Some people seem to go through life with the attitude that the world is out to get them. But those of us with seasonal allergies know this to be a fact. While others cheer the arrival of birds, flowers and all the assorted harbingers of spring, allergics prepare for another round of battle with pollens, armed only with eye drops and nasal spray. Just what makes pollens such efficient vectors of misery? This month we will examine the nature of pollinosis, a condition more commonly known as hay fever, rhinitis or, in its ocular incarnation, seasonal allergic conjunctivitis.
A Peek Inside Pollination
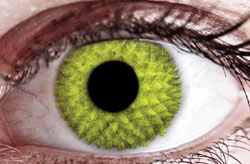
Pollens are the male gametes of plants, and as such, they are engineered for reproduction.1 It turns out that plants have evolved three distinct mechanisms for pollen transfer: by insect; animal; or through the air. Pollen transfer by air, or anemophily, is predominant in temperate regions and is the mechanism employed by most grasses and weeds, and by many tree varieties. The dominance of insect and animal-based pollination mechanisms in the tropics is one factor in the lower prevalence of pollinosis in those regions.
|
An important factor in the prevalence of pollinosis is the prodigious capacity of many species of plants to synthesize and distribute pollens. For example, an acre of ryegrass is capable of producing nearly 200 kg of pollen in a single bloom.3 Pollen production, particularly with tree species (such as birch, cedar and oak) is synchronized with flower production and so is optimized to generate bursts of pollen release and dispersal.4 As with all forms of reproduction, airborne pollination is a competition, so plants are compelled to produce large pollen yields in short time frames in order to be successful. Unfortunately, allergenic pollen producers appear to have organized their assault on our immune systems with a well-designed schedule of pollination that provides allergen nearly year-round, from spring trees to summer grasses to fall weeds.
Perhaps the most important aspect of pollen biology is that all pollens are decidedly not equal when it comes to eliciting allergic signs and symptoms, and it is the nature of the allergens carried by each pollen that determines whether it will elicit an allergic response.
Pollens Aren’t Created Equal
Despite the tremendous diversity of plant species around the globe, there are relatively few that release pollens capable of eliciting allergic reactions (See Table 1). Of an estimated 200,000 known species of plants, only 50 are listed as airborne allergen sources by the International Union of Immunological Societies.5 While many grass pollens are allergenic, only a handful of tree species, including birch, alder, cypress and cedar are responsible for the majority of pollen-evoked allergies. Similarly, a few species of weeds, including mugwort and, of course, ragweed, dominate the fall allergy season. When a limited number of species produce the majority of allergenic pollens, it means that atopic individuals can benefit by a careful consideration of their landscaping choices. For example, grasses such as St. Augustine (genus Stenotaphrum) reproduce primarily by stolons (runners) and so are far less allergenic than bermuda or ryegrasses.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Another recent series of studies has shed light on causes of increased prevalence of allergies, including allergic conjunctivitis. There is growing evidence that pollutants can interact with pollen allergens; the result is a greater antigenicity and increases in allergic disease. For example, controlled studies showed that increased atmospheric carbon dioxide can cause a significant increase in the amount of pollen produced by several species of grasses.9 Hydrocarbons and other components of exhaust can also interact with pollens, acting as adjuvants to increase their antigenicity and potentiating the immune responses elicited by a given pollen allergen.
For clinicians it’s important to realize that there is considerable cross-reactivity in immune responses to some pollen allergens, and this can significantly impact both the severity and duration of the allergy season for many patients. A well-documented example of this is seen in Japan, where increased incidence of rhinitis and allergic conjunctivitis is blamed primarily on pollens from two species, the Japanese Cedar (Cryptomeria japonica) and the Japanese Cypress (Chamaecyparis obtusa).10,11 Both C. japonica and C. obtusa trees produce prodigious amounts of pollen, but just as important is the timing of these events: C. japonica flowers first, in early February to March, while C. obtusa blooms from March to late April. And where there are flowers blooming, there is pollen. To make the situation worse, subjects allergic to C. japonica pollen typically exhibit a cross-reactivity making them susceptible to C. obtusa as well. Thus, the most important factor isn’t the specific pollen species or the maximum pollen levels on a particular day, but the fact that the susceptible individuals are exposed to high levels of pollen over a protracted period of time.
Most recent efforts to classify allergens according to antigenicity have been developed to address the observed cross-reactivity that goes beyond the level of related plant species. For example, many patients who are allergic to fruits such as apples and pears also suffer from allergic conjunctivitis in response to birch or alder pollens. A newer set of allergen families contained within a group termed panallergens represent allergens classified according to three-dimensional molecular structures and feature functions that sometimes aren’t immediately apparent from isolated analysis.5 Three well-defined families include profilins (cytoskeletal binding proteins), polcalcins (calcium binding proteins, such as calmodulin or cyclophilin) and lipid transfer proteins. Another large, diverse group that shares functional traits includes allergens with catabolic activity, including pectin- and sugar-degrading enzymes. Most allergenic plant species produce allergens from multiple groups (See Table 1), adding to the complexity. One value of such classifications will be in future efforts to use immunotherapy treatments: In theory, it should be possible to use the knowledge of these panallergens to produce family-specific immune therapies.
Keeping Up the Fight
For those of us who are particularly interested in ocular allergy, it’s comforting to see that the most recent developments in studies of pollen and pollen allergens provide further validation for the conjunctival allergen challenge model. The CAC model was designed to provide a way to elicit allergic responses that were predictable and reproducible so that they could be used to develop new therapeutics for allergy treatment and prevention.12 During the screening process in a typical CAC study, each subject receives a skin test which qualitatively identifies the allergens to which the subject is sensitized. One of these allergens is then instilled in the eye, and the redness and itching responses are quantified. If the response doesn’t reach the protocol-defined threshold, a higher concentration of the same allergen is tried. This process is repeated until an adequate response is achieved, and a different allergen may eventually be used if the first doesn’t produce the desired response. At the end of this allergen titration process, each qualified subject has demonstrated a similar response within a pre-defined range. The key features of the CAC that have been validated by subsequent years of studies are that the specific allergen and allergen concentration may differ from subject to subject, but the mechanism of the allergic response is the same regardless of the allergen used. As our knowledge of pollens and the allergens carried by pollens has advanced, we have seen that the nature of the immune responses elicited by different pollens is the same, as experience with the CAC would predict.
The prevalence of allergic disease has been on the rise in recent decades, and during this time clinicians have also realized that, for a growing subpopulation of allergy sufferers, the conventional antihistamine-mast cell stabilizer medications are insufficient as treatment. It’s likely that this trend results both from increases in the amounts of pollen produced and from the effects of environmental pollutants discussed above. Despite these factors, it seems worth asking if, at some level, this trend reflects a qualitative change in allergic responses to the same varieties and concentrations of allergens. Emerging evidence suggests that this growing population of non-responders reflects an increase in prevalence of late-phase allergy.13
Manifestations of late-phase allergic reactions occur approximately six to 24 hours after allergen exposure, and are characterized by prolonged ocular signs and symptoms as well as a greater degree of a cellular aspect of the response: preformed mediators of the acute phase elicit an influx of inflammatory cells, particularly eosinophils, into the conjunctiva. In the eye, the cellular late-phase reaction may only be present in a subset of patients and, when present, is generally asymptomatic, except in relatively rare cases.14
As with all ocular diseases, a key approach to development of improved therapies for late-phase allergy is to design and validate models that accurately reflect disease signs and symptoms. For the example of the CAC described above, one would simply modify the assay in order to elicit some or all of the features of late-phase allergy in a particular patient. These modified models employ a repeated exposure to titrated amounts of allergen to elicit the inflammatory reaction characteristic of the non-responder population. With the understanding that the prevalence of this condition is on the rise, these efforts are under way and should lead to new treatments in the near future.15,16 REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at the Schepens Eye Research Institute. Drs. McLaughlin and Coderre are medical writers at Ora Inc.
1. Leuschner RM. Pollen. Experientia 1993;49:931-42.
2. Hassan MS, Lau R. Inhalation performance of pollen-shaped carrier in dry powder formulation: Effect of size and surface morphology. Int. J. Pharmaceutics 2011;413:93-102.
3. Nox B, Suphioglu C. Environmental and molecular biology of pollen allergens. Trends Plant Sci 1996;1:156-162.
4. Burge HA, Rodgers CA. Outdoor Allergens. Environmental Health Perspectives. 2000;108(S4):653.
5. Hauser M, Roulias A, Ferreirra F, Egger M. Panallergens and their impact on the allergic patient. Allergy, Asthma, Clin Immunol 2010;6:1-14.
6. Runswick S, Mitchell T, Davies P, Robinson C, Garrod DR. Pollen proteolytic enzymes degrade tight junctions. Respirology 2007;12:6: 834-842.
7. Gunawan H, Takai T, Ikeda S, Okumura K, Ogawa H. Protease activity of allergenic pollen of cedar, cypress, juniper, birch and ragweed. Allergol Int 2008;57:83-91.
8. Ibrahim AR, Kawamoto S, Aki T, Shimada Y, Rikimaru S, Onishi N, Babiker EE, Oiso I, Hashimoto K, Hayashi T, Ono K. Molecular cloning and immunochemical characterization of a novel major Japanese cedar pollen allergen belonging to the aspartic protease family. Int Arch Allergy Immunol 2010;152:207-218.
9. Wolf J O’Neill NR, Rogers CA, Muilenberg ML, Ziska LH. Elevated atmospheric carbon dioxide concentrations amplify alternaria alternata sporulation and total antigen production. Environmental Health Perspectives 2010;118:1223-1226.
10. Kishikawa R, Sahashi N, Saitoh A, Kotoh E, Shimoda T, Shojo S, Akiyama K, Nishima S. Japanese Cedar Airborne Pollen Monitoring by Durham’s and Burkard Samplers in Japan - Estimation of the Usefulness of Durham’s Sampler on Japanese Cedar Pollinosis. Global Environmental Research 2009;13:55-62.
11. Okamoto Y, Horiguchi S, Yamamoto H, Yonekura S, Hanazawa T. Present situation of cedar pollinosis in Japan and its immune responses. Allergol Int 2009;58:155-162.
12. Abelson MB, Chambers WA, Smith LM. Conjunctival allergen challenge. A clinical approach to studying allergic conjunctivitis. Arch Ophthalmol 1990;108:84-88.
13. Choi SH, Bielory L. Late-phase reaction in ocular allergy. Curr Opin Allergy Clin Immunol. 2008;8:438-444.
14. Leonardi A, Abelson MB. Double-masked, randomized, placebo-controlled clinical study of the mast cell-stabilizing effects of treatment with olopatadine in the conjunctival allergen challenge model in humans. Clin Ther 2003;25:2539-2552.
15. Mishra GP, Tamboli V, Jwala J, Mitra AK. Recent patents and emerging therapeutics in the treatment of allergic conjunctivitis. Recent Pat Inflamm Allergy Drug Discov 2011;5:26-36.
16. Gomes PJ, Abelson MA. Comparison of environmental and allergen-challenge assessments of allergic conjunctivitis treatment using an antihistamine-steroid combination therapy. J Allergy Clin Immunol 2012;129:2(S):190.