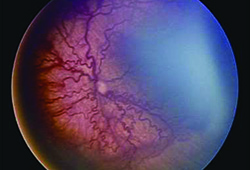
The disease is an ischemic retinopathy in premature and low birth weight infants that can lead to retinal detachment and blindness. It is typically characterized by the location (zone) and clinical appearance (stage). Current guidelines recommend screening babies born at 30 weeks gestational age or earlier, or any baby weighing less than 1,500 g. Any baby who undergoes a difficult clinical course, as determined by the referring neonatologist, also meets the criteria for screening. The first exam is typically performed about four weeks after birth, with subsequent exams every one or two weeks until the retina is fully vascularized.2 Laser treatment to the avascular retina has been standard of care since the 1990s and bevacizumab injection has recently been used successfully, as well.
The population of premature infants is expected to grow significantly in the coming years with advances in medical care and a growing population.3,4 Traditionally, screening exams for ROP consisted of a trained ophthalmologist examining the patient at the bedside until the retina completely vascularized, the disease regressed or treatment was implemented. There are a number of logistic complications involved with the traditional method of screening for ROP: Few specialists with the required expertise are available to examine a growing population of infant patients; medico-legal concerns continue to discourage practitioners from covering ROP exams; and the training required to become competent in the exam is extensive.3,4 Recently, telemedicine, the practice of capturing clinical photographs for review by a medical expert often geographically distant from the patient, has been studied as an alternative to the traditional method of ROP screening. This article will summarize the literature on telemedicine use for ROP and discuss benefits and drawbacks.
Evidence of Validity
For telemedicine to be successful at supplementing or replacing traditional ROP screening exams, the quality of the retinal image taken must be sufficient for examination; the individual reading the image must be able to accurately assess the level of disease; and this must be done in a timely fashion. A 2006 multicenter study of infants at Jackson
|
The Photo-ROP study from 2008 found similar results, finding that in 102 eyes from 51 infants, two physician ROP experts were able to diagnose ROP requiring treatment with 86- to 100-percent sensitivity and 68- percent specificity compared to exam. These studies all demonstrate excellent sensitivity and negative predictive value, or that the examiner was able to capture all cases of infants that truly had treatment-warranted ROP. These earlier studies demonstrate that the quality of fundoscopic images taken by trained individuals is sufficient to allow telemedicine diagnosis of ROP when trained ROP experts examine the images.
More recently, two large studies have examined whether non-physician trained personnel can review retinal images and accurately diagnose treatment-warranted ROP. A study of 67 infants from the Columbia University NICU compared the ability of 14 trained non-experts and three retina specialists to diagnose treatment-warranted ROP against standard exam by an experienced pediatric ophthalmologist.6 The non-experts consisted of one retina fellow, four ophthalmology residents, eight medical students and one neonatal nurse; all completed two hours of training on image-based ROP diagnosis by the authors of the study.
The authors found that the three retina specialists achieved 100-percent sensitivity and 93-percent specificity in detecting treatment-warranted ROP, while the residents achieved 88-percent sensitivity and 84-percent specificity and the students achieved 82-percent sensitivity and 92-percent specificity. The three best residents and three best students achieved 100 percent sensitivity, demonstrating variability within the groups.6 This study suggests strongly that non-experts can be trained to become proficient at image-based ROP diagnosis.
A recently published multicenter study from the eROP cooperative group supports this finding.7 The eROP study enrolled 1,257 infants with birth weight below 1,250 g and showed that two trained non-physician personnel were able to correctly diagnose treatment-warranted ROP with 82-percent sensitivity and 90-percent specificity when viewing images taken by 25 non-physician study personnel. When factoring in both eyes, sensitivity increased to 90 percent and specificity to 87 percent with negative predictive value of 97 percent. Most importantly, only three out of 162 infants who were treated by laser did not have treatment-warranted ROP diagnosed on the image set before laser was performed. Image quality did play an important role in the ability to make the correct diagnosis, as sensitivity increased from 68 percent to 85 percent when all of the retinal images used were judged to be good or acceptable.7 The authors conclude that the study provides strong support for using a telemedicine system consisting of trained non-physician imagers and readers to detect referral-warranted ROP in at-risk infants.
While these studies provide strong evidence that non-physician personnel can diagnose treatment-warranted ROP accurately, a study from 2007 conducted in North Carolina comparing a computer program to detect plus disease to experts found that the program could correctly detect plus disease with 97-percent sensitivity and 94-percent specificity.8 The potential of computer software to support ROP diagnosis is currently an untapped resource, but future studies may advance this nascent field.
In 2013, Daniel Weaver, MD, and Todd Murdock, MD, presented their experience with telemedicine detection of ROP in a distant neonatal intensive care unit in Montana.9 They performed a retrospective review of 582 telemedicine examinations of 137 infants over four years. A RetCam system was used to take pictures, which were posted on a secure server for evaluation by a remote ophthalmologist. Infants suspected of having ROP that may need treatment were transferred to a hospital capable of supporting examination and treatment. Infants determined not to be at risk received an outpatient examination within two weeks of discharge. Good outcomes occurred in all cases, with none progressing to retinal detachment. The authors concluded that telemedicine screening for ROP effectively detected patients in need of laser treatment, allowing prompt transfer with no poor outcomes over a 4.5-year period.
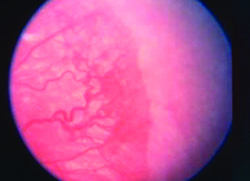
Sasapin G. Prakalapakorn, MD, and colleagues reported the results of a trial using a Keeler indirect ophthalmoscopy imaging system.10 This study was a retrospective review of the medical records of infants screened for ROP who had retinal images taken and sent to two masked reviewers who graded the images based on quality, number of gradable quadrants, and predictability of plus disease. One eye each of 253 infants was evaluated. Grader 1 found the quality of 94 percent of images to be fair or good; grader 2, found 83 percent of the images to be fair or good. Grader 1 judged 87 percent of images to have at least three gradable quadrants; grader 2 found 77 percent of the images to have at least three gradable quadrants. The sensitivity and specificity of grading pre-plus or plus disease were 100 percent and 86 percent for grader 1, and 94 percent and 89 percent for grader 2. The authors concluded that telemedicine using indirect ophthalmoscopy may be a valuable tool for ROP screening.
|
For each method, operating characteristic curves were created and three expert ophthalmologist opinions were used as the comparative standard. Ideal points for plus disease were selected and then tested on a second set of 184 quadrants of 46 different images. The authors concluded that ROPtool had a high overall accuracy in predicting clinically significant changes in retinal vascular dilation and tortuosity and was very likely to aid in telemedicine plus- disease diagnosis.
Challenges Remain
While current studies provide strong support for the use of telemedicine with trained personnel, there are still infants with treatment-warranted ROP who may be missed. It is uncertain at this time what safeguards can be implemented to minimize the number of such infants, or what legal protections would be in place to support a telemedicine program. If disease is detected, ophthalmologists would still have to perform laser or bevacizumab treatment for infants, and it is possible that with fewer exams performed, the skills required to perform depressed fundus exams necessary for laser therapy may be compromised. Despite these questions, the prospect of telemedicine for ROP screening remains promising. REVIEW
Dr. Cao is a resident and Dr. Fecarotta is an assistant clinical professor of ophthalmology, both at SUNY Downstate Medical Center.
1. Harnett EM, Penn JS. Mechanisms and management of retinopathy of prematurity. N Engl J Med 2012;367:2515-26.
2. Screening Examination of Premature Infants for Retinopathy of Prematurity. Section on Ophthalmology American Academy of Pediatrics; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus. Pediatrics 2006;117:572-6.
3. Chiang MF, Keenan JD, Starren JB, et al. Accuracy and reliability of remote retinopathy of prematurity diagnosis. Arch Ophthalmol 2006;124:322-327.
4. Chiang MF, Wang L, Busuioc M, et al. Telemedical retinopathy of prematurity diagnosis: Accuracy, reliability, and image quality. Arch Ophthalmol 2007;125:1531-1538.
5. Fijalkowski N, Zheng L, Henderson M, Wallenstein M, et al. Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP): Four-years of screening with telemedicine. Curr Eye Res 2013;38(2):283-91.
6. Williams S, Wang L, Kane SA, Lee TC, et al. Telemedical diagnosis of retinopathy of prematurity: Accuracy of expert versus non-expert graders. Br J Ophthalmol 2010;94:351-6. doi: 10.1136/bjo.2009.166348. Epub 2009 Dec 2.
7. Quinn G, Ying G, Daniel E, Hildebrand P, et al; for the e-ROP Cooperative Group. Validity of a Telemedicine System for the Evaluation of Acute-Phase Retinopathy of Prematurity. JAMA Ophthalmol 2014 Jun 26. doi: 10.1001/jamaophthalmol.2014.1604.
8. Wallace DK1, Freedman SF, Zhao Z, Jung SH. Accuracy of ROPtool vs individual examiners in assessing retinal vascular tortuosity. Arch Ophthalmol 2007;125:1523-30.
9. Weaver DR, Murdock TJ. Telemedicine detection of type 1 ROP in a distant neonatal intensive care unit. J AAPOS. 2012;16(3):229-33. doi: 10.1016/j.jaapos.2012.01.007
10. Prakalapakorn SG, Freedman SF, Wallace DK. Evaluation of an indirect ophthalmoscopy digital photographic system as a retinopathy of prematurity screening tool. J AAPOS 2014;18(1):36-41. doi: 10.1016/j.jaapos.2013.10.018.
11. Cabrera MT, Freedman SF, Kiely AE, Chiang MF, and Wallace DK. Combining ROPtool measurements of vascular tortuosity and width to quantify plus disease in retinopathy of prematurity. JAAPOS 2011;15:40-44.