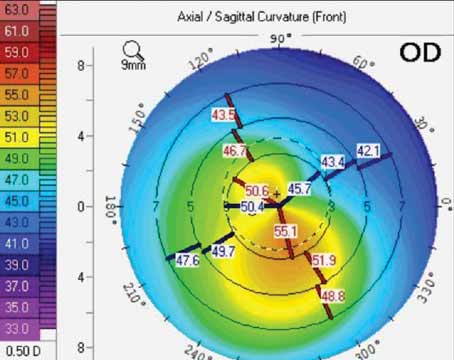
Preop Planning
Like many endeavors, surgeons say where you start often determines where you finish with Intacs.
“In planning, we go off of the corneal topography and refraction,” says Peter Hersh, MD, of Teaneck, N.J. “We try to get the best idea of where the cone is. It’s easiest when the refractive axis and topographic axis align and, if that’s the case, we take the steep axis and that’s where we make our incision. If the refractive and topographic astigmatism axes are not in accord, though, it’s a little more confusing. In those cases, I study the topography maps and even go back and study Scheimpflug maps on the Pentacam or OCT images. I find that by scrolling through these and looking at the maps, one can get a very good idea of the geographic depiction of the cone location, because what we’re doing, essentially, is trying to straddle the cone location.
“Then, I look at the difference between the steep and flat axes,” Dr. Hersh continues. “For this, we’re looking at the steepness of the cone and then, 180 degrees away, at the flatness of the cornea. Looking at this difference and the patient’s refraction tells me if I want to use two segments or one and, if I’m going to use two, do I want to use symmetrical segments or asymmetrical segments. For example, if a patient has a relatively low cone, there’s a big difference in the inferior to superior topographic power and the patient has a preponderance of astigmatism—mixed astigmatism in particular—then I’ll typically use one single segment aligned beneath the cone. If there’s asymmetry and more myopia, then I’ll consider asymmetric segments. And, if there’s mostly myopia and little astigmatism with a central cone—meaning not much of an inferior/superior difference—then I’ll use symmetrical segments, because if you use a single segment or two asymmetrical ones there tends to be coupling. Particularly with a single segment, coupling will flatten the cone inferiorly where the cone is located and simultaneously steepen it superiorly, with the effect being greater corneal symmetry and improved best-corrected vision.”
|
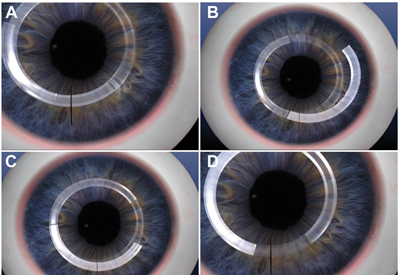
Creating the Channels
To create the channels where the Intac or Intacs will sit, surgeons can choose a manual or a femtosecond method.
“One of the major problems with manual channel creation is it’s not very predictable,” says Chennai, India, surgeon Soosan Jacob. “You can’t be exactly sure about the depth of the Intacs’ placement. With manual, it’s easier to get a decentration or to go more superficial or deep than you’d been planning for. There can be variations in the centration of the channel with respect to the pupil as well as the depth of the cornea.”
Although, like Dr. Jacob, Dr. Hersh uses the femtosecond for almost all of his Intacs cases, he says it’s not foolproof. “In some cases it can be more difficult to place the Intac with the femtosecond-created channel than a mechanical one because, with a mechanical, you’re completely separating a smooth channel,” Dr. Hersh says. “But, when you use the femtosecond, you still have some residual anchors that haven’t been split by the femtosecond, so it might be a little more difficult to pass the Intac through.”
Dr. Jacob says that, in some cases, the laser may make the 360-degree circumferential cut but not the entry incision you need to introduce the segment into the corneal channel. “If this occurs, take a 15 blade and cut down to the depth of the channel,” she says. “You need to know when to stop, however, since you might go below it or stop short of the actual channel. If either of those situations occurs, when you put the segment in you might create a false channel by inserting it at the wrong depth. To make sure you cut down to the proper depth, do so before the bubbles that were created when the channel was formed by the femtosecond dissipate. When your blade reaches the plane of the bubbles, they will escape through the incision and you’ll know you’re at the proper plane of the channel. If you delay, however, and the bubbles disappear, you won’t know where the channel is and it will be very difficult to locate.
“In case you anticipate a delay,” Dr. Jacob adds, “make sure you mark 360 degrees over the channel with a marker pen so that there is no confusion regarding the location of the channel.”
Placement Issues
Once the channel is created, surgeons say you still have to remain vigilant for complications as you slide the segments in.
“You have to be meticulous, going little by little, as you push the segment through the channel,” says Dr. Hersh. “I’ve found it helpful if you provide counter traction at the end of the Intac to give a little stretch as it’s going through. You do this by using your other hand to manipulate the periphery of the cornea in that area.” Even when a surgeon is careful, however, a segment can occasionally go off-course and start creating a false channel by driving into the corneal lamellae next to the real channel. The false channel can be in any direction from the main channel.
“You’ll know you’re getting a false channel because you’ll feel increased resistance as you insert the Intacs segment,” Dr. Jacob says. “At that point, you must stop pushing, because the more you push, the larger the false channel will be. Another way to detect the creation of a false channel is you will begin to see radiating folds around the leading edge of the segment.”
If a false channel occurs, Dr. Jacob performs what she calls the turnaround technique. “With a false channel, an internal lip is formed from some of the stromal lamellae that you cleaved into with the segment,” Dr. Jacob explains. “That lip separates the true channel from the false one, and the more you push, the more you enlarge the lip. At this point, you will never be able to regain the true channel in that direction, since the segment will always slide into the false channel. However, with the turnaround technique that I developed, you come around from the opposite direction and the lip flattens, allowing you to regain the original channel.” (For a video of the turnaround technique, visit http://goo.gl/t9L2fR.)
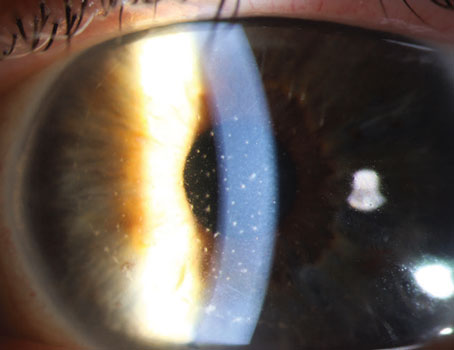
Other issues that can occur are incision gaping and migration of the Intacs postop. “If I’m planning on using a single segment, I’ll make my incision site a little more distant from the head of the segment than I would for double segments,” Dr. Hersh says. “What this does is bring the incision site farther away from the ultimate Intacs placement. I think this mitigates potential problems that one might have with gaping of the incision, potential infection of the incision site and also possible migration out of the incision site. Specifically, I set my laser to create the entry incision site 10 degrees distal to where the head of the Intacs will be.”
In a study of 850 eyes of 531 patients, Dr. Coskunseven says the segments were displaced postop in 11 cases (0.8 percent).1 In seven of the cases the segments migrated in the channel and a suture placed at the incision stopped any further movement. Four segments moved toward the surface, though, and had to be removed before any perforation occurred. Dr. Jacob says superficial migration is possible if a false channel occurs, but the surgeon finishes the case. “It’s possible to leave it in such a way that it straddles the incision,” she says. “However, I don’t do this because if the tip of the Intacs is underlying the incision, there’s a higher chance of foreign body complications such as neovascularization, migration, extrusion and stromal erosion.” REVIEW
1. Coskunseven E, Kymionis G, Tsiklis N, et al. Complications of intrastromal corneal ring segment implantation using a femtosecond laser for channel creation: A survey of 850 eyes with keratoconus. Acta Ophthalmologica 2011;89:54-57.