Of course, uveitic glaucoma is a bit different from primary open-angle glaucoma. Among other things, the cause of the glaucoma can be difficult to determine. It could be that pre-existing inflammation led to the elevated pressure and glaucoma; or it could be that steroids being used to treat the inflammation led to the glaucoma. The cause may even be a combination of both factors.
When you’re treating a patient with uveitic glaucoma and you’ve reached the point at which surgery is necessary, the first surgery one might consider is trabeculectomy or implantation of a tube shunt. However, uveitis by definition is inflammation in the eye, and inflammation leads to a higher rate of post-surgery failure. Tubes and trabs, for example, have a higher failure rate when used to address uveitic glaucoma than when used to treat primary open-angle glaucoma. Thus, to increase the odds of surgical success we need to try to fight the inflammation with tools such as anti-inflammatory drugs. Ironically, we often use the same steroids that can worsen the glaucoma as a way to help fight the inflammation and reduce the likelihood of surgical failure.
Given that surgical options such as tubes and trabs are more likely to fail in cases of uveitic glaucoma, it’s worth considering alternative options. A number of clinicians have looked at the effectiveness of other surgeries in recent years, and although the number of cases in some of their studies has been small—uveitic glaucoma is relatively uncommon, after all—their results suggest that other approaches may be worth considering.
Managing Childhood Uveitis
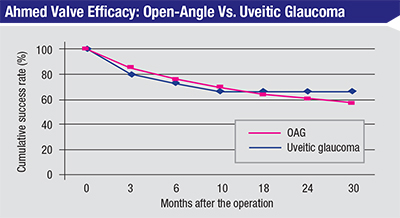 |
| In this retrospective, comparative, case-controlled study, 15 eyes with chronic uveitis and 53 eyes with uncontrolled open-angle glaucoma underwent Ahmed glaucoma valve implantation. No significant differences in intraocular pressure were found at three, six, 12, 24, or 30 months. The only complication that differed significantly was tube removal, which occurred more often in the uveitic glaucoma group (p=0.018). (Rachmiel et al, 2008)4 |
One of these studies on goniotomy was published in 2013;1 it was conducted by Dr. Sharon F. Freedman’s group at Duke University School of Medicine. This was a retrospective study of 36 patients with juvenile uveitic glaucoma who underwent one or more IOP-lowering surgical procedures; 31 of them had goniotomy as their first procedure. Success was defined as an IOP less than 21 mmHg with controlled inflammation, no need for further IOP-lowering surgery and no devastating complication.
With a mean follow-up of 5.6 years, 15 individuals in that group (48 percent) needed no further procedure to maintain an IOP of less than 21 mmHg with controlled inflammation. Nine others (29 percent) needed a second goniotomy. At 10 years, 69 percent of those treated with one or two goniotomies met the criteria for success. For a childhood form of glaucoma, these results are impressive.
Another retrospective study conducted by Dr. Freedman in 2002 evaluated the success rate of 19 goniotomies performed on 16 eyes of 12 patients whose mean preoperative IOP was 32.3 ±4.6 mmHg.2 Surgical success was achieved in 12 eyes (75 percent) with a mean postoperative IOP of 12 ±2.5 mmHg. In 10 of them (60 percent), surgical success was achieved after a single goniotomy.
Another retrospective study was conducted several years ago by Ho Ching Lin and colleagues at the Singapore National Eye Center.3 This study evaluated 54 goniotomies performed by a single surgeon, treating refractory childhood uveitic glaucoma in 40 eyes of 31 patients. The surgery met their definition of success (IOP no greater than 21 mmHg) in 29 eyes (72 percent); 22 of them (55 percent) required no medications to achieve this, while seven others (18 percent) required a mean of 1.6 ±1.1 medications. Factors that led to significantly better outcomes included phakic eyes; fewer peripheral anterior synechiae; no prior surgery; and patient age less than 10 years.
These outcomes suggest that goniotomy is a reasonable option to consider when treating childhood glaucoma associated with uveitis.
Tube or Trab?
When dealing with surgery for uveitic glaucoma—in adults or children—one question that may arise is whether to perform a trabeculectomy or implant a tube shunt. Unfortunately, the Tube vs. Trabeculectomy study didn’t include uveitic glaucoma. However, some inferences related to this question can be drawn from a few small studies that were published in recent years.
One 2008 study conducted at Toronto Western Hospital by Rony Rachmiel, MD, and colleagues was a large retrospective comparison of the success rate of Ahmed shunts in 25 eyes with uveitic glaucoma vs. 53 eyes with primary open-angle glaucoma.4 They found no significant difference in the success rate of the implants, with the sole exception that there were significantly more tube removals in the uveitic glaucoma group. In my experience, this is related to more frequent exposure of the tube or plate in uveitic patients. But despite this difference, the overall success rate was very similar.
Other studies have also addressed this question:
• In a 1999 study conducted at the Massachusetts Eye and Ear Infirmary,5 21 eyes of 19 patients whose uveitis was controlled by immunomodulatory therapy underwent Ahmed valve implantation. With an average follow-up of 24.5 months, all 21 eyes had IOPs between 5 and 18 mmHg; average medications were reduced from 3.5 before surgery to 0.6 after.
• A 2007 retrospective study of 60 eyes of 60 patients, also conducted at the Massachusetts Eye and Ear Infirmary,6 evaluated the long-term success of Ahmed valves in uveitic glaucoma patients. This study found that at one year vs. four years, 77 percent and 50 percent of eyes, respectively, had an IOP between 5 and 21 mmHg. Excluding eyes that had serious complications lowered the success rates to 57 percent and 39 percent at the two time points.
• A 2002 study conducted at the Bascom Palmer Eye Institute in Miami focused on 24 eyes of 24 uveitic glaucoma patients receiving Baerveldt implants.7 That study found success rates of 95.8 percent at three months and 91.7 percent at six, 12 and 24 months. (Success was defined as an IOP between 5 and 21 mmHg, with or without medications, without need for further glaucoma surgery.)
Other Surgical Options
Other studies have provided some information regarding the potential of different surgeries for uveitic glaucoma:
• Comparing trabeculectomy, trabeculotomy and Trabectome. A 2014 study conducted at Tohoku University Graduate School of Medicine in Sendai, Japan, evaluated 47 eyes of 47 uveitic glaucoma patients who underwent either trabeculectomy, trabeculotomy or Trabectome surgery, with an average of 40 months of follow-up.8 The success rates for the surgeries (with success defined as an IOP less than 21 mmHg and no need for additional surgery) were: trabeculectomy 83 percent; trabeculotomy 63 percent; and Trabectome 75 percent. Significant risk factors for failure included male sex (p=0.02), age less than 45 years (p=0.0009), nongranulomatous uveitis (p=0.04), and postoperative inflammation (p=0.01).
Interestingly, the Japanese have had a very positive experience with trabeculotomy for adult forms of glaucoma, and they have produced a body of literature that supports this. Most glaucoma specialists in the United States would find that strange. Over here, that procedure is traditionally reserved for children, because studies have shown that after about age 10 it really doesn’t work well.
• Trabeculodialysis. Another relevant study was reported in a poster at the 2015 annual meeting of the American Glaucoma Society. The study was conducted by Andrew Iwach’s Glaucoma Research & Education Group in San Francisco (the lead author was Lian Chen, MD). This retrospective study of 10 uveitic glaucoma eyes of 10 patients evaluated the success of using trabeculodialysis to treat the disease, with a 5.7-year follow-up. This procedure is in some ways very similar to goniotomy; the surgeon goes in with a knife and cuts at the level of the trabecular meshwork, essentially unhooking it from its normal insertion. Types of uveitis treated in this study included juvenile rheumatoid arthritis, herpetic uveitis and idiopathic uveitis.
The data showed that trabeculo-dialysis led to a 70-percent success rate (seven of 10 eyes) without the need for further surgery. Of those seven eyes, four required some medication to maintain the outcome. (The authors note that this surgery has a very favorable safety profile, making it worth considering before attempting a traditional surgery such as trabeculectomy or a tube shunt.) These results are very similar to the results found in the Japanese study, and the surgeries are somewhat similar; both attempt to treat the trabecular meshwork with either a knife or a device such as the Trabectome or a trabeculotome.
• Canaloplasty. Canaloplasty for uveitic glaucoma is another approach that requires thinking outside the box. A recent retrospective study of 19 eyes of 15 patients, conducted at the University of Montreal, evaluated the effectiveness of this type of surgery for treating herpetic, noninfectious and idiopathic uveitic glaucoma.9 The surgery consisted of 360 degrees of viscodilation followed by a tension suture. They found that 74 percent of the surgeries were a complete success; 11 percent were a partial success; and 16 percent were failures. There was a low complication rate.
All of the surgical options mentioned here produced reasonably good results. Given the difficulty in treating uveitic glaucoma, success of these surgeries (including some that are relatively new) in the range of 65 to 80 percent success is excellent.
Adjunctive Drugs
As you know, anti-VEGF drugs such as Avastin, Lucentis and Eylea are now being used to treat macular degeneration and diabetic retinopathy. However, there’s also a body of literature looking at these agents as adjuncts for glaucoma surgery. Like mitomycin-C, they can help prevent scarring by preventing new blood vessels from growing, vessels that would bring in more inflammatory factors. Furthermore, they may also directly prevent inflammation.
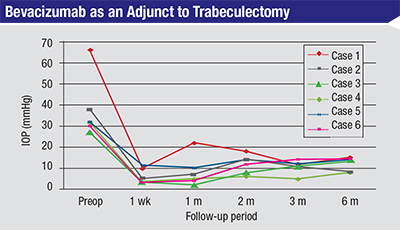 |
| In this prospective, observational case series, six cases of glaucoma—three of them uveitic glaucoma (cases #3, #4 and #6)—received a subconjunctival injection of bevacizumab at the time of trabeculectomy. All six cases had controlled pressures on no medications at six months. (Choi JY et al, 2010)10 |
Of course, it’s impossible to draw any firm conclusions from such a small sample and short follow-up, but since this is a prospective observational study, I consider these results promising and worthy of further testing. Based on these results, I believe adjunctive use of anti-VEGF drugs may show some promise in the treatment of uveitic glaucoma.
It’s also important to note the arrival of new treatments for inflammation, such as tumor necrosis factor inhibitors. These drugs suppress the immune system response to TNF, which appears as part of the inflammatory response, and they can have a profound impact on patients with uveitic glaucoma.
For example, I was following a child with a history of uveitis who had done poorly and was also suffering from glaucoma. Once these anti-TNF drugs became available, he started getting systemic treatment with one of them. His vision improved, his cystoid macular edema got better and his IOP was better controlled, probably because the inflammation was reduced. The drug had a powerful effect on his inflammation status, without the side effects associated with using steroids. For him it was almost a miracle drug.
Steroids, of course, are another challenge when dealing with uveitic glaucoma. They’re very good at treating certain diseases, uveitis included, and they can help to prevent scarring after surgery. However, they can also cause elevated pressure and cataracts. Using steroids therefore becomes a tricky balance for the uveitis specialist and glaucoma specialist, because steroids can be both friend and foe.
Certainly after the surgical treatment of glaucoma with a filtering procedure, heavy use of steroids is recommended. At that point, even if steroid use is the cause of the glaucoma, you’ve treated the elevated pressure in a very definitive way, at least in the short term. You’ve created a hole in the eye, and the pressure’s likely to be around 10 mmHg the next day. Steroids are favorable in this situation because they can help prevent uveitic inflammation, which can cause more failure. Certainly when treating primary open-angle glaucoma with a trabeculectomy it’s been shown that pretreating with steroids leads to a better surgical outcome. (Of course, over the long haul as the inflammation is controlled, the surgeon should taper the steroids appropriately to avoid continued high pressures and steroid glaucoma.)
Broadening Our Options
Uveitic glaucoma definitely comes with some unique challenges. For example, when treating other forms of glaucoma, factors such as age make a difference in our approach to treatment. Older patients don’t scar as much as younger patients, which can affect our choice of surgical options, such as how much mitomycin to use during surgery. But factors such as age matter less when you’re managing uveitic glaucoma, in part because the uveitis is a major driving force behind the scarring, overriding the reduction in scarring you would normally find in an older individual.
This is part of the reason it’s worth considering options besides the standard choices such as trabeculectomy and tube shunts. An uncommon form of glaucoma such as uveitic glaucoma is difficult to study because of the small number of patients most practices encounter; it will be difficult for many groups to do prospective, randomized, controlled trials involving uveitic glaucoma. Nevertheless, there are surgical alternatives, and the evidence—albeit limited—suggests that they may work as well, or better, than the traditional options. REVIEW
1. Bohnsack BL, Freedman SF. Surgical outcomes in childhood uveitic glaucoma. Am J Ophthalmol 2013;155:1:134-42. doi: 10.1016/j.ajo.2012.07.008. Epub 2012 Oct 2.
2. Freedman SF, Rodriguez-Rosa RE, Rojas MC, Enyedi LB. Goniotomy for glaucoma secondary to chronic childhood uveitis. Am J Ophthalmol 2002;133:5:617-21.
3. Ho CL, Wong EY, Walton DS. Goniosurgery for glaucoma complicating chronic childhood uveitis. Arch Ophthalmol 2004;122:6:838-44.
4. Rachmiel R, Trope GE, Buys YM, Flanagan JG, Chipman ML. Ahmed glaucoma valve implantation in uveitic glaucoma versus open-angle glaucoma patients. Can J Ophthalmol 2008;43:4:462-7. doi: 10.3129/i08-082.
5. Da Mata A, Burk SE, Netland PA, Baltatzis S, Christen W, Foster CS. Management of uveitic glaucoma with Ahmed glaucoma valve implantation. Ophthalmology 1999;106:11:2168-72.
6. Papadaki TG, Zacharopoulos IP, Pasquale LR, Christen WB, Netland PA, Foster CS. Long-term results of Ahmed glaucoma valve implantation for uveitic glaucoma. Am J Ophthalmol 2007;144:1:62-69. Epub 2007 May 9.
7. Ceballos EM, Parrish RK 2nd, Schiffman JC. Outcome of Baerveldt glaucoma drainage implants for the treatment of uveitic glaucoma. Ophthalmology 2002;109:12:2256-60.
8. Shimizu A, Maruyama K, Yokoyama Y, Tsuda S, Ryu M, Nakazawa T. Characteristics of uveitic glaucoma and evaluation of its surgical treatment. Clin Ophthalmol 2014 26;8:2383-9. doi: 10.2147/OPTH.S72383. eCollection 2014.
9. Kalin-Hajdu E, Hammamji K, Gagné S, Harasymowycz P. Outcome of viscodilation and tensioning of Schlemm’s canal for uveitic glaucoma. Can J Ophthalmol 2014;49:5:414-9. doi: 10.1016/j.jcjo.2014.07.001.
10. Choi JY1, Choi J, Kim YD. Subconjunctival bevacizumab as an adjunct to trabeculectomy in eyes with refractory glaucoma: A case series. Korean J Ophthalmol 2010;24:1:47-52. doi: 10.3341/kjo.2010.24.1.47. Epub 2010 Feb 5.





