|
Higher-order Aberrations
Surgeons say one of the top benefits topography and tomography systems offer them is the ability to catch irregular astigmatism, represented by higher-order aberration data, that would diminish the presbyopic IOL’s ability to work well.
“It’s important to remember that the corneas of your patients aren’t always perfect,” says Naoyuki Maeda, MD, Phd, of Japan’s Osaka University Graduate School of Medicine. “Even if a cornea looks perfectly clear, it might have irregular corneal astigmatism due to undetected keratoconus, a very faint scar or mild pterygium. This faint scar or mild distortion can result in irregular astigmatism that’s not appropriate for the use of a multifocal IOL.” Devices useful for higher-order aberration, a.k.a., irregular astigmatism, measurement include the Oculus Pentacam, which measures corneal irregular astigmatism; and the Topcon KR-1W and Nidek OPD-Scan, which separate out lenticular and corneal higher-order aberrations. The Zeiss-Humphrey Atlas also provides data on corneal HOAs using ray tracing. “Higher-order aberrations are the enemy of the multifocal IOL,” says Dr. Maeda. “The MF IOL divides light into far and near so, even with a perfect cornea, image contrast is reduced to some extent. The HOAs also cause image contrast to worsen in some situations.”
To help determine if a patient has too much irregular astigmatism that might make a MF IOL unworkable, Dr. Maeda developed a numerical HOA cutoff based on the pupil diameter. “At a 4-mm diameter, 0.3 µm of HOA is similar to the blur produced by 0.5 D of defocus,” he says. “And I think that a defocus, or spherical error, of 0.5 D following cataract surgery is clinically significant, so any HOAs more than 0.3 µm should make the surgeon worry. This number is just based on my experience, and hasn’t been proven in a clinical study, and people may say it’s kind of strict. However, I raised the bar just to be safe. I selected a pupil diameter of 4 mm because a patient’s daytime pupil is around 3 to 4 mm, so I thought it was an appropriate size.”
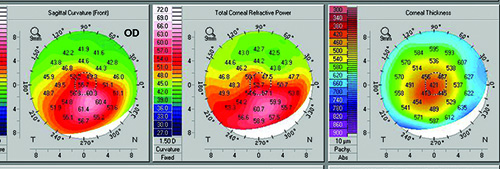
Stephen Klyce, PhD, adjunct professor of ophthalmology at New York’s Mount Sinai School of Medicine, says the pupil size and corneal aberrations are key to understanding how a patient may see with a multifocal IOL; he has developed a way to simulate the patient’s vision based on the aberrations at various pupil sizes. “When a patient’s aberrations are represented visually, you’ll often see point-spread functions, modulation transfer functions, Zernike polynomial terms and other optical transforms that most clinicians cannot understand,” Dr. Klyce says. “You can’t understand from such data how well the patient is seeing. We take the corneal distortions from corneal topography and convolve them with a Snellen eye chart. Then, clinicians as well as their patients can understand how well a patient should see with glasses.”
|
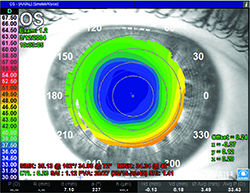
Scott MacRae, MD, professor of ophthalmology at the University of Rochester Medical Center in New York, says that, when using the Orbscan II topographer, certain maps are preferable to others. “I like instantaneous curvature and tangential maps better than axial,” he avers. “Axial maps involve more averaging and you get less local information in terms of local irregularities. The instantaneous map gives you finer detail in terms of the local curvature changes—or local irregularities—that are occurring. The Orbscan also provides an irregularity index for certain pupil sizes. Anything less than 1.5 on the irregularity index is reassuring.”
Abnormal Shape
Surgeons say a cornea can have minimal irregular astigmatism but still have an abnormal shape that will hinder a multifocal lens, as occurs in post-refractive surgery patients.
“Everyone knows that it’s very difficult to determine IOL power after refractive surgery with LASIK,” says Dr. Maeda. “If a patient has an abnormal corneal shape, even if the cornea doesn’t have irregular astigmatism, such as occurs after LASIK, it’s very difficult to minimize post-cataract surgery refractive errors. However, in these premium lens patients, surgeons want to select patients in whom they can easily minimize the postoperative refractive error. To identify the shape characteristics, check for an abnormal corneal shape using the tomographer’s axial power map qualitatively and the sagittal front-back ratio quantitatively. In our clinic, we’ve found that 3 percent of our patients have what would be considered an abnormal corneal shape.” Dr. Maeda cautions that postop refractive errors in ultrasound measurements are usually larger than those produced by optical devices such as the IOLMaster and LenStar.
Corneal Spherical Aberration
Since aspheric is the platform of choice for multifocal IOLs, surgeons say it pays to get a handle on the patient’s spherical aberration. If the SA falls outside a certain number, the patient might be better with another sort of lens.
“The first generation of ReSTOR lens was a spherical IOL,” Dr. Maeda explains. “However, this wasn’t optimized, so Alcon changed it to an aspheric configuration. Major MF IOLs use an aspherical shape as their platform to reduce the spherical aberration. At the 6-mm zone, in general the spherical aberration of patients of European descent is +0.27 µm, so the aspheric IOL has -0.2 or -0.27 to compensate for it.
“When evaluating the IOL candidate,” Dr. Maeda continues, “if he has a negative spherical aberration value, we shouldn’t use an aspheric intraocular lens, but instead a spherical one. Therefore, I’ve set a cutoff of 0.1-µm RMS or higher for acceptability for use of an aspheric, multifocal lens. The acceptable range for a spherical lens is less than 0.1-µm RMS. I don’t have any clinical study evidence that these cutoff values are correct, but theoretically I believe them to be useful values when making preoperative assessments. For instance, the ReSTOR IQ has a -0.2-µm RMS. So if the patient has SA of 0.1, this would create a SA of -0.1, so it makes sense as a cutoff value in this case. At our practice, we’ve found abnormalities in SA in 11 percent of our patients.”
K Readings
|
“If a patient has any irregularity of the corneal surface or has had refractive surgery—and refractive surgery is old enough now that these cases are coming in in droves—traditional keratometry won’t work well,” advises Dr. Klyce. “We published a paper years ago regarding the disparity of keratometry readings and corneal power within the diameter of the pupil after refractive surgery. Keratometers measure at a 3- or 4-mm diameter on the corneal surface, and will miss any curvature changes within the central cornea. One needs to measure the corneal astigmatism and aberrations over the pupil rather than at the periphery. Typically, for intraocular lens calculations, one uses a topographic value called Average Corneal Power, rather than keratometry. ACP gives a much better estimate of the corneal power and cylinder of the part of the cornea actually used for vision. ACP is a value provided on Nidek topographers as well as on other topographers, tomographers and OCT-based instruments, where it may be called by other names.
“As an example of its usefulness,” Dr. Klyce adds, “the ASCRS IOL calculator, created by Warren Hill, MD, Li Wang, MD, PhD, and Doug Koch, MD, for eyes that have undergone refractive surgery (iolcalc.org) has a numerical field requiring the input of one of these variables.” Dr. Klyce says the online calculator is a major advance for optimizing refractive cataract surgery.
Dr. Maeda says a tomographer can help determine how much cylinder needs to be corrected for maximum effect from a toric or multifocal-toric intraocular lens. “It depends on the surgeon, but most surgeons agree that regular astigmatism should be kept below about 1 D postop,” he says. “On the other hand, the toric intraocular lens is more expensive. We need to determine the value of the astigmatism, though I think most surgeons will agree that any cylinder value of 1.5 D or more should be corrected for a lens to have its optimum effect.”
When the readings from the keratometer and those generated by the topographer disagree on the magnitude and/or axis of astigmatism in a post-refractive surgery patient, Dr. MacRae says that he will err on the side of his topography readings. “In such cases I would tend to use the results from the topographer,” he says, “especially if the result is reproducible. This is because the keratometer is user-dependent, and so it’s not as objective a reading as one gets from an automated system such as the corneal topographer. However, such a discrepancy could be another warning sign to the cataract surgeon that there’s some irregularity of the surface as a result of dry eye, so you’d want to repeat the topography and look for consistency with that. Though it’s true you can instill artificial tears, the fact is if you frequently have to put in artificial tears just to get a good image for a particular patient, that’s an indication that you either have to work with the patient to try to get the surface irregularity eliminated on a more sustained basis before the surgery or that you have to shy away from implanting a multifocal lens in that patient. This is because if the patient’s ocular surface is becoming irregular, the combination of an irregular surface and a multifocal IOL can reduce image quality, resulting in an unhappy patient.” REVIEW