Experience with these modern imaging devices has truly changed the way ophthalmologists evaluate the vitreous, retina and choroid and has led to more understanding of the role of the peripheral pathology in uveitis.
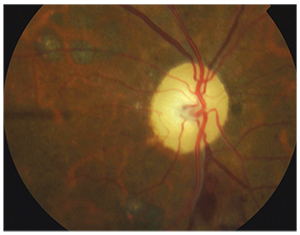 |
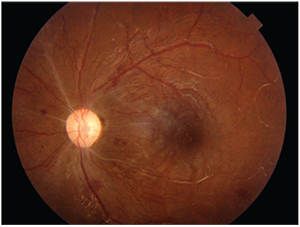
| Figure 1. 20-degree field of view. Color fundus photograph of an eye post retinal laser photocoagulation due to retinal vein occlusion associated with Behçet’s disease. There is optic nerve pallor, intraretinal hemorrhages and laser spots. |
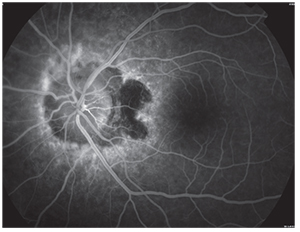 |
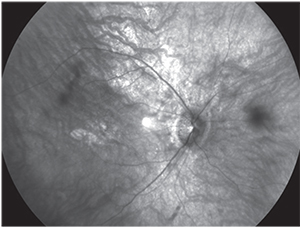
| Figure 2. 35-degree field of view. Fundus fluorescein angiography showing peripapillary staining and blockage from choroidal neovascularization in an eye with presumed ocular tuberculosis. |
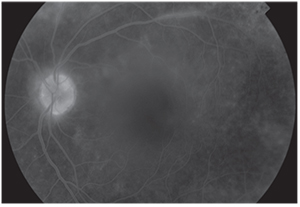 |
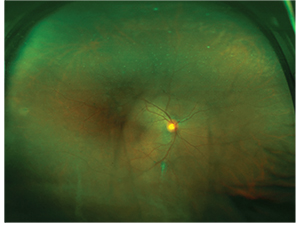
| Figure 3. 50-degree field of view. Fundus fluorescein angiography showing mild optic disc and retinal pigment epithelium staining and vascular sheathing in an eye with idiopathic retinal vasculitis. |
 |
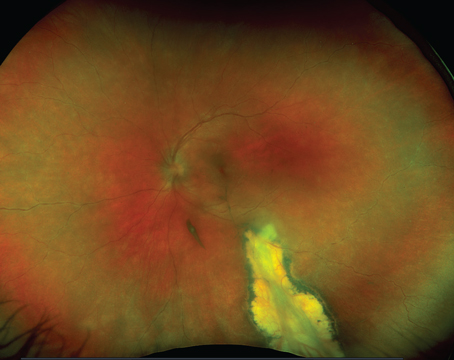
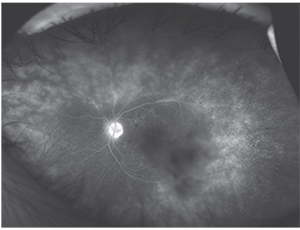
| Figure 4. 80-degree field of view. Color fundus photograph of an eye with lupus retinopathy showing sclerotic retinal arteries, intraretinal hemorrhages and macular deposits. Fundus fluorescein angiography demonstrated central retinal artery occlusion. |
Standardized imaging protocols were employed in some early clinical trials and research studies. The Diabetic Retinopathy Study used a protocol consisting of seven standard 30-degree photos for acquisition of images of the retinal periphery in a systematic manner. The width of these composite images in this protocol is approximately 75 degrees. Photographs anterior to the equator can be obtained with this protocol by tilting the camera, but they will not image farther peripheral structures.3 This protocol was extended to a nine standard-field protocol for the Longitudinal Studies of Ocular Complications of AIDS (L-SOCA) protocol to image both active and inactive peripheral cytomegalovirus retinitis. Per specifications of the Fundus Photography Reading Center at the University of Wisconsin, retinal cameras approved for this procedure had 50-degree or 60-degree magnification settings.
Such photography, however, may be limited by patient alignment problems, focusing irregularities, marginal corneal astigmatism, poor fixation and light reflex artifacts.4
Since then, numerous advances have been made that permit visualization of the retinal periphery in a practical manner. The Retcam (Clarity Medical Systems) is a contact-based, wide-angle camera system with a 130-degree field of view.5 The system is particularly well-suited for imaging pediatric patients because it is portable and can be placed directly just over the eyes of patients who are unable to position themselves, such as neonates and infants.
Reflection of light from interfaces in the ocular media is a major cause of artifacts with any fundus imaging. Confocal scanning laser ophthalmoscopy, which separates the illuminating and imaging beam within the eye, eliminates these reflections.4 Giovanni Staurenghi, MD, and colleagues developed a combined contact and noncontact handheld lens system coupled with SLO. The Staurenghi lens system obtains high-resolution images with a 150-degree field.6
The Optos 200Tx (Optos) is a UWF imaging system that produces a 200-degree view depending on the definition of the geometric center of the retina. The Optos technology utilizes a combined SLO with an ellipsoidal mirror to obtain pictures of the peripheral retina with one capture without the need for bright illumination lighting or a contact lens, and in some patients, pupillary dilation. The system provides the ability to capture red and green reflectance imaging, as well as fundus autofluorescence and fluorescein/indocyanine green angiography.7
Wide-field imaging of the vitreous is now possible with the introduction of a biomicroscopic wide-angle retinal and vitreous observation system utilizing a three CCD (charge-coupled devices) video camera and a personal computer for image display.8 Optical coherence tomography technology is expanding toward examining wider areas of the retina. The systems have now expanded from 30 degrees to 55 degrees (Heidelberg Spectralis system, Heidelberg Engineering). With moving of the scan towards periphery, some areas can be visualized that were previously unreachable for OCT imaging.9
Uveitis
 |
| Figure 5. 100-degree field of view. Red-free fundus photograph of an eye with unknown retinal dystrophy and inflammatory reaction in the cortical vitreous. |
 |
| Figure 6. 150-degree field of view. Color fundus photograph of an eye with intermediate uveitis showing vitreous debris. The patient had a positive Quantiferon test for tuberculosis. |
 |
| Figure 7. 200-degree field of view. Ultra-widefield fundus fluorescein angiography of an eye with idiopathic retinal vasculitis (the same eye as Figure 3). The image demonstrates mild optic disc staining, staining and stippling of the retinal pigment epithelium and vascular sheathing. |
Marina Mesquida, MD, MSc, PhD, and colleagues assessed the role of UWF retinal imaging in the diagnosis and management of retinal vasculitis associated with Behçet’s disease.14 They found that UWF retinal imaging had allowed documentation of peripheral retinal lesions and greatly simplified longitudinal comparisons for disease activity and progression. In their study, peripheral vein sheathing and retinal infiltrates that denote disease activity were clearly detected with UWF pseudocolour imaging. UWF fluorescein angiography was a very helpful tool in their patients for determining whether the vasculitis had an occlusive nature and for quantifying the true extent of the capillary non-perfusion. Areas of retinal ischemia and neovascularization were easily identified in their series, aiding in the decision for targeted laser photocoagulation. Their observations also suggested that active retinal vasculitis in patients with Behçet’s disease may induce retinal epithelium alterations in the retinal periphery. These abnormalities were visible with UWF fundus autofluorescence as multiple hyperfluorescent spots in the retinal periphery.14
UWF indocyanine green angiography has been shown to produce high-resolution images of both the central and peripheral choroidal vasculature.15 Wide-field ICG may also be invaluable in the diagnosis and monitoring of some uveitic entities.
Future Directions
There have been significant improvements in imaging the peripheral retina over the past years. UWF technology has become important clinically with regards to early diagnosis, effective treatment and monitoring of posterior uveitis. We expect that wide-field imaging will be used to extend and/or modify certain morphologic classifications of posterior uveitis phenotypes. It will be widely used in clinical research and maybe in some clinical trials. In addition, we can expect incorporation of UWF retinal imaging in the field of telemedicine. Recently, a novel portable handheld smartphone-based retinal camera capable of capturing high-quality, widefield fundus images was developed. The use of the mobile phone platform creates a fully embedded system capable of acquisition, storage and analysis of fundus images that can be directly transmitted from the phone via wireless telecommunication system for remote evaluation.16 A significant amount of work is going on to validate and expand the utilization of UWF imaging. We believe that UWF imaging technology will be indispensable for the routine uveitis practice in the near future. REVIEW
Dr. Kozak is a senior academic consultant in the Vitreoretinal and Uveitis Division, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia. Dr. Nguyen is a professor and chairman at the Truhlsen Eye Institute, University of Nebraska Medical Center, Omaha, Neb. Contact Dr. Kozak at King Khaled Eye Specialist Hospital, Box 7191, Riyadh 11462 Saudi Arabia. Phone: +96614281234 ext. 3772; e-mail: ikozak@kkesh.med.sa.
1. Tan CS, Sadda SR, Hariprasad SM. Ultra-widefield retinal imaging in the management of diabetic eye diseases. Ophthalmic Surg Lasers Imaging Retina 2014 Sep 1;45(5):363-6.
2. Pang CE, Shah VP, Sarraf D, Freund KB. Ultra-widefield imaging with autofluorescence and indocyanine green angiography in central serous chorioretinopathy. Am J Ophthalmol 2014 Aug;158(2):362-71.e2. doi: 10.1016/j.ajo.2014.04.021.
3. Diabetic retinopathy study. Report Number 6. Design, methods, and baseline results. Report Number 7. A modification of the Airlie House classification of diabetic retinopathy. Prepared by the Diabetic Retinopathy, et al. Invest Ophthalmol Vis Sci 1981; 21(1 Pt 2):1–226.
4. Kaines A, Oliver S, Reddy S, Schwartz SD. Ultrawide angle angiography for the detection and management of diabetic retinopathy. Int Ophthalmol Clin 2009 Spring;49(2):53-9.
5. Roth DB, Morales D, Feuer WJ, Hess D, Johnson RA, Flynn JT. Screening for retinopathy of prematurity employing the Retcam 120: Sensitivity and specificity. Arch Ophthalmol 2001;119: 268-72.
6. Staurenghi G, Viola F, Mainster MA, Graham RD, Harrington PG. Scanning laser ophthalmoscopy and angiography with a wide-field contact lens system. Arch Ophthalmol 2005;123: 244-52.
7. Witmer MT, Parlitsis G, Patel S, Kiss S. Comparison of ultra-widefield fluorescein angiography with the Heidelberg Spectralis noncontact ultra-widefield module versus the Optos Optomap. Clin Ophthalmol 2013;7:389-94.
8. Lee BR, Chang HR. Biomicroscopic vitreous observation using a 3 CCD video camera and a personal computer for image capture and archiving. Korean J Ophthalmol 2000;14:74-9.
9. Gregori NZ, Lam BL, Gregori G, et al. Wide-field spectral-domain optical coherence tomography in patients and carriers of X-linked retinoschisis. Ophthalmology 2013;120:169-74.
10. Campbell JP, Leder HA, Sepah YJ, et al. Wide-field retinal imaging in the management of non-infectious posterior uveitis. Am J Ophthalmol 2012;154:908-11.
11. Gupta V, Al-Dhibi HA, Arevalo JF. Retinal imaging in uveitis. Saudi J Ophthalmol 2014 Apr;28(2):95-103.
12. Seidensticker F, Neubauer AS, Wasfy T, Stumpf C, Thurau SR, Kampik A, et al. Wide-field fundus autofluorescence corresponds to visual fields in chorioretinitis patients. Clin Ophthalmol 2011;5:1667-71.
13. Leder HA, Campbell JP, Sepah YJ, Gan T, Dunn JP, Hatef E, et al. Ultra-wide-field retinal imaging in the management of non-infectious retinal vasculitis. J Ophthalmic Inflamm Infect 2013 Feb 11;3(1):30.
14. Mesquida M, Llorenç V, Fontenla JR, Navarro MJ, Adán A. Use of ultra-wide-field retinal imaging in the management of active Behçet retinal vasculitis. Retina 2014;34:2121-7.
15. Klufas MA, Yusuf IH, Xur K et al. Feasibility and clinical utility of ultra-widefield indocyanine green angiography. Retina 2015;35:508-20.
16. Maamari RN, Keenan JD, Fletcher DA, Margolis. TPA mobile phone-based retinal camera for portable wide field imaging. Br J Ophthalmol 2014;98:438-41.