Centering on Success
Surgeons say one of the key aspects of topography-guided treatments in virgin corneas is centration, since these systems center differently than non-topo-guided systems.
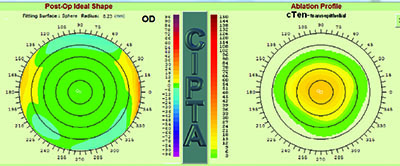
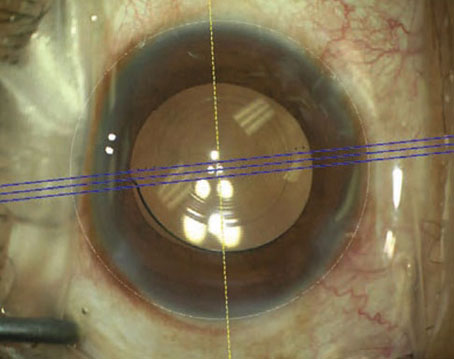
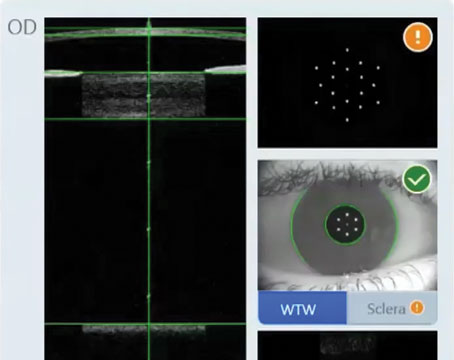
“Centration is very important, and needs to be on the corneal vertex in topography-guided procedures,” says Arun Jain, MD, of Chandigarh, India, who performs topography-guided treatments with a MEL-80 laser but says the general tips on centration can be applied to other devices. “Preoperatively, with the CRS Master device, topography is captured along the line of sight, or what we call the corneal vertex, but then the device overlays the ablation pattern onto the center of the pupil, even in topography-guided procedures. There is a provision in the CRS Master software, however, that lets you recenter it along the corneal vertex—also called the corneal apex or line of sight. Once we do that, we transfer this data to the MEL-80. On the MEL-80 we have to do an offset, asking the laser to center on the coaxially sighted corneal light reflex. This is because, normally, the software in the MEL-80 will center the ablation on the pupillary center. During the procedure, we tell the patient to fixate on the light, and we center the ablation on the coaxially sighted light reflex. In this way, we counteract the effect of angle kappa.”
Assessing Astigmatism
Aleksandar Stojanovich, MD, of Tromso, Norway, actually performs topography-guided ablation on all patients, using a transepithelial PRK approach. He says surgeons will have to make a few decisions when addressing the patient’s astigmatism.
“An example of a typical case would be a patient with 3 D of astigmatism on refraction, but 4 D of corneal astigmatism on topography,” says Dr. Stojanovich. “This is because the crystalline lens is partially compensating for the corneal astigmatism with its own astigmatism at the opposite axis. This leads to the question: Should we treat all 4 D in the cornea, or treat only that measured by refraction? Usually, in young people, we opt for the latter; we treat just the refractive astigmatism, treating the amount that will allow the patient to be emmetropic postop. For an older patient, however, a surgeon might say, ‘OK, the patient is older and will have cataracts soon, so we shouldn’t correct for all the astigmatism—which includes astigmatism from the lens—because we’ll then end up with corneal astigmatism that will remain as extra astigmatism when the cataract is removed.’ You have to judge it from patient to patient. However, usually, in younger patients it’s quite common to treat all the astigmatism on refraction.”
The Transition Zone
One of the ways that a topography-guided ablation potentially differs from a wavefront-guided one is the ability to have more control over the transition zone.
Dr. Stojanovich says his system allows him to impart a dioptric gradient between treated and untreated areas. “You can make the transition super-smooth, taking as much tissue as necessary to make it as wide as possible,” he says, “or you can economize things and use less tissue to create a transition zone.
|
Topo-guided Results
Surgeons have also studied the results from topography-guided procedures and found them equivalent to—and by some measures, better than—other laser procedures.
Alcon performed a Food and Drug Administration study of its topography-guided custom ablation treatment in virgin corneas of 249 eyes of 212 patients (though not all eyes were available at all follow-up points).1 In terms of efficacy, at 12 months the average manifest refraction spherical equivalent had been reduced to 0 D from a preop average of -4.61 D; 99 percent of eyes saw 20/32 or better uncorrected, 93 percent saw 20/20 or better and 65 percent saw 20/15 or better. At that same time point, 99.6 percent of eyes were within 1 D of the intended target, and 94.8 percent were within 0.5 D.
On the safety side, in the T-CAT FDA study, at one month postop, 4 percent of eyes had lost a line of best-corrected vision. This percentage decreased to 2.2 percent at a year. At a year, 0.4 percent had lost two lines of vision.
Also at a year, 57 percent had no change in BCVA, while 27 percent gained one line, 10.4 percent gained two lines and 3 percent gained greater than two lines of vision. Comparing postop UCVA to preop BCVA, at one year 30 percent had an UCVA one or more lines better than their preop BCVA, and 11 percent had an UCVA that was two or more lines better.
At his practice, Dr. Jain has also performed a study of the safety and efficacy of topography-guided LASIK. In his study, however, he added the wrinkle of performing the topo-guided ablation in one eye of each patient and a wavefront-optimized procedure in the other in order to compare the two. He performed the surgeries in 20 patients.
“We only took eyes in which the spherical equivalent was no more than 6 D,” Dr. Jain explains. “A main difference that we found postop was in ablation depth: In topography-guided eyes, we saved an average of 15 µm of corneal tissue compared to wavefront-optimized eyes. The average depth was around 66 µm in topography-guided vs. an average of 80 µm in wavefront-optimized. This could possibly translate to increased biomechanical stability of the cornea in the long term, or might allow us to correct higher amounts of refractive error. In terms of refractive results, 100 percent of the eyes in the topography-guided group were within 1 D of intended, and 90 percent were within 0.5 D at six months. In the wavefront-optimized group, 90 percent were within 1 D and 80 percent were within 0.5 D at six months. But the main visual difference, which was also reported in a similar way in the FDA trial study, was that, in our study, almost 30 percent of eyes in the topography-guided group gained more than one line of BCVA, compared to only 20 percent in the wavefront-optimized group.”
Dr. Jain says that, though both topography-guided and other custom procedures provide excellent results now, the future will see a melding of the technologies. “As of now, none of the topography-guided laser systems also uses higher-order aberrations in planning the ablation pattern,” he says. “The future will involve the use of a combination of corneal aberrations, topography and the total eye refraction to correct the complete visual status of the eye.” REVIEW
1. https://www.myalcon.com/products/surgical/wavelight-t-cat-study/clinical-study-results.shtml. Accessed 1 May 2015.