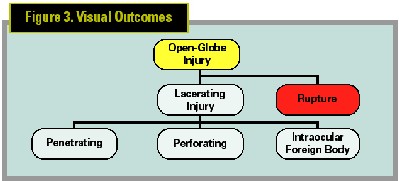
AN OPEN-GLOBE INJURY BY DEFINITION includes a full-thickness defect in the cornea and or sclera. Proper care for patients presenting with this type of injury requires a systematic approach to the diagnosis and management, but more than other ocular disease processes, managing the open globe calls for creativity and flexibility of surgical approach tailored to the specific case.
Open-globe injuries come in many varieties and are sub-classified based on the mechanism of injury. Blunt injury of significant force causes deformation changes of the globe with rapid rise in intraocular pressure. With anterior-posterior shortening of the eye, the eyewall undergoes significant strain and can rupture or burst at weak points.
| Table 1. Classifying Open-Globe Injury |
| Globe Injury |
| Type (mechanism of injury) |
| Rupture |
| Penetrating |
| Intraocular foreign body |
| Perforating |
| Combined |
| Grade (presenting visual acuity) |
| > 20/40 |
| 20/50 to 20/100 |
| 19/100 to 5/200 |
| 4/200 - Light Perception NLP |
| Pupil (RADP) |
| Positive, relative afferent pupillary defect present (RAPD) |
| Negative, RAPD not present |
| Zone (location of wound) |
| I. Cornea |
| II. Limbus to 5 mm posterior into sclera |
| III. Posterior to 5 mm from limbus |
 |
|
A ruptured globe. Extrusion of bloody |
Diagnosis
Clinical suspicion should be high for the possibility of an open-globe injury in all trauma cases. Direct particular attention to cases involving grinding or hammering, since these continue to be the most common cause of penetrating and intraocular foreign body (IOFB) injuries. Patients with a history of significant ocular and periocular blunt trauma should be considered ruptured until proven otherwise. The diagnosis of a ruptured globe can be difficult given the periocular and ocular swelling, and since the rupture often occurs under the rectus muscles, the wound may be occult.
When obtaining a history from patients, particularly children, one must be skeptical that the circumstances surrounding the injury may be falsified. More than once, I have taken part in the management of such injuries where the diagnosis was delayed with devastating implications. The delay in these cases was initiated because the patient was not forthcoming with the true nature of the injury.
Complete ocular examination is important when possible and should begin in all cases with measurement of the visual acuity and testing for the presence of a relative afferent pupillary defect. Poor presenting visual acuity and the presence of an afferent pupillary defect are the most significant prognostic factors that can be detected on presentation. It is important to document these factors for clinical and medical legal reasons.
Most open-globe injuries can be diagnosed with simple pen light or flashlight examination. Smaller wounds may require slit-lamp examination for confirmation, to rule out associated injury, intraocular foreign body and endophthalmitis. As mentioned, posterior rupture may be occult. Clinical signs of occult rupture include diffuse chemosis, asymmetric deepening of the anterior chamber, low intraocular pressure, hemorrhagic choroidal detachment and vitreous hemorrhage.
Fundoscopic examination should likewise be attempted in all trauma patients, however, in the severely injured eye, anterior and posterior segment opacities often limit visualization. In such cases, it is imperative that ancillary testing is carried out. The test of choice is the CT scan. Today, the CT scan is as easy to obtain in the emergency department as an EKG. It is a rapid, noninvasive test that provides information about the integrity of the globe, the presence of an IOFB, and the status of the orbital and facial bones. We found the CT scan to have reasonable sensitivity and specificity in the diagnosis of the open globe.
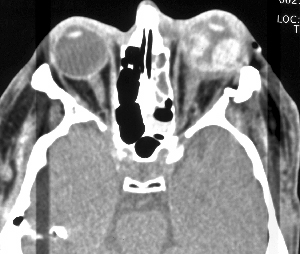 |
| CT scan confirms occult ruptured globe with evidence of hemorrhagic choroidal detachment and deepening of the anterior chamber. A discontinuity of the lateral eyewall at the insertion of the rectus muscle is present as well. |
Treatment
When the open-globe injury has been confirmed, a few questions need to be answered:
1. Does the wound require closure or is it self-sealing?
2. Is an IOFB present?
3. Are there signs of endophthalmitis?
Depending on the status of these questions most of the planning of timing and repair can be determined.
Self-Sealing and Non-Self-Sealing
Penetrating injuries resulting from lacerating force may be very localized, with the ideal lacerating wound being the carefully constructed surgical incision. In rare instances, a patient may experience a similar wound following trauma. When such a wound is present, careful inspection of the wound is necessary to confirm that indeed the wound is self-sealing. Seidel testing is carried out with and without gentle pressure. Passing such a test should circumvent the necessity of surgical intervention, assuming other ocular structures do not require immediate repair (i.e. dense cataract, IOFB, endophthalmitis).
In most cases traumatic wounds are not self-sealing and require surgical repair. The closure of the wound should be completed on an urgent basis (within 12 to 24 hours). Wounds at particular risk for infection such as contaminated wounds, IOFB-related injuries, rural injuries and lens injury associated open-globe injuries, require more emergent care. When delay in primary repair is anticipated, for example because of patient transport, prophylactic antibiotics should be administered as soon as possible.
When a wound is particularly large one must consider that delay in closure could increase not just the risk of infection but also the opportunity for an expulsive hemorrhage and extrusion of intraocular contents.
Intraocular Foreign Body Injuries
In the acute setting when an IOFB is confirmed, urgent intervention is necessary to reduce the risk of infection. Some cases of IOFB-associated Bacillus endophthalmitis may progress rapidly with irreversible damage and rapid loss of the eye. Remember, presence of an IOFB may increase the chance of traumatic endophthalmitis by two to 30 times, although a recent review of traumatic endophthalmitis failed to show IOFB as an independent risk factor for the development of post traumatic endophthalmitis.1 In the case of a chronic IOFB, the risk of endophthalmitis is negligible and removal of the IOFB is not emergent and based on associated injuries and the possibility of IOFB-related toxicity. The point at which the risk of acute endophthalmitis becomes low, so that emergent removal is not necessary has not been established.
Endophthalmitis following open-globe injury is much more common (10 to 100 times more common) than post-operative endophthalmitis. In many cases the signs of infection are present at the time of the initial examination but may take days to manifest. Infection is associated with rural injuries, dirty wounds (injuries caused by an object contaminated with soil or vegetable material), IOFBs, lens injury, and delay in wound closure. When suspected, emergent treatment is initiated with appropriate intravitreal antibiotics, with or without pars plana vitrectomy. The endophthalmitis vitrectomy study (EVS) did not address specifically endophthalmitis associated with open-globe injuries and extrapolating results from this study for the post-trauma case may be inappropriate. Many would advocate vitrectomy with intravitreal antibiotics instead of a less invasive approach with vitreous tap and intravitreal injection at the time of wound closure. However, this does not mean that it is inappropriate to close a wound and perform a vitreous tap and intravitreal injection of antibiotics without a complete vitrectomy.
The appropriate antibiotic prophylaxisis for cases of open-globe injury without presenting infection is controversial. Given the potential for infection, most advocate the use of topical as well as systemic antibiotics. In high-risk cases, some even recommend intravitreal prophylaxisis. Traditionally, prophylaxisis has required admission to the hospital for intravenous antibiotics. With the more recent advent of newer fluoroquinolones such as ciprofloxacin and gatifloxicin, therapeutic levels of the antibiotic can be achieved in the vitreous cavity following oral administration. Given these newer antibiotics, it is now not necessary that a patient be admitted solely for the administration of antibiotic prophylaxisis and it is appropriate to consider outpatient management of most open-globe injuries.
Outcomes
The most prognostic factors for poor visual outcome and the need for enucleation are poor presenting visual acuity and the presence of an afferent pupillary defect in the injured eye. We previously reported a simple system for classifying ocular injuries at the time of presentation and have shown it to be prognostic for visual outcomes in open-globe injury. There is however, no single factor or combination of prognostic factors, even no light perception vision (NLP), that precludes visual recovery. Following from this, we recommend attempted primary repair (closure of the wound) in all cases. Primary enucleation is considered in the rare instance of extreme tissue loss prohibiting anatomic closure. For the severely injured eye, determining the potential for visual recovery and salvaging the eye is paramount when deciding whether or not to proceed with secondary repair versus enucleation. In most cases, we recommend secondary repair even if the vision is NLP. A review of the United States Eye Injury Registry noted that nearly 13 percent of the cases presenting with NLP vision regained some vision during follow-up. The risk of proceeding with secondary repair of the very severely injured eye is that delay or deferral of enucleation may increase the risk of sympathetic ophthalmia (SO). SO is a consideration in all open-globe injuries and thorough discussion of the risks with the patient is necessary, but the incidence today appears to be extremely low. In the rare case that SO does develop, current treatment strategies are effective in the maintenance of good vision for most patients.
Dr. Pieramici is co-director of the California Research Foundation, 515 E. Micheltorena, Santa Barbara, Calif. Contact him at dpieramici@ yahoo. com.
1. Essex RW, Yi Qing, PG Charles, et al. Post-traumatic Endophahtlmitis. Ophthalmology 2004 ;111 :2015-2022.
2. Thompson JT, Parver LM, Enger CL, et al. Infectious endophthalmitis after penetrating injuries with retained intraocular foreign bodies. National Eye Trauma System. Ophthalmology 1993;100:1468-74.
3. Meredith TA. Posttraumatic Endophthalmitis. Arch Ophthalmol 1999;117:520-1.
4. Pieramici DJ, Sternberg P Jr, Aaberg TA, Bridges WJ. A System for Classifying Mechanical Injuries of the Eye. Am J Ophthalmol 1997; 123;820-31
5. Pieramici DJ, Au Eong KG, Sternberg P Jr, Marsh MJ. The prognostic significance of a system for classifying mechanical injuries of the eye (globe) in open-globe injuries. J Trauma 2003;54 (4):750-4.



