|
Real-color Imaging
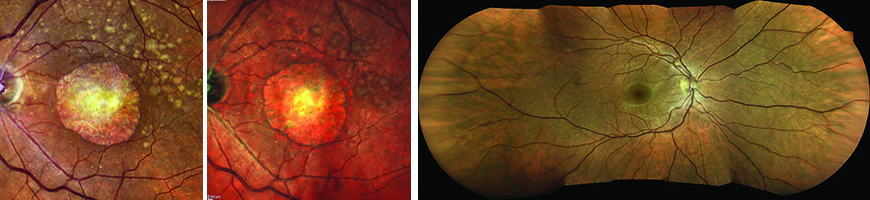
The Eidon confocal scanner (Centervue, Padova, Italy) received FDA clearance in December 2014. According to the manufacturer, Eidon is the only wide-view system that combines confocal imaging with natural white-light illumination to provide a true-color image, as opposed to the pseudo-color rendering generated by monochromatic lasers in scanning laser ophthalmoscope-based systems. The merging of color channels in that approach results in a bright orange retinal image, blood having a blue-green hue, and a dark or black optic nerve. (See example, facing page.) Centervue says that white-light illumination reveals greater detail of retinal pathologies and allows a clearer view of the optic nerve.
Other benefits of the Eidon, according to Centervue, include:
- • infrared and red-free confocal image options, presented with super-high resolution and contrast;
• non-mydriatic operation (2.5 mm minimum pupil size);
• the ability to image through cataract and media opacities;
• the ability to run in fully automated or manual modes;
• automatic alignment with the patient’s pupil and retinal focus;
• a compact, small-footprint design with standalone operation; and
• an exam time less than 30 seconds per eye for a single field.
|
Paolo Lanzetta, MD, professor and chairman of the Department of Medical and Biological Sciences-Ophthalmology at the University of Udine, Italy, has used the Eidon at a large-volume ambulatory surgery center in Udine. “Eidon is the first true-color scanning ophthalmoscope that uses confocal imaging and white light illumination integrated in a pupil-dilation-free system,” he says. “We’re very enthusiastic about its ability to generate high-quality, high-resolution, real-color pictures. It provides a retinal image that looks exactly as the retina looks when directly observed. This should provide new opportunities for early diagnosis of many retinal conditions.”
Dr. Lanzetta says he finds the device to be very versatile with its combination of multiple imaging modalities. “The instrument and the software interface are user-friendly and easy to learn,” he notes. “It requires minimal operator involvement; it automatically aligns with the patient’s pupil and focuses on the retina. At any time, it’s possible to stop the automatic alignment and switch to manual mode using the joystick, allowing us to customize focus and alignment to capture specific pathologies in detail.”
Pros and Cons
Dr. Lanzetta sees the Eidon as having some advantages in comparison to both conventional fundus cameras and other wide-field options. “Conventional fundus cameras capture color retinal images that are oversatured in the red channel, showing an optic disc that looks washed-out and uniform,” he points out. “Image acquisition may be limited by media opacities such as cataracts or corneal opacities, and the capture flash can be very disturbing for the patient. SLO systems are able to achieve better contrast compared to conventional fundus photography, but they typically use a single wavelength laser and provide monochromatic images—black and white or pseudo-color—and thus are unable to extract color information from the retina. A true color, high-resolution retinal image is essential for an accurate diagnosis.”
Dr. Lanzetta says that his clinic has used Optos’s Daytona instrument in the past. “Both the Daytona and Eidon are compact in design and extremely easy to use, although positioning the patient’s head and capturing the retinal image is easier with Eidon,” he says. (The manufacturer notes that the Eidon costs less than half as much as Optos’s California.)
Dr. Lanzetta says the Eidon does have some limitations. “Eidon is an excellent device, but the field of view should be increased,” he says. “Adding autofluorescence images or fluorescein angiography may provide additional diagnostic information. Also, Eidon’s optical system operates within the range of -12 D to +15 D. In eyes with a myopic refractive error of more than 12 D, Eidon may be unable to focus on the posterior pole and detect retinal conditions related to pathological myopia.”
Despite these limitations, Dr. Lanzetta says the Eidon device could be widely used as a screening tool in the primary-care setting for the detection of ophthalmic diseases such as diabetic retinopathy, glaucoma and age-related macular degeneration. “Eidon can be introduced into the daily practice for detecting posterior segment diseases and helping retinal physicians in the diagnosis and management of several retinal conditions,” he says. “It can easily be used by any type of personnel thanks to its automated mode.”
Next-generation Ultra Wide-field
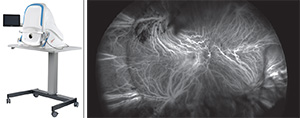
Optos’s recently approved California instrument is a compact, tabletop device that does non-mydriatic high-resolution ultra wide-field imaging (up to 200 degrees) through many cataracts, and pupils as small as
2 mm. According to Optos, other features include:
- • ultra wide-field indocyanine green angiography, in addition to the previously available composite color, red-free, autofluorescence and fluorescein angiography modes (the device allows parallel capture of fluorescein angiography and ICG images without manually switching between modalities);
• ProView software, which displays wide-field scans in a consistent geometry that accurately represents anatomical features in the retina;
• new proprietary optical hardware that optimizes resolution throughout retinal scans, resulting in more clarity in the periphery;
• automatic image registration for longitudinal tracking and inter-modality image comparison;
• images taken in different modalities or on different dates can be overlaid for comparison.
Dr. Sadda says that in his experience, several features of the California are big steps forward. “One is that the Optos wide-field platform now has indocyanine green angiography capability,” he explains. “ICG is important for identifying certain conditions such as polypoidal choroidal vasculopathy, a type of choroidal neovascularization. One of the things that we’ve learned from using ultra-wide-field ICG for this purpose is that the lesions can be quite large and extend quite a ways, even past the posterior poles. We also use ICG to aid in the diagnosis and management of patients with central serous chorioretinopathy. Using ultra-wide-field ICG on my patients with CSR, I’ve discovered that the choroidal vascular disturbance and hyperpermeability can be quite extensive. This has given us new insights into that disease.”
Dr. Sadda believes the most significant application for wide-field ICG, especially in the United States, is for the evaluation of uveitis and inflammatory diseases. “ICG can highlight a number of lesions that you can’t see with other imaging modalities because they tend to be deep lesions or affect the choroid in particular,” he explains. “Having ultra-wide-field ICG is great because inflammatory diseases that affect the choroid tend to affect the entire retina and extend far beyond the posterior pole. Those are areas we were not able to access before.”
Addressing Technical Problems
Dr. Sadda is also impressed that Optos has figured out how to manage the peripheral distortion that’s present in retinal images. “Any fundus camera will have this distortion,” he notes. “It can become particularly noticeable in a wide-field fundus camera, and it’s not easy to correct for the distortion so that you can get accurate measurements from the images. I run an image-reading center, so things related to image quality and measurements are pretty important.
“Optos claimed to have resolved this problem with this instrument, so we put it to the test,” he continues. “We did a project that we published in Ophthalmology a few months ago,1 in which we used patients who had been implanted with the retinal chip prosthesis—an electronic implant that’s put on the retina in blind patients with retinal degenerations to help them see. We chose these patients because that chip is of a known size, making it possible to use it as a ruler inside the eye.
|
“The California instrument also addresses another common problem with wide-field images: It’s harder to see the details in the superior and inferior aspects of the image,” he says. “The image kind of fades away a bit. In the past we’d compensate for this by having the patient look up or down and take another image. Now we don’t often do that, because the California device optimizes and maintains the resolution out to the periphery, especially superiorly and inferiorly.”
Dr. Sadda also likes that the California makes it easy to correlate findings between the different modalities it offers. “We’ve had a few patients in whom we’ve done a fluorescein angiogram and ICG simultaneously,” he explains. “The instrument doesn’t do them at exactly the same time; it alternates the flashes to get them. But they’re so close in time that it makes it easier to correlate findings between the two modalities.” REVIEW
Dr. Sadda has served as an advisor and consultant to Optos, as well as other imaging companies. His reading center has received research support to support the analysis of images collected in trials and other projects related to retinal imaging. Prof. Lanzetta has no financial interest in any technology cited in this article.
1. Sagong M, van Hemert J, Olmos de Koo LC, Barnett C, Sadda SR. Assessment of accuracy and precision of quantification of ultra-widefield images. Ophthalmology 2015;122:4:864-6.
doi: 10.1016/j.ophtha.2014.11.016. Epub 2015 Jan 8.