D-Eye
The D-Eye Portable Retinal Imaging System (D-Eye, Padova, Italy) is a lens assembly that magnetically attaches to a late-model Apple iPhone or Samsung Galaxy.
Andrea Russo, MD, a practicing ophthalmologist and PhD candidate at Italy’s University of Brescia, invented the D-Eye. “About 20 years ago, they joined digital cameras with PCs in order to record the view of the retina in our offices,” Dr. Russo says. “Now, we have the smartphone, which is a computer in your pocket. When I finished my residency program, I decided to use a few lenses to create the D-Eye project. Essentially, the D-Eye is a direct ophthalmoscope for viewing the retina using just a smartphone held close to the patient’s eye.”
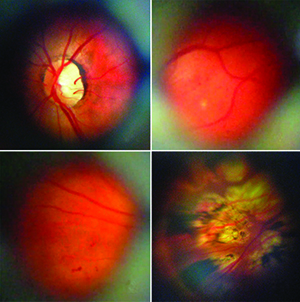 |
| A collage of retinal images captured with the new D-Eye system. (Image courtesy Andrea Russo, MD.) |
In practice, Dr. Russo says the field of view is limited. “It’s around 5 to 8 degrees with an undilated pupil, and 20 to 25 degrees with dilation,” he says. “This is because direct ophthalmoscopy is similar to looking through a keyhole, and the wider the keyhole, the wider the field of view. It really depends on the pupil’s dimensions.
“You can record still images or videos with it,” Dr. Russo continues, “but I suggest recording video, since you have a limited field of view. In video mode, you can pan around the retina, from the fovea to the optic disk, then out to the equator, to catch all the details. Otherwise, if you only use still images, you could lose a few parts of the retina. You can’t go farther than the equator, but you can reach it as you can with an ordinary direct ophthalmoscope.”
Dr. Russo says that, though the device is useful, it’s not a substitute for a traditional retinal camera and direct ophthalmoscopy. “The traditional system is the next level,” he says. “The D-Eye system is in the middle between direct ophthalmoscopy and high-end, expensive cameras. This isn’t intended to be a substitute for traditional equipment, but instead to help with exams in specific cases, such as bedridden patients, patients in rural areas and babies. In terms of conditions, it’s good for glaucoma screening because the optic nerve is easy to view. For diabetic retinopathy, you can assess the retina out to the periphery and notice signs of diabetic retinopathy. We actually published a paper this year that described the agreement between the D-Eye system and the ordinary slit-lamp exam in diabetic retinopathy that found that the agreement was pretty good.”1
Future plans for the device are aimed at overcoming the current version’s limitations. “We’re developing a D-Eye 2.0 with a much wider field of view,” Dr. Russo explains. “Since, as I said earlier, direct ophthalmoscopy is like looking through a keyhole, the closer you get to the keyhole, the wider the field of view, so the solution is to make the D-Eye slimmer. This one is about 1 cm, and the 2.0 will be 0.5 cm.”
The D-Eye costs $390. Also, when a new version comes out, Dr. Russo says all the user will need to purchase is the housing that attaches to the phone, not an entirely new D-Eye lens system. For information, visit d-eyecare.com.
OphthalmicDocs Fundus
The OphthalmicDocs Fundus is born out of the open-source movement in software, which allows users to take a product, in this case an adapter for a smartphone, and modify it in ways they see fit. As such, the OphthalmicDocs adapter isn’t something you buy; instead it’s a file you can download and send to a 3D printer, creating it yourself for the cost of the printing and materials. You add a condensing lens and then attach the device to your smartphone.
The idea for the device came from Hong Sheng Chiong, MD, an ophthalmology registrar (similar to a resident in the United States) at Gisborne Hospital in New Zealand. At first, his idea was limited to drawings on paper, but when he co-founded OphthalmicDocs he teamed up with product designers and engineers, and the device began taking shape.
 |
| The OphthalmicDocs Fundus is inexpensive because you make it on a 3D printer. (Image courtesy Hong Sheng Chiong, MD.) |
“We’ve been mainly using it locally in our hospital for patients who present to the emergency department, those too sick to be sent down to the eye clinic, and for neonatal examinations,” says Dr. Chiong. “Because we’re on the east coast of New Zealand, it’s an outreach area, and we have small villages of 500 to 1,000 people who live two hours away from the nearest health-care center. In that type of situation, it’s useful for screenings for patients who require a retinal exam. It’s also handy in an outreach environment because a conventional fundus camera would be too heavy and bulky to move around, and could be damaged by the rough road conditions.”
Dr. Chiong says that, though the adapter is useful in certain situations, it has some limitations, as well. “The strength of the system is that it’s portable,” he says. “But, like any portable, handheld device, if you try to take a video and there’s movement, it will degrade the image quality. The best way to get a good image is to have the patient sit down, and then stabilize the patient’s head with one hand while holding the smartphone with the other.
“The pupil size is a huge factor in getting images with the current version of the device,” Dr. Chiong continues. “Cases that are challenging for the retinal adapter are patients that don’t have a pupil that’s easily dilatable. It’s challenging in floppy-iris syndrome, for example. Also, like any other fundus camera, it doesn’t give you a 3D perception of a lesion, just 2D, so you can’t be sure if it’s elevated or not.”
Future plans center on making the system non-mydriatic. “We’re working on a non-mydriatic adapter with a wider field of view,” says Dr. Chiong. “You could actually have up to a 50-degree field of view by incorporating a small, powerful lens after the objective lens and using an infrared light source to get focus to prevent pupillary constrictions.”
The 3D printer file can be downloaded at ophthalmicdocs-fundus.org, along with instructions on assembly. If you don’t have access to a 3D printer, you can find one near you by visiting 3Dhubs.com.
PEEK Retina
A smartphone solution for retinal imaging that’s being used for research outside of the United States is the Portable Eye Examination Kit Retina.
PEEK Retina consists of an adaptor that slides over the top portion of a smartphone, interfacing with the phone’s camera, and a software application for focusing the retinal image and organizing the videos and images that the camera captures.
The PEEK system has been used for retinal screening in low-income communities in Kenya, for diabetic retinopathy detection in Botswana and for screening patients for possible malarial retinopathy in Mali. PEEK’s designers are also working on incorporating eye tests into the system to allow physicians in the field to perform quick eye exams to get a baseline for a patient’s acuity. In the future, PEEK will also have color testing to screen for color-blindness and contrast sensitivity testing.
In terms of availability, it looks like PEEK will arrive in Europe first. “We are currently in the manufacturing stage, and aim to have the PEEK Retina adapter available in early 2016,” explains PEEK’s Sarah O’Regan. “We should be able to ship it within the European Union—and to non-governmental organizations within the EU who will be responsible for export. We hope to be able to ship to as many countries as possible, and are working with a regulatory consultant on this. We’re currently unable to ship PEEK Retina to addresses in the United States until FDA approval has been granted, but we are working on this.” For more information or to possibly get involved with PEEK research, visit peekvision.org. REVIEW
Dr. Russo sold the patent for the D-Eye and is an adviser to the company. Dr. Chiong is co-founder of the charitable trust OphthalmicDocs, which doesn’t charge for the adapter or app.
1. Russo A, Morescalchi F, Costagliola C, Delcassi L, Semeraro F. Comparison of smartphone ophthalmoscopy with slit-lamp biomicroscopy for grading diabetic retinopathy. Am J Ophthalmol 2015;159:2:360-4.




