Catching the Problem
Assessing the extent of a patient’s ocular surface issues will point you toward potential solutions, surgeons say.
“The ocular surface is very important in refractive surgery,” says Sioux Falls, S.D., surgeon Vance Thompson. “The air/tear interface is the most powerful refracting element of the eye, and if it’s deficient due to aqueous deficiency or is breaking up early due to meibomian gland dysfunction, it will affect our laser vision correction results. In our clinic, every patient has dry eye until proven otherwise.”
A good patient history is an important aspect of the diagnosis. “I want to find out anything that might lead me to believe the patient could develop dry eye,” explains Norfolk, Va., ophthalmologist Elizabeth Yeu. “So, I look for any risk factors such as contact lens intolerance, an erratic sleep schedule, prolonged hours spent on computer devices and even seasonal or perennial allergies. Age is also a factor. We also look for comorbidities and ask what medications they’re on. Younger patients—especially those telling me that they’re dry—who disclose the use of psychotropic medications, sleep aids or anxiolytics raise my index of suspicion for how aggressively I need to treat for potential dry-eye disease in the postop period.”
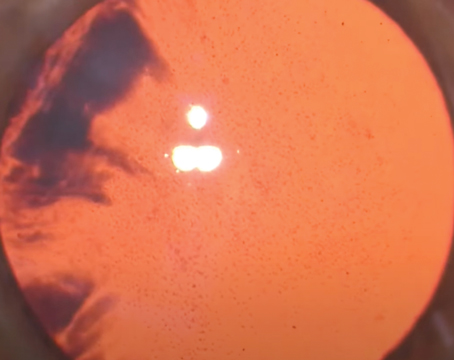
Working in tandem with the history are the results of a thorough exam. “I look at the tear meniscus, fluorescein staining and will occasionally do rose bengal staining if it looks severe and the conjunctiva looks very dry,” says Aurora, Colo., surgeon Rich Davidson, medical director of the faculty ophthalmology practice and vice chair for quality and clinical affairs at the University of Colorado Hospital Eye Center. “Then, looking at the lids themselves is important. It’s common for patients to get pigeonholed as dry-eye sufferers but sometimes, when you really look at them, you find they may have floppy eyelids or lower-lid laxity instead. So, it’s important to look at the lid position and make sure there’s no lagophthalmos or any type of exposure that can result in ocular surface issues.
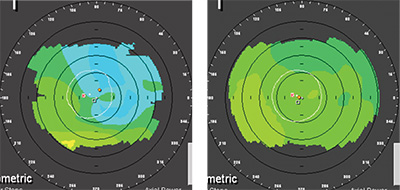
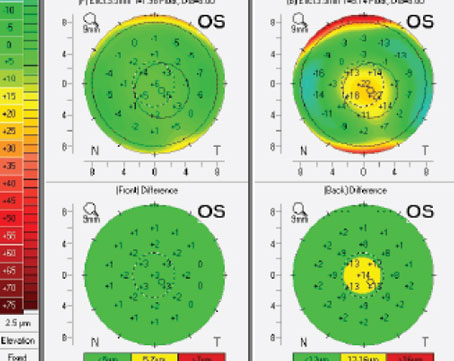
“We then look at the ocular surface itself,” Dr. Davidson continues. “It’s important to ascertain if patients have any meibomian gland disease. If they have such elements as crusting of the lashes or inspissated glands, that will help steer us in a certain direction. Also, depending on the severity of the ocular surface disease, it can even affect the diagnostic tests we do. If a patient has a cornea that’s really dry, it’ll affect our keratometry reading and our topography. I’ll do some cursory evaluations just to tell them whether I think they’re a candidate or not, but I won’t take any measurements for planning the actual surgery until the ocular surface has improved.”
Dr. Thompson says you can sometimes catch ocular surface problems by noting how well the patient reads the Snellen chart. “When people concentrate, their blink reflex can go down 30 percent,” he says. “So, if the patient finds that the chart is clear, gets blurry, but then clears with a blink, we already know that there are tear-film issues present, and that we’re going to want to normalize them.” In addition to the tests already mentioned, Dr. Thompson plans to add LipiView to his practice to help catch patients with problematic ocular surfaces.
|
Proper Treatment
Surgeons will adjust their therapy based on the cause and severity of the ocular surface problem.
“For patients with aqueous deficiency, our approach depends on the level of the deficiency,” says Dr. Thompson. “If it’s mild, we’ll just use lubricants and potentially Restasis. If it’s moderate to severe, however, we’ll start by using punctal plugs, lubricants and Restasis. We’ll also inquire about their home humidity. If it’s very dry, then we’ll ask them to turn it up. If their home isn’t conducive to that, we’ll ask them to get a humidifier. We ask if they’re using a ceiling fan, which can contribute to dryness. We also talk to them about computer use or if they’re a truck driver, because both situations require concentration, and blink reflexes go down when you concentrate. We’ll talk to them about the importance of blinking and using tear supplements in those situations.”
Dr. Yeu likes to work in oral supplementation. “We’ll start with artificial tears, and if they have more telangiectasia and poor mucin quality, I’ll move down the list and add oral omega 3 fatty acids, with or without the addition of an oral tetracycline,” she explains. “In this way, I’m tailoring the treatment for what seems to make up the majority of the disease. Everyone deserves oral supplementation, especially anyone who might be at risk for dry eye postop, but especially if they do have some form of staining. Once you start seeing corneal epithelial breakdown, however, it’s more than just revitalization. In that case, you’re actually having apoptosis and epitheliopathy. Any patient like that deserves to be on Restasis for the long haul, and should at least have a chronic course of it preop to prepare for the postop period. I will also use topical steroids to try to stabilize the surface as soon as possible and stop the destructive cycle of whatever’s causing the ocular surface breakdown. For mild to moderate thinning, I’ll start with something in the range of Lotemax or FML.”
In cases of meibomian gland dysfunction or lid problems, Dr. Davidson says he first rules out any anatomic lid abnormalities that might need to be corrected surgically. If those aren’t present, he’ll address the MGD. “We do the normal things like lid scrubs and warm compresses,” he says. “If it’s really inflamed, I’ll start the patient on a combination antibiotic/steroid drop such as Tobradex. I think this really helps kill the bacteria on the lid and reduce the ocular surface inflammation. Doxycycline can be helpful, as well.” Surgeons say that the LipiFlow treatment can also be helpful in some patients with MGD.
When gauging the effects of treatment, most surgeons like to see an absence of staining before moving forward with refractive surgery. “I’ll give patients three to four weeks before I bring them back,” says Dr. Davidson. “If things start to look better at the three to four week visit, I’ll want to get at least one other consistent reading two weeks after that. Then, I’ll do the surgery two weeks after that final measurement visit. So we’re looking at a two-month process to get things resolved, on average. At the follow-up visits, if a patient is symptomatic I want to reduce his symptoms, and I don’t want to see any staining, or at least markedly reduced staining. I’m looking for less lid inflammation, and I want to see the meibomian glands cleared up, if it’s MGD. If it’s aqueous-deficient dry eye, I want to make sure the patient’s tear meniscus and cornea are looking better.” REVIEW