 |
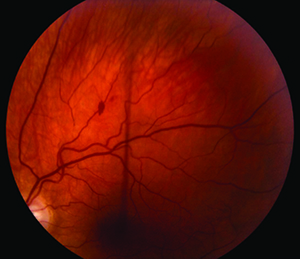
| Figure 1. Fundus photo of the left eye demonstrating a retinal hemorrhage superiorly. |
A 32-year-old Caucasian male presented with an acute onset of partial temporal visual field loss in the left eye over a period of a few days. The patient saw an ophthalmologist who, in the setting of an otherwise normal ocular exam, was concerned the patient was having a cerebrovascular accident. During a brief hospitalization, CT and MRI findings were thought to be due to atypical migraines. He did note a history of migraines and was having regular headaches that would last about one hour with visual “floaters.” According to the patient and records, there were no other neurological deficits at that time. Further stroke workup was negative. Upon routine follow-up a year and a half later, he continued to have his headaches as previously described but noted stable vision with no new changes. On review of systems, he noted occasional vertigo, which would last days to weeks at a time. He also reported decreased hearing in both ears with an increase in fatigue. He denied any weakness, numbness or loss of balance.
Medical History
Medical history was significant for hypertension, depression, gastroesophageal reflux disease, atypical migraines and Meniere’s disease (diagnosed at age 26). Ocular history included congenital dyschromatopsia and mild myopia. Surgical history was notable for prior appendectomy and cholecystectomy. He denied current tobacco (noted a prior 15 pack-year history), alcohol or illicit drug use. Employment included secretarial work.
Medications include aspirin 81 mg p.o. daily, amlodipine 10 mg-benazepril 20 mg p.o. daily, clonazepam 0.5 mg p.o. b.i.d. as needed for anxiety, ranitidine 25 mg p.o. daily, meclizine 25 mg p.o. b.i.d., and Zoloft 100 mg p.o. daily.
Examination
Initial presentation revealed a completely normal systemic and ocular exam with the exception of temporal field defect in the left eye by confrontation visual fields.
On follow-up examination a year and a half later, vital signs were stable and within normal limits. The patient was oriented to person, place and time but was somewhat drowsy during the visit with a slow thought process. Ocular exam revealed best-corrected visual acuity to be 20/20 OU. He denied subjective color or light desaturation. Pupils were equally round and reactive to light without a relative afferent pupillary defect. Amsler grid was full OU. Confrontation visual field was notable for nasal defects in the left eye. Extraocular motility was full OU.
Anterior slit-lamp examination was normal OU. Dilated fundus exam was normal OD and revealed vitreous syneresis, attenuated vessels and a small retinal hemorrhage superiorly (See Figure 1) OS.
What is your differential diagnosis? What further workup would you pursue?
Please click this link for diagnosis, workup, treatment and discussion.
Please click this link for diagnosis, workup, treatment and discussion.



