Prevention and Risk Factors
Surgeons say some things seem to predispose patients toward ingrowth, and knowing about them ahead of time can avoid problems.
“I’d say the incidence is from 1 to 3 percent following LASIK, and most of the time it occurs with enhancements,” says Michael Taravella, MD, professor of ophthalmology at the University of Colorado School of Medicine. “The other risk factor, especially with enhancements, is if you’re performing a hyperopic correction. With these, because the ablation is outside the original stromal bed, I think that can stimulate the epithelium around the edge, making the patient prone to ingrowth.”
Beverly Hills, Calif., surgeon Andrew Caster did a study of ingrowth, and found that when a surgeon did a flap lift enhancement within the first three years, the rate of clinically significant ingrowth was 1 percent.1 “After three years, though, it jumped to about 7 percent,” Dr. Caster says. “And that risk remained stable over time.”
Surgeons note there are steps you can take during surgery to decrease the risk of ingrowth.
|
Scott MacRae, MD, a professor at the University of Rochester Medical Center, says flap alignment helps, too. “I like to make sure that the flap is well-aligned postop,” he says. “Think of it as trying to reunite the cells you bisected. You don’t want asymmetry where the flap has shifted to one side, because that opens up the edge of the flap for invasion by the epithelium.”
Dr. MacRae also tries to help the flap’s natural sealing process by using a small fan. “Once the epithelial barrier and endothelial pump kick in, and you dry the cornea a little, it osmotically seals,” he says. “So, the more you can gently dry it, it probably seals the flap better and makes it less likely to have small tunnels through which the epithelium can migrate. However, if you dry it too much you’ll see the flap retract. So, I’ll use the small, handheld, batter-powered fan to do some blowing on the cornea from six to eight inches. For primary LASIK, I’ll use the fan for 10 to 15 seconds, and for retreatments I’ll use it for a minute.”
For hyperopic ablations during retreatments for overcorrected primary myopic LASIK, Dr. Taravella uses a tip a colleague mentioned: Protect the epithelium with Goniosol. “I’ll take a TB syringe and put a little Goniosol in it, and put a 19-ga. cannula on it. I’ll then apply it to the periphery of the cornea, taking care not to let it leak into the stromal bed and interfere with the ablation. Since the hyperopic ablation is sometimes bigger than the myopic ablation’s bed, sometimes you’ll notice laser spots going outside of the original bed. However, if you shield the epithelium from them, I think you’re less likely to stimulate ingrowth.”
Managing Ingrowth
For the unfortunate times when ingrowth occurs, surgeons have various approaches that they say help remove the cells and prevent them from recurring.
There is some ingrowth that won’t progress and can just be observed, surgeons say. “It’s common to see a little bit [of ingrowth] after enhancements,” says Dr. Taravella. “However, if it is within 1 mm of the flap edge and isn’t causing any flap adherence problems, is stable and not growing, I’ll usually just watch the patient carefully, especially in the first week or two after an enhancement to make sure they’re not showing any signs of it growing or affecting the refraction. But if it’s 2 to 3 mm in, you’ll probably have to treat it. The ones you have to be concerned about are those that are progressing, or when you see flap melt occurring.” Dr. Taravella also says that early topography can help, since if the area around the ingrowth is elevated and is causing some irregular astigmatism, that’s an indication that you need to treat it.
Jules Stein Eye Institute surgeon Kevin Miller says proliferation on all sides usually isn’t a good sign. “If it grows from both sides—you get a wraparound—and the edge of the flap is kind of loose, those cases don’t tend to do well,” he says.
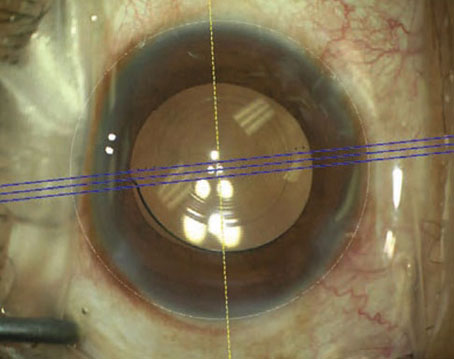
To treat cells, some surgeons like lifting the entire flap, while others just like to expose the area of ingrowth. Dr. Taravella, who flips the whole flap, first marks the cornea. “At the slit lamp, with a marking pen I’ll mark the extent of the ingrowth both circumferentially around the edge of the bed and also centrally,” he says. “I’ll also mark the flap so I know where it is on the flap edge. Then, I’ll lift the flap. The ingrowth is usually easy to see and very loose. For the most part, you can remove it with a Weck-Cel sponge and maybe light scraping with a blade, though I think it’s important to remove it from both the bed and underside of the flap. I’ll then inspect the area on low and high magnification, and under the Visx laser’s ring light, which I think highlights epithelial changes better than the oblique light. I’ll try to clean it as meticulously as I can.”
Dr. MacRae also marks the cornea, but prefers just removing the cells from a local area, rather than lifting the entire flap. “If it’s a small area of ingrowth, I may wash it out with an irrigation cannula at the slit lamp and then dry it with the fan,” Dr. MacRae says. “If it’s more extensive, or if it comes back, I will lift the flap only in the region where I want to remove the ingrowth—there’s no sense stirring up the epithelium someplace else. I’ll use a spatula to retract the flap and clean out the cells by gently scraping both the flap side and the stromal bed with a 64 blade. For a lot of these patients, I’ll place a bandage contact lens, which makes recovery easier.”
For a recurrence, Dr. Taravella has had success with a technique described by Minneapolis surgeon David Hardten. “You lift it, meticulously clean the area, re-seat the flap and then apply Tisseel fibrin glue on the entire flap edge,” he explains. “You then put on a contact lens.”
In tough recurrences, suturing is also an option, though it can induce astigmatism that may not completely resolve. To help deal with this, Dr. MacRae uses a technique he heard about from Overland Park, Kan., surgeon Dan Durrie. “I’ll lift the area, clean it out, then suture down the flap,” he explains. “Sometimes I’ll do a horizontal mattress suture. The key is not to bury the knots, but instead keep the knots in the peripheral untouched cornea and put a bandage contact lens on. When you bury them, it causes a lot of corneal distortion; you have to pull the knots aggressively to tighten them. I’ve found that, by not lifting the entire flap when you clean it and then putting sutures in and covering it with a contact lens, the cornea will go back to its original flap position.”
Surgeons say epithelial ingrowth is a problem that, though infrequent, they’re always thinking about and trying to outmaneuver. “Other than ablations that don’t fully correct the refractive error,” says Dr. Miller, “ingrowth is probably the biggest current problem in LASIK. Though it occurs less frequently than before, this particular problem hasn’t gone away yet.” REVIEW
1. Caster AI, Friess DW, Schwendeman FJ. Incidence of epithelial ingrowth in primary and retreatment laser in situ keratomileusis. J Cataract Refract Surg 2010;36:1:97-101.