The Epithelium Factor
Dan Z. Reinstein, MD, adjunct professor of ophthalmology at Columbia University Medical Center in New York City, and medical director at the London Vision Clinic in the U.K., notes that although the current Food and Drug Administration approval of topography-guided ablation in the United States only allows very limited use of the technology, many surgeons are anxious to use it to treat unhappy patients who have previously undergone refractive surgery. Dr. Reinstein points out that getting the best possible result in these patients can be complicated by the impact of epithelial masking, which evens out small irregularities. For that reason, he and his colleagues are working on performing ablations based on the stromal surface instead of the epithelial surface measured by corneal topography. The refractive results appear to be improved in some eyes.
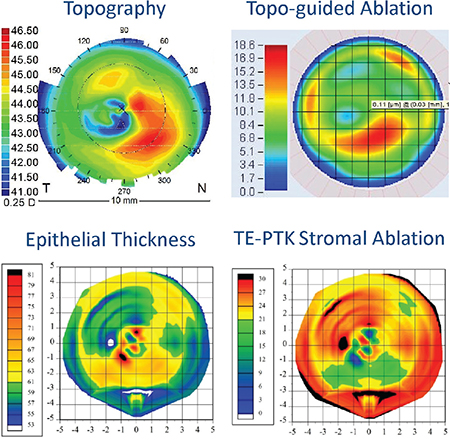 |
| Basing an ablation on the stroma can make a significant difference in the outcome. In this example a patient had an injury to the right eye resulting in a central scar. The front surface topography (top left) is irregular; the topography-guided ablation profile (top right—not including any refractive error correction) indicates that the majority of the ablation should be done in an inferior zone. However, the epithelial thickness map (bottom left) shows that the epithelial thickness is also extremely irregular, as it is partially compensating for the irregularities on the stromal surface; the epithelium varies from 53 to 82 µm (a range of 29 µm) within a 1-mm zone centrally. The map of the predicted stromal tissue removal for a trans-epithelial PTK treatment (bottom right) indicates that the maximum ablation needs to be slightly supero-temporal. The major irregularity on the stromal surface has been completely hidden from the front surface by the epithelium, and would therefore not be included in a topography-guided ablation. (Image: Dan Z. Reinstein, MD) |
Dr. Reinstein explains that the degree of epithelial compensation present on the cornea is defined by the curvature gradient of the stromal surface.3,4 “This explains why a topography-guided treatment works well for decentrations and small optical zones,” he says. “The majority of those kinds of irregularities will be detectable by topography. This also explains why topography-guided treatments don’t work in cases where the irregularity is localized (i.e., the curvature gradient is very high), and in some cases can actually make the situation worse: The epithelium will have compensated for the majority of the irregularity, hiding it from front-surface corneal topography. In these cases, a trans-epithelial phototherapeutic keratectomy procedure is much more effective, as it uses the epithelial thickness profile as a natural masking agent to focus the ablation onto the peaks in the stroma.”5,6
Dr. Reinstein notes that surgeons are limited by the manufacturer regarding which topographer they can use to gather the data, but he says it’s always important to obtain a corneal tomography scan to map the back surface of the cornea and corneal pachymetry profile. “It’s also vital that an epithelial thickness map be obtained in order to appreciate the topography of the stromal surface,” he says. “Epithelial thickness maps can be obtained using OCT or VHF digital ultrasound.”
Dr. Reinstein says his group recently described the first case where the ablation profile was calculated based on the stromal surface topography.7 “Paola Vinciguerra, MD, and colleagues are also working in this area using their custom phototherapeutic keratectomy approach, where they treat based on topography scans after removing the epithelium,” he notes.8 “If there are irregularities on the front corneal surface, the irregularities on the stromal surface will always be more severe due to epithelial masking—and it’s the stromal surface that we actually need to regularize.”
Taking Everything into Account
Arthur Cummings FRCSEd, a consultant ophthalmologist at Wellington Eye Clinic in Dublin, Ireland, notes that the advantages of a topography-guided treatment may soon be overshadowed by systems that also incorporate ray tracing. (Ray tracing is a way to use mathematics to predict how light will move as it passes through different media and strikes different surfaces. Using this technique, a computer can perform very complex analyses of a physical system such as an eye, modeling the impact of different conditions on light transmission and focus. Products currently incorporating this type of technology include Tracey Technologies’ iTrace Visual Function Analyzer.)
“Topography-guided treatments regularize the cornea, but we still have to do some work to figure out how the ablation is going to affect the refraction,” explains Dr. Cummings. “With ray tracing technology, you don’t have to do any of that; the technology does it for you.
“When performing wavefront-optimized or wavefront-guided treatments, no matter how clever our diagnostics and compensations are, the laser thinks it’s treating an eye that’s 24 mm long and has a corneal curvature of
43 D,” he continues. “If the treatment is topography-guided, the laser knows exactly what the cornea looks like, and that’s an improvement. But it still doesn’t know where the lens is sitting or the length of the eye. So we do our treatments, but occasionally we get surprises. We get surprises because using that model to plan every treatment, with its assumptions about the dimensions of the eye, doesn’t make sense.
“Ray tracing technology measures the eye’s wavefront, topography and biometry,” he continues. “So you now have measurements along the central axis and the line of sight, all the way through the eye. The laser knows the exact location of the front and back of the lens and where the retina is. It knows, for example, that this particular eye is 28 mm long, not 24 mm. It knows where the lens is; it may be more posterior than the other models assume.
Using that information, the software creates a virtual model of the eye and uses it to plan the treatment.
“Next, the software performs a virtual treatment on the virtual eye,” he says. “Once it has reshaped the virtual cornea, it projects an image into the virtual eye to see how well the rays are converging. If the rays all converge perfectly on the macula, that’s the basic ablation profile. However, most of the time the initial treatment plan doesn’t end up with the rays perfectly focused. So, the software works backwards, deducing how to adjust the
treatment so the rays will all end up correctly focused. It repeats this process until the virtual outcome is perfect, and the light coming into the virtual eye is well-focused on the fovea.”
Dr. Cummings says the software does one additional thing that increases the accuracy even more. “An ablation can cause epithelial and biomechanical changes,” he says. “Those changes are pretty well described in the literature.
So, the ray tracing algorithms include what is expected in terms of epithelial healing and biomechanical response and take that into account in the final treatment plan. This is all fine-tuning, but it’s the ultimate level of fine-tuning, where you’ve thought of everything and you’re making far fewer assumptions about the eye.
“So, I believe there is something beyond topography-guided ablation,” he concludes. “Topography-guided lasers are fabulous tools, but we can still get refractive surprises. We’re hoping that ray tracing will take care of those refractive surprises because it’s planning the treatment using the actual measurements of the patient’s eye, instead of approximations.
“Alcon is working on this technology right now,” he adds. “I think it will become available within the next couple of years.”
Dr. Reinstein is a consultant to Carl Zeiss Meditec. Dr. Cummings is a consultant to Alcon Laboratories and Wavelight.
1. Reinstein DZ, Archer TJ, Gobbe M. Combined corneal topography and corneal wavefront data in the treatment of corneal irregularity and refractive error in LASIK or PRK using the Carl Zeiss Meditec MEL80 and CRS Master. J Refract Surg 2009;25:503-515.
2. Reinstein DZ, Yvon C, Carp GI, Archer TJ, Gobbe M, Miller EA. Optical zone enlargement and recentration after previous myopic LASIK using topography-guided custom ablation. ESCRS 2015. Barcelone, Spain, 2015.
3. Reinstein DZ, Archer TJ, Gobbe M. Rate of change of curvature of the corneal stromal surface drives epithelial compensatory changes and remodeling. J Refract Surg 2014;30:800-802.
4. Vinciguerra P, Roberts CJ, Albe E, Romano MR, Mahmoud A, Trazza S, Vinciguerra R. Corneal curvature gradient map: A new corneal topography map to predict the corneal healing process. J Refract Surg 2014;30:202-207.
5. Reinstein DZ, Archer TJ, Gobbe M. Improved effectiveness of trans-epithelial phototherapeutic keratectomy versus topography-guided ablation degraded by epithelial compensation on irregular stromal surfaces [plus video]. J Refract Surg 2013;29:526-533.
6. Reinstein DZ, Archer TJ, Dickeson ZI, Gobbe M. Trans-epithelial phototherapeutic keratectomy protocol for treating irregular astigmatism based population on epithelial thickness measurements by Artemis very high-frequency digital ultrasound. J Refract Surg 2014;30:380-387.
7. Reinstein DZ, Gobbe M, Archer TJ, Youssefi G, Sutton HF. Stromal surface topography-guided custom ablation as a repair tool for corneal irregular astigmatism. J Refract Surg 2015;31:54-59.
8. Vinciguerra P, Camesasca FI. Custom phototherapeutic keratectomy with intraoperative topography. J Refract Surg 2004;20:S555-563.



