Here, I’d like review some of the recent clinical data regarding hysteresis, discuss possible explanations for what is actually being measured and talk about how measuring corneal hysteresis may be a significant aid when caring for glaucoma patients and suspects.
What Are We Measuring?
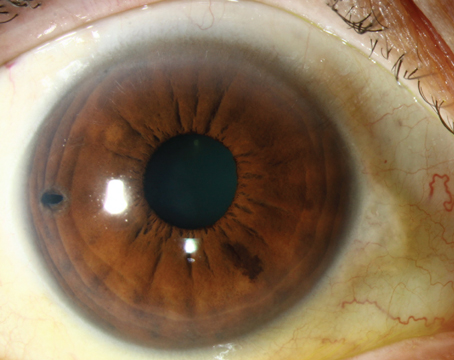
A good place to start is by asking the question: When we measure hysteresis, what exactly are we measuring? Technically, hysteresis is defined as the difference between the pressure at which the cornea bends inward during an airjet applanation and the pressure at which it bends out again. (See diagram, facing page.) It’s thought that this difference, which is measured in mmHg, gauges a bio-mechanical property of the cornea relating to its elasticity—specifically, the cornea’s relative ability to absorb pressure by bending when pressure is applied.
Given this specific definition of hysteresis, it can currently only be measured by the Ocular Response Analyzer. However, there’s another device produced by Oculus, called the Corvis ST, which like the ORA device uses an airjet tonometer to measure pressure. Unlike the ORA, it uses a high-speed Scheimpflug camera to monitor the cornea while the pres-sure is being measured, and it can calculate all sorts of other parameters. Essentially, like the Reichert instrument, it’s trying to measure the biomechanical properties of the cornea.
|
Thickness and Hysteresis
As you know, corneal thickness has become important in the management of glaucoma. Given that both thickness and hysteresis are corneal factors, comparing their histories, uses and interaction provides some interesting insights into the nature and value of hysteresis.
Corneal hysteresis and corneal thickness share some interesting parallels. Ophthalmologists became interested in corneal thickness ini-tially because it was thought to be a factor that interfered with our ability to accurately measure IOP, particularly when using Goldmann applanation tonometry. (The Gold-mann technology was developed with the assumption that corneal thickness was relatively constant from one person to the next, which turned out not to be the case.) To our surprise, studies like the Ocular Hypertension Treatment Study re-vealed that corneal thickness was an independent risk factor for glaucoma progression. For example, a drop in 40 µm of corneal thickness equates with about a 70-percent higher chance of developing glaucoma. That means that a thicker cornea may be more than sufficient to offset the risk associated with a higher pressure. A person who has a pressure of 30 mmHg with a corneal thickness of 600 µm has half the glaucoma risk of someone who has a pressure of 20 mmHg—10 mmHg less—if that person also has a corneal thickness of 500 µm. In other words, in terms of glaucoma risk, the cornea is just as important a factor to consider as the IOP.
In certain respects, our under-standing of corneal hysteresis has followed the same path as corneal thickness. Researchers were interested in hysteresis initially as a means to help doctors more accurately measure IOP. That work was fruitful; for example, some of the early work demonstrated that when IOP was adjusted for hysteresis it would measure the same before and after LASIK—not the case with methods such as Goldmann tonometry. As a result of that data, they began to recommend the Ocular Response Analyzer as a way to accurately measure IOP. Ironically, that may have ended up being a distraction, because like corneal thickness, most of the accumulating data is showing hysteresis to be a risk factor for glaucoma—even a more significant risk factor than corneal thickness.
This raises the question: Are corneal thickness and hysteresis related? They do correlate to a small degree, but they are definitely not the same thing. Some people have thick corneas and low hysteresis; other have the reverse. However, both go down with age. Furthermore, in a study I conducted, we found that African Americans and Hispanics have lower hysteresis than Caucasians.1 In the OHTS study, one of the main factors that accounted for glaucoma risk in blacks was a thin cornea; it turns out they have lower hysteresis as well.
| ||||
The measurement of corneal hysteresis has been slow to be adopted clinically compared to a corneal parameter such as pachymetry. However, corneal pachymetry was quickly adopted for several reasons that haven’t applied to hysteresis. For one thing, the largest glaucoma study (the OHTS, which involved 1,600 patients) validated pachymetry’s clinical use-fulness. For another thing, devices that measure pachymetry are often portable and relatively inexpensive, and pachymetry measurements can be performed by many devices using several techniques. That made it easier for people to start measuring corneal thickness, get comfortable with it and eventually adopt it into their practices.
The Progression Connection
One of the most important things we’ve learned about hysteresis is that a low hysteresis correlates with a greater risk of glaucoma progression. Several studies have confirmed this association. A study by the Chinese University of Hong Kong’s Nathan Congdon, MD, and Wilmer Eye Institute’s Harry Quigley, MD,2 as well as a paper by New York University Medical Center ophthalmologist Gustavo deMoraes,3 showed that patients with lower hysteresis were more likely to have progression, as evidenced by visual fields. Also, I recently completed a study that showed that having a lower hysteresis was also associated with progression in terms of optic nerve damage.4
Corneal thickness has been tied to risk of progression, but in the three studies mentioned above that compared hysteresis and corneal thickness, hysteresis has turned out to be a more powerful predictor of progression. All three of those studies were large and had significant numbers, although they were all retrospective studies, which means that technically, hysteresis was associ-ated with progression rather than be-ing an established risk factor.
To be able to define something as a risk factor, you have to collect the hysteresis first and then follow patients for four years or so. Drs. Felipe A. Medeiros, MD, PhD, and Robert N. Weinreb, MD, of the University of California, San Diego, recently conducted such a prospective study, involving 114 eyes of 68 patients.5 They collected hysteresis at baseline and then followed the patients for an average of four years so they could determine whether or not hysteresis was a risk factor for glaucoma progression. They found that visual fields of patients whose hysteresis was 4 mmHg or lower tended to degrade at a faster rate; also, the patients with low hysteresis and high pressures were at the greatest risk. Furthermore, hysteresis accounted for three times as much of the progression as corneal thickness.
Interestingly, one of the strongest and most consistently demonstrated risk factors for progression in all of the literature is age. And sure enough, as you age, your hysteresis score drops. In fact, if you take the patient’s age into account in some of these studies, the hysteresis effect is a little bit weaker, although it’s still present. So there is some interplay between age and hysteresis.
The IOP Connection
One important difference between hysteresis and corneal thickness is that corneal thickness is almost always very similar, if not identical, between the two eyes; it doesn’t change very much based on your eye pressure. In contrast, hysteresis will often vary, and it does change when IOP changes. For example, hysteresis is lower when an eye has higher pressure, so starting a patient on a drop should both lower her pressure and raise her hysteresis a little bit. Corneal hysteresis is not an inherent property of a cornea; it’s more like a behavior.
The fact that IOP and corneal hysteresis interact is both potentially helpful and harmful from a clinical standpoint. Because it can change so readily, it may not be as repeatable a measurement. On the other hand, we may get more information from measuring it once we know why it’s higher one day and lower another day. In fact, the interplay between IOP and hysteresis suggests to me that hysteresis might be useful as a clinical target. At some point it is conceivable that we may be focusing on trying to get our patient’s hysteresis to a particular level, just as we now try to do with IOP.
|
The Medication Effect
Another fascinating fact relating to hysteresis is that it can give you some idea of how much a person’s pressure will come down when you start him on an eye drop. In one recent study we found that if a patient has a very low hysteresis, for example 7 mmHg, putting him on a medication might produce a 29-percent pressure reduction. But if the patient has a high hysteresis, such as 11.9 mmHg, that patient would only get 7.6-percent pressure reduction from the same medication.6 (See charts, p. 55.)
Knowing this could be helpful, because sometimes when the pressure doesn’t come down we’re tempted to start the patient on a second drop. If you know the patient has a high hysteresis, you know that the patient has a lower risk of progression—and, you know that you may not see a big pressure drop when you start a new medicine. In this situation, I can take a step back; instead of adding more drops, I’ll just watch the patient and see if he progresses. Conversely, when a patient with a low hysteresis has a nice pressure response to a new drop, that’s good news; but you can’t let your guard down. The low hysteresis means the patient is at greater risk, so you still have to watch him carefully.
We set target pressures all the time, but the patient’s cornea will actually tell us a lot about whether the patient will get to that target. Knowing that you might not need to add the extra drop is important because adding a drop punishes the patient; it’s tough on the patient’s lifestyle and tough on the eyes. You don’t want to add a drop unless you really have to.
Incidentally, you might suspect that this difference in response to medication could be explained by the drop penetrating the cornea more or less effectively when the hysteresis is low or high. However, the data indicates otherwise, because the same association was recently found with selective laser trabeculoplasty.7 Sixty-eight eyes had laser trabeculoplasty; the eyes were checked for both hysteresis and IOP. On average the SLT reduced the pressure 23 percent; but if you looked at who had the best response, those with higher pressure and lower hysteresis did the best. Those two factors accounted for 64 percent of the variability in pressure lowering.
So, hysteresis not only tells us something about a patient’s risk of progressing, it also tells us a little bit about who might respond well—or not respond as well—to a drop (or to SLT).
One Possible Explanation
Obviously, all of this raises some important questions. What’s happening in the cornea that produces a high or low hysteresis measurement? And how does the level of hysteresis increase or decrease the risk of glaucomatous progression?
Currently, we have no clear answers, only theories. One theory is that having a high corneal hysteresis is like having an eye that’s a good shock absorber, for lack of a better term. When pressure is applied to a shock absorber, the shock absorber caves in a little to accommodate the increase in pressure. So an eye with high hysteresis may be more flexible, perhaps handling pressure more adroitly than a less-flexible eye with a lower hysteresis score, much like a flexible tree bending in the wind while a less-flexible tree is blown over and uprooted.
| |||||||||||||||||||||||||||||||||||||||||||||
Furthermore, consider the fact that hysteresis drops when the intraocular pressure gets very high. That makes sense because an eye that has a high pressure is already under stress; it’s already used up its ability to absorb energy or pressure. That eye, with its reduced flexibility, may be more susceptible to nerve damage. Conversely, when you lower the pressure, hysteresis increases; you’ve taken some stress out of the system. Now it has more absorbing capability again. Again, this is still theoretical.
Here’s another way to think about this: Instead of giving us a simple reading of the pressure inside the eye, hysteresis may be telling us about the pressure the eye is experiencing. It’s a bit like when my son and I carry our backpacks. He’s lifting a lighter backpack, but it’s heavier relative to his strength; so it feels heavier to him, and he’s going to get tired sooner.
Knowing that bit of information might be far more useful in the real world than simply knowing the weight of the backpack. In other words, hysteresis may allow us to treat each eye as a unique entity. We already know that some eyes can handle high pressure and others can’t; hysteresis might be the key to figuring out which ones are which. And all the data is consistent with that idea.
Hysteresis in the Clinic
So: How might a clinician use this measurement in practice to improve the care of glaucoma suspects and patients? As a clinician who has taken this measurement for several years, I can say that it does make a significant difference in my treatment decisions, and it’s pretty easy to incorporate it into your routine.
Certainly, hysteresis tells me about a patient’s risk, just as a thinner or thicker cornea does. A patient whose hysteresis is lower than, say, 9 mmHg is at greater risk of progression. If a patient has a higher hysteresis, I worry less, even if his pressure is elevated.
Hysteresis is helpful in glaucoma suspects because if the eye looks more cupped, has questionable nerve health or a suspicious visual field, and the hysteresis is lower in that eye, I see that as a pretty good evidence that the patient is at risk. The only thing I know of that connects an abnormal-looking nerve and low hysteresis is glaucoma. Notably, hysteresis is much more helpful in this situation than corneal thickness, because it’s been shown that eyes with worse damage than the fellow eye will also have lower hysteresis than the fellow eye. In contrast, corneal thickness is almost always the same between the eyes, regardless of the levels of damage.
The interplay between hysteresis and medication response is also very clinically useful. Knowing a patient’s hysteresis affects my expectations regarding how much of a pressure drop an eye will achieve on a new medication. For example, if a patient’s hysteresis is high and his IOP doesn’t drop much as a result of starting a medication, I know that this may be partly explained by the hysteresis. The medication is probably working better than it appears to be; I just can’t measure it through the patient’s cornea, which is absorbing so much energy. That realization prevents me from being hasty about starting the patient on an additional drop.
When a patient is at greater risk, I treat a low hysteresis the way I might treat a disc hemorrhage. It doesn’t lead me into the operating room, but it may lead me to see the patient in three months instead of six. It may cause me to get two or three visual fields a year instead of just one. And it reminds me to make sure that I have all the information I need in case this patient does progress, including a picture of the optic nerve, visual fields and OCT data. If I have that high-quality information, I’ll be able to detect the progression. (In fact, that’s where the ball often gets dropped when managing glaucoma patients. We identify risk, but if we haven’t been following the patient carefully, when he does progress we won’t have confidence that the progression is real. Maybe the patient’s first visual field wasn’t high-quality and we neglected to repeat it; now we can’t tell if we’re seeing fluctuation or true progression. If we had just gotten more high-quality visual fields over a two-year period, we’d know.)
Hysteresis is also important when managing normal-tension glaucoma patients. In a study I conducted with New York City ophthalmologist Mitsugu Shimmyo, we found very low hysteresis in normal-tension glaucoma patients.9 In that study we were looking at corneal-compensated IOP, i.e., pressure adjusted for hysteresis. After making that correction, we found that the normal-tension glaucoma patients actually had very high pressure. And the difference in pressure reading produced when this factor was taken into account was significantly greater in these patients than in high-tension patients or normals.
| ||||||
Put another way, some normal-tension glaucoma patients may not have normal tension at all.
Practical Realities
Undoubtedly, one factor that has contributed to a very slow adoption of clinical hysteresis measurement is that it’s not currently reimbursed by Medicare. In an ideal world that wouldn’t matter, but doctors are hesitant to spend money on a device that will not be reimbursed. There is currently a tracking code for the measurement of corneal hysteresis (0181t), and it is reviewed by the Food and Drug Administration from time to time, so at some point it could become a standard code, allowing physicians to be reimbursed.
One interesting side effect of measuring hysteresis is that it often provides evidence that our previous analysis of a patient’s situation was not accurate. That’s fine if it indicates that the patient is not actually in as much danger as you thought; but if you start measuring corneal hysteresis, you’re going to find that some patients are at much greater risk than you had previously recognized. That can be discouraging.
Nevertheless, measuring corneal hysteresis can be profoundly useful in the assessment of an individual’s glaucoma risk, and it also provides an objective measurement of IOP. You don’t have to worry about your technician having a bad day or be concerned that your hopes for this patient’s pressure are biasing your measurements. With the ever-mounting evidence supporting the value of corneal hysteresis, I feel certain that one way or another this test will become incorporated into our standard clinical routine. And when it is, I believe it will change the way we practice.
Of course, we still don’t understand exactly what it is we’re measuring when we measure hysteresis. But as a doctor treating glaucoma, I’m ready to say that I’m not too concerned about what specific characteristic this measurement actually represents, because whatever it’s measuring is meaningful. It’s giving me important infor-mation about my patients’ risk of progression, which has been validated by a number of well-executed, independent studies.
For that reason, I think we need to avoid becoming bogged down in the question of whether hysteresis is measuring viscous dampening or elasticity. For now, we can just note that it’s measuring something that’s important for glaucoma. We should start using it and learn more about it as we go along. REVIEW
Dr. Radcliffe is an assistant pro-fessor of ophthalmology at Weill Cornell Medical College in New York City. He has no financial ties to Reichert or the Ocular Response Analyzer.
1. Haseltine SJ, Pae J, Ehrlich JR, Shammas M, Radcliffe NM. Variation in corneal hysteresis and central corneal thickness among black, hispanic and white subjects. Acta Ophthalmol 2012;90:8:e626-31.
2. Congdon NG, Broman AT, Bandeen-Roche K, Grover D, Quigley HA. Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol 2006;141:5:868-75.
3. De Moraes CV, Hill V, Tello C, Liebmann JM, Ritch R. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012;21:4:209-13.
4. Vu DM, Silva FQ, Haseltine SJ, Ehrlich JR, Radcliffe NM. Relationship between corneal hysteresis and optic nerve parameters measured with spectral domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 2013;251:7:1777-83.
5. Medeiros FA, Meira-Freitas D, Lisboa R, Kuang TM, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology 2013;120:8:1533-40.
6. Agarwal DR, Ehrlich JR, Shimmyo M, Radcliffe NM. The relationship between corneal hysteresis and the magnitude of intraocular pressure reduction with topical prostaglandin therapy. Br J Ophthalmol 2012;96:2:254-7.
7. Hirneib C, Sekura K, Brandlhuber U, Kampik A, Kernt M. Corneal biomechanics predict the outcome of selective laser trabeculoplasty in medically uncontrolled glaucoma. Graefes Arch Clin Exp Ophthalmol 2013;251:10:2383-8.
8. Wells AP, Garway-Heath DF, Poostchi A, Wong T, Chan KC, Sachdev N. Corneal hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patients. Invest Ophthalmol Vis Sci 2008;49:8:3262-8.
9. Ehrlich JR, Radcliffe NM, Shimmyo M. Goldmann applanation tonometry compared with corneal-compensated intraocular pressure in the evaluation of primary open-angle Glaucoma. BMC Ophthalmol 2012;12:52.