “You can never go wrong with these. It’s just a little more expensive and a little more time-consuming to apply the drops,” he adds.
Another choice is formulations containing vanishing preservatives. The preservatives basically turn into water or a non-toxic chemical when they are exposed to air or mix with the tear film. “The first vanishing preservative (sodium perchlorate) was introduced in the Genteal brand by Novartis, which is still available. Another brand of vanishing preservative is sodium chlorite or Purite from Allergan, which is found in a wide variety of their products, including all of their multi-dose preparations of the Refresh Optive brand of tears,” Dr. Sheppard explains.
Robert Latkany, MD, notes that cost can also play a role in artificial tear choice. “The preservative-free products can be double the cost of the preserved ones,” he says. “There have been studies showing that these preservatives are destroying the ocular surface, but I think it’s overstated and overhyped. If I can save some money for a particular patient and have him or her use Refresh Liquigel with a disappearing preservative rather than Refresh Celluvisc because they are using these products forever, numerous times a day, then I will take that into consideration. Many of these people see me every two to four weeks, so I can monitor the situation. If there is ever an issue with an artificial tear product, I pick up on it quickly,” says Dr. Latkany, founder of New York Eye and Ear Infirmary’s Dry Eye Clinic.
The choice between a tear with a preservative and a preservative-free tear comes down to the number of drops instilled in the eye daily. According to Stephen Pflugfelder, MD, director of the Ocular Surface Center at Baylor College of Medicine in Houston, it would be best for patients who use tears more than four times a day or who have severe dry eye to use a preservative-free unit-dose artificial tear.
Lipids
Another important approach to providing an excellent over-the-counter tear preparation is to attempt to mimic the biphasic nature of tears by providing a lipid and an aqueous component to the tear, Dr. Sheppard says. “The guar in Systane provides an excellent matrix for the aqueous component of the tear. Refresh Optive Advance as well as Soothe from Bausch + Lomb provide a lipid substitute to better stabilize the tear film. Another valuable additive to over-the-counter tears is hyaluronic acid, which can be found in Blink tears from Abbott,” he explains.
Viscosity
Another factor to consider when recommending drops is viscosity. Patients with mild dry eye may prefer a watery drop, while those with more severe dry eye may prefer a thicker drop that stays on the cornea longer.
|
Dr. Pflugfelder agrees that transient blurring can be a problem with more viscous drops. “Although the more viscous tears may decrease friction in the eye and lubricate the eye better, they do come with the side effect of being more blurry. In some cases, if someone can’t close his or her eye because he or she has Bell’s palsy, and a whole section of the inferior cornea is drying out, I definitely would recommend a thicker tear or a gel or even an ointment, knowing that although it may blur the patient’s vision, it would probably protect the eye better. People who have good vision and can blink normally don’t tend to like very viscous artificial tears. Some people use them at night, but you can even have blurred vision for an hour or so after you wake up in the morning,” he adds.
Osmolarity
Another differentiating feature among the drops is osmolarity. “Some tears have lower osmolarity,” Dr. Pflugfelder says. “There are some studies that show that lower osmolarity tears may have a better effect on the ocular surface. There are some tears that have ingredients that are called osmoprotectants. They are taken up by cells, and they blunt the response of the epithelial cells on the surface of the eye to high osmolarity in the tears. The Optive tears have osmoprotectants; some of those are found in sports drinks also because people can lose a lot of fluid and their blood may be a higher osmolarity. There is pretty good scientific evidence that they do help to protect cells.”
For example, a study conducted by Dr. Pflugfelder and his colleagues at Baylor found that the osmoprotectants L-carnitine and erythritol, alone or in combination, protect against stress activation of corneal epithelial cells cultured in hyperosmolar media.2
After a patient starts on an artificial tear, she needs frequent follow-up to determine whether the drop is relieving symptoms. “They may need to use the drop for a month or two before they can determine whether it will work for them,” says Dr. Sheppard.
Jay Pepose, MD, PhD, medical director of Pepose Vision Institute and president of the Lifelong Vision Institute, St. Louis, relies on a combination of symptoms and tear osmolarity to assess the efficacy of treatment. “I test patients’ tear osmolarity before I initiate treatment, and then I ask them not to use any tears or put anything in their eye for at least 30 minutes, but preferably for at least an hour, before they come in for follow-up, and then I re-test their tear osmolarity after they have been on a product for a few weeks,” he says. “Changes in tear osmolarity, along with vital staining and tear breakup time and reduction in symptoms, help me to decide whether patients are using the appropriate product or if we may need to switch tears, supplement treatment with cyclosporine, consider doxycycline or punctal plugs or add omega-3s.”
Dr. Latkany notes that artificial tears are helpful as adjunctive agents, but that they are not the answer for dry-eye patients. “None of these can come close to the complexity of our natural tears,” he says. “I am not in love with any of them, but we are improving the options. I think the marketing campaigns from the pharmaceutical companies make these products appear very attractive and very complex and to appear to be the answer to all dry-eye patients, but that is far from the truth, and we have a long way to go.” REVIEW
1. Sarkar J, Chaudhary, Namavari A, et al. Corneal neurotoxicity due to topical benzalkonium chloride. Invest Ophthalmol Vis Sci 2012;53(4):1792-1802.
2. Corrales RM, Luo L, Chang EY, Pflugfelder SC. Effects of osmoprotectants on hyperosmolar stress in cultured human corneal epithelial cells. Cornea 2008;27:574-579.