Who Needs It?
Surprisingly, surgeons say they’re seeing more patients coming back after five or 10 years asking for an enhancement, as opposed to patients who just had their LASIK within the past year asking for a re-do. Either way, physicians say to make sure the enhancement is necessary.
“You want to make sure the best-corrected vision is good and they don’t have a significant cataract, retinal disease or any other factor that would be significantly limiting the vision,” says Beverly Hills, Calif., surgeon Andrew Caster. “You also want to make sure that the other factors that will lead to a successful procedure are present: good tear film; no significant lid disease; and sufficient stroma on topography and tomography.”
Majid Moshirfar, MD, director of refractive surgery and cornea at the University of Utah’s Moran Eye Center, says that he also makes sure the refraction is stable. “They need two consecutive acuity measurements performed three to six months apart and a cycloplegic refraction,” he says. “They also need tomography to determine if the refractive error is consistent with early keratoconus or if it’s lenticular myopia. The patient may also have developed epithelial hyperplasia from ocular surface dryness that led to the development of myopia.”
If the patient legitimately needs an enhancement, Dr. Caster likes to simulate what the resulting vision will be for the patient. “You want to show the patient the anticipated correction with spectacles,” he says. “If it’s a person of presbyopic age, make sure he understands the ramifications of both far and near vision, and that he thoroughly tests his far and near vision with the trial glasses. If it’s a myopic enhancement, I emphasize to presbyopic patients how this will have a negative impact on their near vision. If I’m creating monovision, I emphasize how it’s going to negatively impact their distance vision. I emphasize that this won’t solve all their vision needs but will make their vision better.”
PRK or Lift the Flap?
Surgeons say they usually go one of two routes for LASIK enhancement: Re-lift the flap and do LASIK or do PRK on top of the flap. Surgeons say the decision comes down to weighing the risk of epithelial ingrowth with LASIK vs. the slow visual recovery and risk of haze associated with PRK.
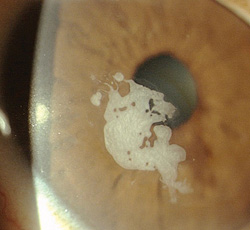
• Ingrowth concerns. “In a study at my practice, I found that my risk for epithelial ingrowth with primary LASIK was 1/1,440,” says Alan Carlson, MD, chief of corneal and refractive surgery services at the Duke Eye Center. “But it was 1/40 with LASIK enhancements. So I looked carefully at who to avoid with a flap lift: epithelial basement membrane dystrophy; neovascularization, especially across the flap edge; a history of ingrowth either in this eye or the other; if I had done a previous myopic LASIK; and situations where travel might be a problem for the patient in terms of postop follow-up.”
|
Dr. Caster says surgeons use this data in different ways. Some recommend a flap lift enhancement if it’s within the three-year period, but will do PRK if it’s been longer than that. “I take a different approach,” he says. “I recommend a LASIK enhancement for most of my patients who originally had LASIK with the understanding of the ingrowth risk if it’s longer than three years out. I carefully explain this to the patient, and say he’s got the option of PRK, but that I’m prepared to deal with the complication of ingrowth, because it’s a very rare patient in whom the first treatment for ingrowth doesn’t solve the problem. I feel the morbidity from the epithelial ingrowth and the subsequent ingrowth removal is less than the morbidity from a PRK procedure. PRK is also a different experience for patients; what they really dislike is the slow recovery of vision. People just don’t like a PRK enhancement when they’ve had a previous LASIK.”
• Surface ablation issues. Dr. Carlson acknowledges that surface ablation either takes away completely, or substantially reduces, the risk of ingrowth. “But the disadvantages are the medication usage is longer, there’s an added risk of haze and there’s what I call the mitomycin-C ‘black box’: It’s a lot of variability in the recommendations of how to use it. We got recommendations initially to use it for 40 seconds, then it was 24 seconds, and now they recommend using it for 12 seconds. Who knows what it’s going to be next year? Also, performing a flap lift conforms to patient expectations. If it goes well the healing is great and occurs at the LASIK interface, as opposed to the surface, where there could be some remodeling.” Dr. Carlson says it may be good to avoid this epithelial remodeling from PRK in the long run. “If you have a LASIK flap, there’s a good chance there are very fine irregularities in the flap,” he says. “If the irregularities are mild, then they’re typically not visually significant and the epithelium has remodeled to correct for them. If you perform a surface treatment—rather than lifting the flap, treating the bed, then placing the mild, accepted irregularity back down—you remove the epithelium and induce a new remodeling. The new epithelial remodeling could lead to a change in refraction.”
Dr. Moshirfar is a surgeon who saw Dr. Caster’s data and went in the direction of surface ablation for long-standing flaps. “I think the standard of care now for me, if someone comes in who’s five to 10 years out, is to perform surface ablation for the enhancement,” Dr. Moshirfar says. “But what about patients who had LASIK five or six months ago? If the surgeon knows the patient and is confident in the thickness of the residual stromal bed, and the refractive error makes sense and is stable, I think lifting is valid.”
Though mitomycin-C has made haze less of an issue than it used to be with surface ablation, Dr. Moshirfar acknowledges that it’s something to keep in mind. “There’s still a chance you might cause PRK haze,” he says. “For instance, say a LASIK patient who was -9 D before LASIK comes back and is -3 D. There’s a chance you might get haze in this case due to the laser treatment inadvertently ablating the flap and then lasering through it. That event can cause haze. It’s a small possibility.
“If the patient has a very small correction and PRK is being used for the enhancement, it makes sense to use mitomycin-C,” Dr. Moshirfar adds. “If it’s a -1.5 D virgin cornea, you don’t need to use it. But for -1.5 D with an enhancement—there’s a risk for haze with that, so I don’t think it would be a bad idea to use mitomycin-C.”
• Ectasia worries. Dr. Carlson agrees that it’s crucial to get the stromal bed measurement right, since another complication of flap-lift enhancement—rarer than ingrowth but more devastating—is corneal ectasia. “The vast majority of patients who develop ectasia are those who have undergone a flap-lift enhancement,” says Dr. Carlson. “And the largest settlements in LASIK court cases are those in which the patients went on to ectasia.” REVIEW
1. Caster AI, Friess DW, Schwendeman FJ. Incidence of epithelial ingrowth in primary and retreatment laser in situ keratomileusis. J Cataract Refract Surg 2010;36:1:97-101.