SURGEONS APPEAR TO BE TAKING SURFACE PROCEDURES more seriously as a refractive option for their patients. However, postoperative pain has been one of the main stumbling blocks for these surgeries. If you perform surface procedures such as PRK, LASEK or epi-LASIK, or are thinking about getting involved with them, here are tips on pain management from several surface-procedure experts.
Mountain View, Calif., surgeon Lee Shahinian Jr. says the most important preop treatment involves a frank discussion about pain in the context of the advantages and disadvantages of surface ablation.
"It's important to prepare patients for the fact that surface ablation is a different entity from the more popular LASIK in terms of discomfort and the recovery of vision in the first several days after the procedure," he explains. "I think the patient has to hear that message more than once preoperatively, because he will be talking to his co-workers or neighbors who had LASIK, and will hear about how they had no pain and recovered their vision quickly."
Miami surgeon William Trattler feels that the primary cause of pain after surface procedures is dry eye. So, he makes an effort to diagnose dry eye and treat it ahead of time. "It's a critical issue," he says. "If the eye's very dry, there will be a lot of irritation during the early postoperative period and a delay in epithelial healing."
After a thorough history, Dr. Trattler performs a Schirmer's test with anesthesia and stains the cornea with fluorescein. If the patient has dry eye, he'll start him on Restasis (Allergan) b.i.d., and place punctal plugs if necessary. He'll also have the patient use lubricating drops preop, starting as soon as possible.
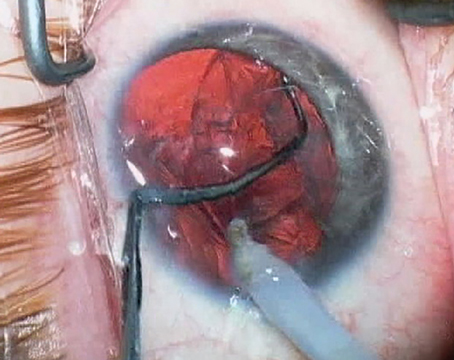
 |
| Miami's William Trattler, MD, uses tests like Schirmer's with anesthesia to root out dry eye, which he says is a major contributor to pain postop. |
Dr. Trattler chooses to give patients oral Celebrex 24 hours before surgery to help reduce the sensation of pain. "We're using it for a short period of time in a normal, not elevated dose, so they should be safe," he says.
Intraoperative Approaches
In addition to the usual drops, for preventing pain during surgery the watchword is "cold."
"I think irrigation with chilled BSS during the procedure or a 'Weck-Cel popsicle' can be helpful in reducing the heat generation in the cornea caused by the laser," says Dr. Trattler.
The Weck-Cel popsicle is a technique devised by Overland Park, Kan., surgeon Dan Durrie. As explained by Dr. Trattler, it involves soaking sterile Weck-Cel sponges in sterile BSS, placing them in a sterile baggy, then putting the baggy in the freezer. Then, during the procedure, you put a frozen Weck Cel on the cornea for eight to 10 seconds before the ablation and 12 to 14 seconds afterwards.
Postop Pain Control
In the postop period, surgeons bring out the big guns. The following techniques are in addition to the usual drop regiment.
The latest innovation may be "comfort drops" of dilute topical anesthetics to use on an as-needed basis. Dr. Shahinian pioneered this, and has a patent interest in a stabilized dilute tetracaine formulation he developed.
"Postoperatively, the heart of my approach is the use of 0.05% tetracaine in a 5-cc vial the patient can use every 15 to 30 minutes as needed for pain," Dr. Shahinian says. He has the mixture made for him by Leiter's Park Avenue Pharmacy in San Jose, Calif. (leiterrx.com; (408) 292-6772). He has no financial interest in the formulation from Leiter's. "We haven't seen any toxicity or delay in epithelial healing with this approach," he avers. "So the toxicity that's usually associated with topical anesthetics isn't there." Drs. Trattler and McDonald also use the comfort drops.
In addition to the tetracaine mixture, Dr. McDonald has the patients continue to take vitamin C for a week postop. She also has them continue the oral prednisone for five days postop on this schedule (counting surgery as day one): 80 mg (surgery day and the next); 40 mg (day three); 20 mg (day four); 10 mg (day five); 5 mg (day six).
"For patients who have had previous LASIK," she explains, "I'll give the prednisone for an extra two days preop, so they have a total of eight days of treatment. I preload in this fashion to prevent diffuse lamellar keratitis." She also prescribes Zantac 20 mg for the entire oral steroid course to prevent gastritis.
Dr. McDonald also prescribes prednisolone acetate (Pred Forte, Allergan) drops q.i.d. for a week, and ketorolac (Acular, Allergan) q.i.d. for three days. For patients with extreme refractive errors, or who have had previous corneal surgery, Dr. McDonald prescribes an extra week of prednisolone drops. "The dose for the second week may be as frequent as every two hours while awake for previous LASIK patients," she says. In addition to Tylenol, for extreme pain she prescribes Mepergan Forte (Demerol) to be taken every four to six hours as needed for three days.
Using her regimen, Dr. McDonald says she's lowered patients' subjective pain score of 10 (worst pain ever) to a score of two. "My goal is to make surface ablation as comfortable as LASIK," she says.