It’s hard to overestimate the problem of drug-resistant pathogens. In the United States alone, microorganisms live with a constant pressure to respond to more than 15 million kg of antibiotic introduced into the environment annually.1 Recent Centers for Disease Control and Prevention estimates suggest that somewhere between 20,000 to 40,000 people (old and young) die in the United States annually from bacterial infections resistant to antibiotic therapy. While ocular infections rarely lead to death, there is significant morbidity associated with infectious keratitis, uveitis and endophthalmitis due to resistant strains of microbes.
A number of studies have established that antibiotic therapy leads to dramatic changes in both the relative populations of commensal species and the frequency of antibiotic resistance.2,3 Data from the human biome project has established a basic paradigm that with antibiotic therapy comes a decrease in the diversity of commensal species, as well as a trend toward increased pathogenicity of bacteria that are normally innocuous.4 Based on the 2009
ARMOR study,there is an increasing incidence of resistant pathogens taken from bacterial eye infections in the United States, including methicillin-resistant coagulase-negative Staphylococcus strains and methicillin-resistant Staphylococcus aureus.5 Additionally, a 2008 New York Eye and Ear Infirmary study demonstrated that the incidence of both S. aureus and MRSA increased dramatically in bacterial conjunctivitis patients from 1998 to 2008.6 Moreover, gram negatives such as Acinetobacter or Pseudomonas are now typically resistant to multiple antibiotics, and have expanded their range such that they are no longer considered primarily nosocomial pathogens.7
Antimicrobial Development
What’s clear is that combating the problem of antibiotic resistance requires a combination of three elements: infection control; antibiotic stewardship; and development of new compounds.1 Infection control and stewardship are the public-health policies and procedures implemented at hospitals and other health-care facilities that will combine the strictest hygiene protocols with spare, judicious use of the most potent antibiotics only in those cases where infection by a resistant microbial strain is established. There is also a need for new therapeutics, including the next generation of existing drug classes, as well as agents with new mechanisms of action.
It may seem surprising that as we watched the issue of antibiotic resistance grow ever more problematic, progress in development of new anti-infectives ground to a halt. This reflects a mixed bag of forces acting on this therapeutic space. In ophthalmology, the dearth of new products is due in part to the high efficacy of fourth-generation fluoroquinolones that have occupied the largest segment of the market since their introduction in 2003. At the same time, many pharmaceutical companies exited the antibiotic development arena, preferring to focus on other therapeutic areas. A number of advocacy groups and governmental agencies have voiced their concerns about this therapeutic innovation vacuum. The Infectious Disease Society of America proposed a response to the need in 2010, with the “10 x ’20 Initiative,” a global commitment to develop 10 new antibacterial agents by 2020.8 In 2012, the U.S. Congress passed the Generating Antibiotic Incentives Now Act, a program that provides for extended patent exclusivity and accelerated review for new antibiotics targeted toward serious and life-threatening infectious diseases.9 This is a key step, since the biggest impediment to new antibacterial drug development is the lack of an economic incentive: Regardless of demand, it’s not feasible to bring a new drug to market with no possibility of recouping the costs of clinical development. The jury is out on whether these initiatives will lead to improved tools to combat ocular infections.
Assessing the Need
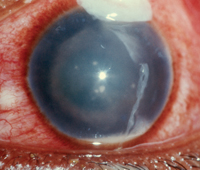
Ocular indications for anti-infective therapy include bacterial conjunctivitis, blepharitis, bacterial keratitis and endophthalmitis. Each of these conditions is most commonly associated with a handful of causative bacterial agents, and while the strains remain the same, rates of resistance are on the rise across the board. For example, while S. aureus is the most common culprit in bacterial conjunctivitis, the strains of S. aureus cultured from conjunctiva between 1994 and 2003 showed a threefold increase in ciprofloxacin resistance, and an almost tenfold increase in MRSA (4.4 percent to 42.6 percent).7 While most acute infections involve S. aureus or S. pneumoniae, gram negative pathogens such as H. influenzae are also seen, particularly in the pediatric population. It’s important to note that while external infections such as bacterial conjunctivitis are generally self-limiting, there remains a sound rationale for the use of topical antibiotics to shorten both the duration and the severity of the infections.10,11
|
Pipeline Perspective
With the slowdown in development, the ophthalmic medicine cabinet for bacterial infections hasn’t changed much in the past decade. Thankfully, there are encouraging signs of activity, an array of new compounds in the development pipeline, and the hope that some of these will be formulated and tested for ocular indications. Newer classes of compounds include anti-microbial peptides, bacterial biosynthetic inhibitors, biologicals and a host of next-generation compounds.13,14 A number of glycopeptide compounds such as Oritavancin (The Medicines Company) that act by inhibiting cell wall biosynthesis have shown promise against gram positive organisms, including MRSA. While similar in action to vancomycin, compounds such as Oritavancin are active against most vancomycin-resistant strains. A related compound, Telavancin (Theravance), was approved for IV use against MRSA infections in 2009, but has seen limited use due to production issues.
Carbapenems are the most recently developed family of beta-lactam antibiotics and, like penicillins and cephalosporins, they exhibit broad-spectrum activity against gram positive and gram negative bacteria. None of the currently approved compounds have ocular indications, but several are in development. Another next-generation candidate is Plazomicin (Achaogen), a new aminoglycoside which, like its predecessors tobramycin and gentamycin, acts by inhibiting bacterial protein synthesis. Early studies suggest it’s more potent than others in this class, but a final verdict will come from ongoing studies.
|
ACH-702 has demonstrated the ability to kill fluoroquinolone-resistant S. aureus. Unlike the first generation of this drug class, ACH-702 has the ability to inhibit topoisomerase and DNA gyrase in resistant bacterial strains, and also demonstrated a 128-fold increase in the minimal inhibitory concentrations compared to moxifloxacin in resistant S. aureus clinical isolates.15 It’s thought that this new fluoroquinolone also exhibits a unique enzyme inhibitory activity against bacterial DNA primase, a novel bacterial target. This action is important for two reasons: it provides an MOA distinct from topoisomerase and DNA gyrase inhibition; and it allows the compound to target and kill metabolically active bacteria even in a non-dividing state. The unique features of ACH-702 represent the types of molecular strategies necessary to defeat the process of antibiotic resistance.
As with other candidate therapeutics, new antimicrobials will still require testing in an ocular setting before they can be brought to market for ophthalmic indications. Despite these hurdles, there does seem to be a renewed effort to identify and develop compounds that can address the problem of antibiotic resistance. For those whose sight is threatened by multidrug-resistant bacteria, these compounds will definitely qualify as wonder drugs. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School. Mr. Shapiro is vice president for anti-infectives at Ora Inc, where Dr. McLaughlin is a medical writer.
1. Spellberg B, Bartlett JG, Gilbert DN. The future of antibiotics and resistance. N Engl J Med 2013;368:299-302.
2. Dave SB, Toma HS, Kim SJ. Changes in ocular flora in eyes exposed to ophthalmic antibiotics. Ophthalmology 2013;120:937.
3. Kim SJ, Toma HS. Ophthalmic antibiotics and antimicrobial resistance. Ophthalmology 2011;118:1358-1363.
4. Gerber GK. The dynamic microbiome. FEBS Lett. 2014 Feb 28 [Epub ahead of print].
5. Haas W. et al. Monitoring Antibiotic Resistance in Ocular Microorganisms: Results from the Antibiotic Resistance Monitoring in Ocular Micro-organisms (ARMOR) 2009 Surveillance Study. Am J Ophthalmol 2011;152:567-574.
6. Adebayo A. et al. Shifting trends in in vitro antibiotic susceptibilities for common bacterial conjunctival isolates in the last decade at the New York Eye and Ear Infirmary. Grafes Arch Clin Exp Ophthalmol 2011;249:111-119.
7. Bertino JS, Impact of antibiotic resistance in the management of ocular infections: The role of current and future antibiotics. Clinical Ophthalmology 2009:3507-521.
8. Infectious Diseases Society of America. The 10 x ‘20 Initiative: Pursuing a global commitment to develop 10 new antibacterial drugs by 2020. Clin Infect Dis 2010;50:1081-3.
9. Tillotson GS. GAIN Act legislation: Is it enough? Lancet Infect Dis 2012;12:823-4.
10. AAO Preferred Practice Pattern: Conjunctivitis. http://one.aao.org/preferred-practice-pattern/conjunctivitis-ppp--2013 accessed 30 April 2014.
11. Sheikh A, Hurwitz B, van Schayck CP, McLean S, Nurmatov U. Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev 2012;9:CD001211.
12. Schimel AM, Miller D, Flynn, Jr HW. Endophthalmitis Isolates and Antibiotic Susceptibilities: A 10-Year Review of Culture-Proven Cases. Amer J Ophthal 2013;156:50–52.e1.
13. Wright GD. Something old, something new: Revisiting natural products in antibiotic drug discovery. Can J Microbiol 2014;60:147-154.
14. Kumar K, Chopra S. New drugs for methicillin-resistant Staphylococcus aureus: An update. J Antimicrob Chemother 2013;68:1465-1470.
15. Pucci MJ, Ackerman M, Thanassi JA, Shoen CM, Cynamon MH. In Vitro Anti-tuberculosis Activities of ACH-702, a Novel Isothiazoloquinolone, against Quinolone-Susceptible and Quinolone-Resistant Isolates. Antimicrobial Agents Chemother 2010;54:3478-3480.