Hedging Against Herpes
Surgeons say a history of HSV keratitis is a relative contraindication for laser refractive surgery. Some feel, however, that with the proper evaluation and preparation patients with a history of HSV can have a good outcome.
The main risk surgeons are concerned about is reactivating the herpes, since case reports and animal studies have found that excimer laser procedures might be able to reactivate the HSV. The other risk, surgeons say, comes from trying to laser through any corneal scars left over from previous HSV episodes.
 |
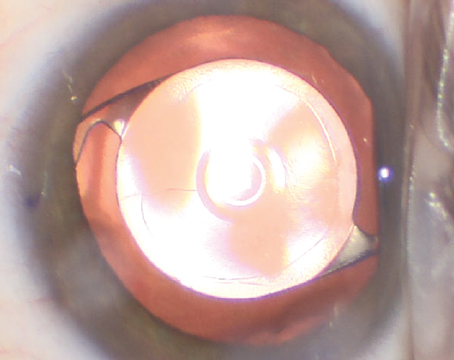
| A history of herpes simplex keratitis poses the risk of recurrence post-LASIK or PRK. David Hardten, MD |
In one report, an elderly woman underwent phototherapeutic keratectomy for band-shaped keratopathy. Researchers took tear samples preop and postop, and then performed polymerase chain reaction assays to quantify the HSV DNA in her tears. They found that the PTK appeared to have triggered viral shedding, as the HSV DNA only appeared in the postop samples.1
In another paper, researchers infected the ocular surface of 23 rabbits with HSV, then waited for it to resolve. The investigators then split the rabbits into two groups: de-epithelialization alone; and de-epithelialization plus PRK. Sixty-seven percent of the PRK group experienced HSV reactivation, compared to none of the former group.2
Because of this risk, surgeons are wary of such cases, but will perform refractive surgery under certain conditions. “Though such a case is a relative contraindication, I think a lot of surgeons have loosened their criteria a bit and will operate on this type of patient,” says Richard Davidson, MD, medical director for the faculty practice at the University of Colorado Hospital Eye Center. “If this patient’s history of herpes consisted of just one episode, with not much scarring, and the eye has been quiet for a while, I think surgeons would be willing to operate,” he says. “I’d plan on doing a PRK rather than a LASIK in such a patient; I’d rather not cut through corneal nerves in eyes that already have some damage to their corneal nerves. I’d start a patient with HSV history on antivirals a week preoperatively, and then probably keep him on them for two to three weeks postoperatively as things heal, in order to make sure he doesn’t get a reactivation. The key is making sure he’s been quiet for a decent period of time beforehand, and making sure you’re not treating a cornea that has significant scarring.”
Norfolk, Va., surgeon Elizabeth Yeu says she takes a very conservative approach to such patients. “Unfortunately, we corneal specialists end up seeing many corneal complications from disease such as HSV, and bad outcomes leave a lasting impression,” she says. “In personal correspondence with [LSU corneal specialist] Herb Kaufman, he has stated that, with proper antiviral prophylaxis, he’s seen great outcomes after performing LASIK in such patients, and doesn’t see a distant history of HSV keratitis as a hard contraindication.”
Los Altos, Calif., surgeon Bryan Lee says ophthalmologists shouldn’t feel the need to operate on such a patient, however, and that it’s all right to be more conservative. “For me, personally, if someone has a history of ocular HSV, I wouldn’t perform LASIK on him,” he says. “This is because many of these patients have corneal scars, so they won’t be able to have a femtosecond laser flap. If someone can’t have a femtosecond flap, I don’t do LASIK on him. Beyond that, there are reports of post-LASIK reactivation of the HSV. This reactivation might be related to the LASIK, or it might not be, since it also happens fairly frequently to patients who don’t have LASIK.” Dr. Lee also has a law degree, which he says makes him acutely aware of the legal ramifications of operating on such a patient. “For any type of situation in which you’re doing a refractive procedure on a patient that has a relative contraindication, having a very thorough informed consent conversation is critical,” he advises. “The patient should know all the risks and be able to make the most informed decision possible.”
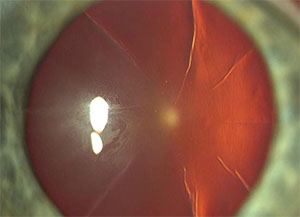 |
| The two main risks post-RK patients need to be aware of are the cornea’s possible unpredictable reaction to subsequent refractive surgery and the possibility of problems with the incisions during LASIK or PRK. |
The Post-RK Patient
The fluctuations in vision experienced by RK patients, as well as the presence of the incisions, make subsequent laser refractive surgery a dicey proposition. Given the right circumstances, though, surgeons say it can be done.
Dr. Davidson again prefers PRK over LASIK in such a patient. “I think it’s better to remove the epithelium than to cut a flap in some of these corneas,” he says. “If you talk to 10 different surgeons, though, you’d probably get 10 different answers. However, I feel strongly about PRK in this type of situation.
“You don’t have to modify your PRK technique so much as watch the RK incisions carefully,” Dr. Davidson continues. “Don’t put a lot of pressure on the globe, because even a moderate amount of pressure could potentially open up the incisions again. The key is being gentle.” The risk posed by the incisions was elucidated in a 2007 paper in Cornea. In it, a 39-year old LASIK patient who had a history of RK experienced a separation of his old incisions during the lifting of the femtosecond flap, with one of the incisions extending into the center of the cornea due to the force from the blunt spatula.3 “The incisions are unlikely to open with PRK, but it could possibly occur as you remove the epithelium and the epithelium turns out to be plugging some of the incisions,” Dr. Davidson says. “Obviously, you need to inform the patient ahead of time that the incisions opening is a possibility. If a surgeon were to perform LASIK over RK, he should be careful during the docking of the femtosecond laser. He has to understand that these RK incisions are made to the full depth of the cornea—there’s no way to avoid cutting through them.”
Personally, Dr. Lee wouldn’t do LASIK on a patient who has had RK. He acknowledges, though, that surgeons might consider PRK in such a patient, but advises the use of mitomycin-C. “The use of mitomycin-C is perfectly safe in the setting of PRK, but make sure you discuss mitomycin’s risks as experienced with its use in glaucoma surgery with the patient,” he says. “Also, discuss the fact that the RK cornea never stops changing. It fluctuates throughout the day and, over time, we know such patients become more hyperopic. The cornea becomes less predictable in terms of its reaction to future treatments. This discussion is important.”
Rheumatoid Arthritis
A patient with RA carries the risk of immunologic corneal melting postop, as well as a strong possibility of ocular surface issues that can impede a good result.
Dr. Yeu says that, similar to the HSV patient, it’s critical that the eye be as quiet as possible. “Autoimmune connective tissue diseases such as lupus and rheumatoid arthritis can pose unique challenges,” she says. “The disease severity and clinical presentation can vary greatly from patient to patient, and the overall picture really helps me decide whether or not they’re LASIK candidates. I want to ensure that their serologic levels are under control, and the patient is under the care of a rheumatologist for systemic control.”
Dr. Lee says the preop discussion is important, just as in the other conditions. “I’d let the patient know that there is at least a case report of someone having a post-LASIK corneal melt,” he says.4 “That’s why this is considered a relative contraindication. But, explain that it is relative; if he’s highly motivated and has really well-controlled disease—which has been under very good control for a year or longer without systemic problems—it’s all right to perform the surgery if he’s otherwise a candidate.”
Along with the systemic problems, however, RA also poses the risk of ocular surface issues, which can disrupt a LASIK outcome even in a non-RA patient. “I’d get the ocular surface under control for anyone, but for someone with RA, I’d definitely pretreat him,” Dr. Lee says. “I’d consider having the patient on pulsed oral steroids around the time of surgery, pretreat with warm compresses, artificial tears, omega-3 supplements and Restasis. Restasis takes three months before it really starts to kick in, but in terms of pretreatment for LASIK I’d want to do it for at least one or two months. I’d start all the other elements of the pretreatment regimen after I first saw the patient in clinic, and have them continue them for a month or two before the procedure. Postoperatively, taper the patient off the oral prednisone over a couple of weeks. You then have to be aggressive in treating the dry eye with plugs and the like. You want to stay on top of the ocular surface with those patients.” REVIEW
Drs. Lee and Yeu have consulted for Allergan. Dr. Davidson has no financial interest in the products discussed.
1. Deai T, Fukuda M, Tomoda Y, Higaki S, Hayashi K, Shimomura Y. Excimer laser photokeratectomy reactivates latent herpes simplex virus. Jpn J Ophthalmol 2004;48:6:570-2.
2. Epstein SP, Fisher EM, Sternberg GJ, et al. Recurrent ocular herpes simplex keratitis following excimer laser photorefractive keratectomy in a rabbit model. CLAO J 2001;27:2:94-9.
3. Perente I, Utine CA, Cakir H, Yilmaz OF. Complicated flap creation with femtosecond laser after radial keratotomy. Cornea 2007;26:9:1138-40.
4. Lahners WJ, Hardten DR, Lindstrom RL. Peripheral keratitis following LASIK. J Refract Surg 2003;19:6:671-5.