Here, I’ll summarize some of the key issues relating to hypotony and offer suggestions for how best to manage it when it occurs.
Defining Hypotony
Hypotony can be defined either statistically or clinically. The statistical definition of hypotony is an intraocular pressure less than 6.5 mmHg (although the specific number depends on which source you consult). What really matters is the clinical definition: an IOP that’s low enough to cause clinically significant complications such as vision loss. The primary cause of these complications is hypotony maculopathy—low intra-ocular pressure associated with fundus abnormalities such as chorioretinal folds, optic nerve edema and vascular tortuosity.
The reported incidence of hypotony ranges from less than 1 percent of cases to 32 percent. The reason the range is so broad is that the amount of hypotony triggered by the surgery is greatly affected by factors such as surgical technique and the way mitomycin-C is used. For example, the Tube Versus Trabeculectomy Study reported a 13-percent rate of hypotony. That was undoubtedly partly a result of using an MMC concentration of 0.4 mg/ml—which is on the higher end of MMC concentrations—and applying it for four minutes using pledgets. In the Collaborative Initial Glaucoma Treatment Study, the reported percentage of hypotony was 9 percent; the antifibrotic agent used in that study was 5-fluorouracil. I inject 0.1 cc of 0.2 mg/ml of MMC into the sub-Tenon’s layer at the start of the trabeculectomy procedure, rather than applying it with sponges. I find this method to be efficient, with similar or better outcomes, and it’s not associated with an increased rate of hypotony. (My current rate of hypotony ranges between 3 and 5 percent.) Hence, the amount of hypotony you encounter will depend at least partly on your technique, the amount of MMC you use and how long you apply it. Of course, other factors such as the nature of your patient population can also influence your hypotony rate.
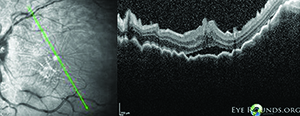 |
| Hypotony following trabeculectomy that is not addressed can lead to hypotony maculopathy (above)—low intraocular pressure associated with fundus abnormalities such as chorioretinal folds, optic nerve edema and vascular tortuosity. |
Hypotony that occurs more than two weeks after surgery, or late hypotony, may be secondary to an ischemic, avascular, thin bleb or overfiltration by the bleb. Late hypotony is usually more serious than early hypotony, and the prognosis for visual recovery depends on its duration. It becomes a cause for concern if it exceeds more than six months, since progression beyond that time frame may result in irreversible chorioretinal fibrosis.
Hypotony can be caused by either increased outflow of aqueous or by decreased aqueous production. Increased outflow could indicate overfiltration of the bleb secondary to loose scleral flap closure, or a leaking bleb. Other possibilities include cyclodialysis cleft, ciliochoroidal detachment, rhegmatogenous retinal detachment and trauma, although these are uncommon.
Decreased aqueous production can be secondary to a number of issues: iritis or iridocyclitis; ocular ischemia, where you have hypoperfusion of the ciliary body; pharmacologic aqueous suppression caused by the patient continuing to take a glaucoma medication such as timolol or Cosopt in the surgical eye unbeknownst to you, or a possible crossover effect from medication being used in the contralateral eye; tractional ciliary body detachment; rhegmatogenous retinal detachment; cyclodialysis cleft; or chemical toxicity to the ciliary body from antimetabolites like 5-FU or MMC. Some of these can be unintentional consequences of the trabeculectomy surgery.
Managing a Bleb Leak
One issue when a patient appears to be developing hypotony is deciding when to intervene. Certainly you need to intervene if the patient is having visually significant symptoms—if vision is deteriorating as a result of the low pressure. Other considerations include the possibility of endophthalmitis or imminent risk of bleb failure if the patient has a persistent bleb leak. Choroidal effusion can lead to visual impairment or persistent ocular pain, as well. The specific response to hypotony depends on the cause and the extent of the problem. An extremely low pressure, for example, may call for a different response than a moderately low pressure.
If the cause of early hypotony is a bleb leak, I begin by trying a few conservative measures, in particular a bandage contact lens and an aqueous suppressant, assuming the pressure is not already extremely low. Although using an aqueous suppressant to manage a situation relating to hypotony may sound counterintuitive, it can help address the cause of the low pressure by relieving the pressure inside the bleb and reducing flow through the leak, giving it a chance to heal. So, if I put on a bandage lens to tamponade the leak, I usually also have the patient use timolol or brimonidine. (I don’t always combine the contact lens with a suppressant; I may try one or the other, depending on how the patient responds.)
Needless to say, if the pressure is very low—say, 2 mmHg—I wouldn’t use an aqueous suppressant. In that situation I’d try a contact lens first and cover the area with a non-epithelial-toxic antibiotic, preferably a fourth-generation fluoroquinolone, to prevent an infection. Some surgeons believe that using an antibiotic such as gentamicin may serve as a mild irritant, stimulating epithelial cells to proliferate and seal the leak.
Other options to address the leak would include fibrin tissue glue, argon laser and direct suturing of the conjunctiva. (I rarely have to resort to these alternatives.) If none of these approaches work to resolve an early leak, I move on to surgical treatment.
Late-onset Leakage
The main surgical management for late-onset bleb leaks, which I use very often, is excision of the avascular, ischemic bleb followed by advancement of surrounding healthy conjunctiva or an autologous conjunctival graft. If the affected area of the bleb and the amount of excised tissue is large, there may not be enough tissue for conjunctival advancement, and an autologous conjunctival graft (usually harvested from the inferior bulbar conjunctiva) may be performed. Generally, the bleb is leaking because the tissue on top of it is not healthy. Ideally, during the repair you want to avoid disturbing the filtration that’s happening underneath.
Of course, the risk here is that the new bleb will scar down. I tell these patients: Your pressure is 4 mmHg now, because you’re leaking. Once I fix this, there’s a very good possibility that your pressure will go up again and you may need another glaucoma surgery or medication. But we do need to fix the leak; in addition to hypotony maculopathy, leaving a leak unrepaired leaves you vulnerable to infection.
In some cases, you may want to resuture the scleral flap, either by taking down the conjunctiva, suturing the flap again, and then bringing the conjunctiva forward, or by doing a transconjunctival revision—placing sutures into the flap through the conjunctiva. You would employ this technique if there is overfiltration secondary to loose scleral flap sutures or if the sutures were cut too early in the postoperative period.
Some clinicians try to address a late-onset leaking bleb using an autologous blood injection. Basically, this means taking blood from the patient and injecting it into the bleb. The theory is that the fibroblasts in the blood can cause a transformation in the Tenon’s capsule that leads to scarring. Some patients are attracted to this option because they may avoid the need for surgical revision in the operating room if they end up on the winning side of the “coin toss” (the 50/50 success rate). I usually proceed directly to a more definitive surgical repair of the problem. I think if you’re going to address a bleb leak you might as well do something that will give you a higher success rate.
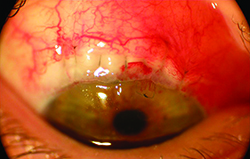 | 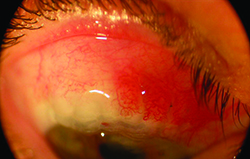 |
| Compression sutures used to manage overfiltration hypotony four months after a trabeculectomy. Left: One day after the placement of compression sutures. The sutures were removed one and three weeks after placement. Right: three months after suture placement. At this point the patient’s pressure had improved from 3 mmHg to 15 mmHg. | |
Another good option for addressing a bleb leak is compression sutures, which I discuss below.
Managing an Overfiltering Bleb
In some cases, when the cause of hypotony is an overfiltering bleb, non-surgical management approaches such as cycloplegia using atropine or Cyclogyl may be worth trying. If there is a shallow anterior chamber secondary to the overfiltration, the cycloplegic agent will move the lens iris diaphragm back and help the ciliary body restart the production of aqueous.
Some clinicians believe that if overfiltering happens in the early postoperative period it may be effective to taper the anti-inflammatory medications, like NSAIDs and steroids; this may facilitate faster episcleral scarring so you don’t get as high a bleb. Some will also try an autologous blood injection, as described above. Unfortunately, my experience has been that these methods are probably not going to work. Sooner or later you’ll have to resort to surgical management.
One of the most effective surgical ways to manage an overfiltering bleb is to use compression sutures. In fact, compression sutures are an excellent option whether your bleb is overfiltering or has a leak. Compression sutures tamponade the tissue in order to prevent fluid from moving past the suture. If a leak is in the periphery of the bleb, for example, Paul Palmberg, MD, has demonstrated that a compression suture can be used to wall off that section of the bleb. Meanwhile, the rest of the bleb is functioning normally, giving it a chance to heal.
Marlene Moster, MD, uses a slightly different technique, mostly for overfiltering blebs, that was initially published by Judith Eha, MD.1 In this variation you take several radial interrupted sutures (10-0 nylon 7707 Ethicon suture) and put them all the way through the full-thickness scleral flap. The suture pass starts at the limbus and goes through the conjunctiva, through the full-thickness sclera, and then out again through the conjunctiva. By suturing these layers very tightly together, you bring down the profile of the bleb; at the same time, you’re tamponading the bleb because you’re suturing through the flap.
One of the nice things about this technique is that if you use multiple compression sutures, the sutures can be selectively removed. For instance, suppose you put 10 sutures through and the pressure rises from 3 mmHg to 40 mmHg. You can remove two sutures and reassess the pressure. This elegant approach is less involved than a full bleb revision, and also provides you with some room to maneuver, thus providing a more gradual tapering of pressure.
I recently published a prospective case study of 15 patients with my colleagues Drs. Jesse Richman, Marlene Moster and Thandeka Myeni.2 Hypotony was reversed in 100 percent of cases and all but two patients (87 percent) achieved success, as defined in the study. They started out with a mean pressure of 3.3 mmHg and visual acuity of 20/150; after one year their mean IOP was 10.4 and vision improved to 20/30. (Additional surgery was necessary in two patients for elevated IOP post-procedure.)
A video showing this technique can be seen at https://youtu.be/v4i2ROPh7MA on the Web.
Management Tips
These strategies will help ensure that hypotony doesn’t become a serious problem for you or your patient:
• Err on the side of tighter sutures, not looser. You can always open your sutures with laser suture lysis or remove them, if you’re doing releasable sutures. On the other hand, if you make the sutures too loose at the outset you may end up with hypotony, which is much more difficult to fix.
• Try using the modified Wise technique for conjunctival flap closure. Gary Condon has popularized this technique, originally described by Dr. James Wise.3 This technique involves making an incision at the limbus to create a fornix-based flap. The incision may be at the limbus or about 1 mm posterior to the limbus, while leaving an anterior lip of the conjunctiva to act as a bolster for watertight closure. After the filtration portion of the procedure is done, you use a minimally spatulated needle, either with a 9-0 monofilament vicryl Ethicon suture (D8760), a 8-0 braided vicryl TG140-6 suture (the more affordable version), or a 9-0 vicryl suture on a BV needle—probably the most commonly used—to close with a running mattress suture. You make multiple passes in the conjunctiva and the sclera using suture bites that are longer than the space between the bites, anchoring the suture at both ends in the conjunctiva and sclera outside the confines of the incision. This ensures that you don’t have any breaks at the limbus, especially when doing a fornix-based flap.
The learning curve associated with this technique is steep; however, once you’ve learned to do it, it’s quick and efficient and always reproducible. I’ve had no bleb leaks since adopting this technique. I’ve also found that this technique minimizes astigmatic distortion. (You can watch a video illustrating this technique at https://youtu.be/nsKMjvbVuAo.)
• If there’s a potential problem, have the patient return frequently. In general, if a patient has hypotony, seeing the patient every couple of days is reasonable. If there’s no initial indication of a problem, I usually see patients on the first postoperative day, and at the first and second weeks. Then, depending on how they do, I’ll see them two weeks later and then a month after that. As long as there’s no sign of trouble, I keep lengthening the time between visits.
• Be patient with the pressure in the early postoperative period. You want to aim for a pressure between 15 and 20 mmHg, but I always tell my patients not to get too excited about the initial number. The initial postoperative period is a roller coaster, so the number matters less, as long as it doesn’t get too far out of the 15 to 20 mmHg range. But if the patient comes in on the first postoperative day and the pressure is 5 mmHg and her vision is blurry and she has choroidals—which is rare on the first day—then I would say, “Let me see you tomorrow or the day after. Let’s try this conservative treatment with steroids and atropine and see how you do.”
• If the patient has both an overfiltering bleb and a cataract, cataract surgery may resolve the bleb problem. In this situation, doing the cataract surgery may help address the overfiltration by inducing episcleral inflammation. It’s the same principle as tapering the patient’s anti-inflammatory medications. So if the patient has a cataract that is out of the immediate postoperative window, cataract surgery may induce some scarring, which will treat the hypotony and improve visual acuity.
• Remember that not all hypotonous eyes require intervention. The condition of the patient’s vision should always guide treatment, and the timing of any intervention should depend on the severity of the symptoms, patient preference and the status of the fellow eye. For instance, if you have a 90-year-old Caucasian female with a pressure of 3 mmHg, a diffuse filtering bleb and 20/25 vision, the most you should offer in terms of intervention would be the use of a plastic shield at night and having the patient sleep on the opposite side. On the other hand, if you’re dealing with a 20-year-old myopic Asian male with low scleral rigidity, a pressure of 6 mmHg and 20/400 vision, immediate intervention will proably be needed. REVIEW
Dr. Trubnik is an attending surgeon at Ophthalmic Consultants of Long Island in New York.
1. Eha J, Hoffmann EM, Wahl J, Pfeiffer N. Flap suture--a simple technique for the revision of hypotony maculopathy following trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol 2008;246:6:869-74.
2. Richman J, Moster MR, Myeni T, Trubnik V. A prospective study of consecutive patients undergoing full-thickness conjunctival/scleral hypotony sutures for clinical ocular hypotony. J Glaucoma 2014;23:5:326-8.
3. Wise, JB. Mitomycin-compatible suture technique for fornix-based conjunctival flaps in glaucoma filtration surgery. Arch Ophthalmol 1993;111:992-997.






