“Ophthalmology was the first medical field to use microscopes in surgery. We have had a long and illustrious marriage with the technology,” says Robert M. Kershner, MD, MS, FACS, professor and chairman of the Department of Ophthalmic Medical Technology at Palm Beach State College, and a consultant specialist in cataract and refractive surgery in Palm Beach Gardens, Fla.
He notes that there were few advancements for about 30 years, but then surgery changed and demanded more of the microscopes than they were capable of. “We discovered that the bright illuminators caused macular burns, so rheostat-controlled and less intense filaments were utilized to reduce injury and still provide a bright red reflex,” he says. “First, they had to become portable, as the surgeon moved between operating rooms and the high cost mitigated against purchasing more than one. Microscopes went from large, heavy, ceiling-mounted scopes (and those of us who used them still have the scalp bruises to prove it) to smaller and lighter scopes mounted on a moveable base. The arms needed to be longer to allow the scope to be positioned over the patient’s head to compensate for a base that was farther away.”
Today’s surgical microscope is sophisticated and offers a host of controllable options to provide the proper illumination and visualization that smaller microincisional techniques demand. However, ergonomics is still an area that needs improvement.
Eric Donnenfeld, MD, of Ophthalmic Consultants of Long Island, says one of the major upgrades that is already available in some microscopes is integrating the microscope into the surgical procedure. “Microscopes are becoming significant adjuncts to improve refractive cataract surgery,” he says. Here are some of the latest advances.
|
Alcon Laboratories acquired Endure Medical Systems, and, with that acquisition, added the LuxOR ophthalmic surgical microscopes to its product offerings. The LuxOR LX3 with Q-VUE ophthalmic microscope features the following proprietary technologies:
- • Q-VUE assistant visualization takes no light from the surgeon’s optical pathway.
• The ILLUMIN-I technology provides stable, high-quality red reflex that is six times larger than the red reflex zone created by conventional microscopes. It also provides premium visualization and detail recognition and contrast, along with penetrating depth of focus.
• The new LX3 floor stand features an electromagnetic clutch system for easy positioning, an ergonomic design that hides all cords and cables, a touchscreen video control and 360° base rotation with extra-long reach.
• AMP technology delivers more light to the surgeon during retinal procedures.
• The LIBERO-XY Communication System and Heads-Up Display provides easily accessible microscope feedback to the surgeon and touchscreen video control.
• The microscope is compatible with both the Cataract Refractive Suite and the Verion Image Guided System, which provides the digital marker and image-guided overlays of patient-specific data that can be viewed through the surgeon’s ocular.
• The microscope has video capabilities to capture still and moving images.
OPMI Lumera 700
This ophthalmic surgical microscope from Zeiss features Stereo Coaxial Illumination technology, which makes even fine anatomical details clearly visible. The red reflex is high in contrast and stable.
For retinal surgeons, the OPMI Lumera 700 and Resight 700 fundus viewing system allow recognition of every detail of the retina.
The microscope can be configured with Invertertube E, which facilitates an upright, ergonomic posture as well as rapid changeover from cataract to case surgery. A fully integrated HD video recording system includes a 1080p HD video recorder, which can be operated by the foot control panel or handgrip of the microscope head.
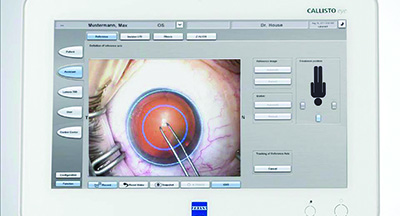
This microscope works seamlessly with the Callisto eye-assistance system. The Callisto Eye and Integrated Data Injection System allows surgeons to view visual assistance functions, such as incision and rhexis assistant and the toric intraocular lenses alignment feature Z Align, which are displayed directly into the eyepiece of the microscope.
It also includes an integrated assistant microscope that works with no light loss for the main surgeon. It features a zoom function that can work with the main surgical microscope or independently.
|
Richard Hoffman, MD, also uses the Lumera. “In the past five years, there has been the addition of wireless controls, so you don’t have cords all over the operating room floor,” he says. “The biggest thing that is happening is the integration of office devices with the operating microscope. For instance, the Callisto system can be added onto your operating microscope. When you are doing your IOL measurements using the newer model IOLMaster, the landmarks on the patient’s eye are registered and can then be transferred to the operating microscope. Because the microscope has that information in it, your limbal relaxing incisions can be placed exactly where you want them, and the toric IOLs can be aligned exactly where you want them. In the future, I think these microscopes are going to have wavefront aberrometry built into them as well.” Dr. Hoffman is a clinical associate professor of ophthalmology at the Casey Eye Institute at Oregon Health & Science University. He is also in private practice at Drs. Fine, Hoffman & Sims.
According to UCLA’s Dr. Miller, there is a similar product called the Cirle Surgical Navigator that is not being sold yet, but will be licensed through Bausch + Lomb. “It will provide a stereo heads-down display through an operating microscope. Like the Verion and Callisto systems, it will provide toric alignment and incision marks based on reference images obtained before surgery,” he says.
Allegra and Hi-R NEO
From Haag-Streit USA, the Allegra microscopes are designed for multidisciplinary use in hospitals and surgical centers. The Hi-R NEO 900 is designed for use in ophthalmology, and it delivers advanced red reflex and offers stereoscopic co-observation.
Additional equipment includes EIBOS 2, a new ophthalmoscope system for posterior segment surgery, and TOCULAR for toric lens alignment.
CellChek XL
The CellChek XL specular microscope system from Konan Medical is fully automated and features auto-align, auto-focus, auto-capture, auto-analysis, and auto-pachymetry. The patented capture method acquires data samples that include position data. This can allow accurate reassessment of the same specular data sample areas to trend cellular statistics over time.
M822 and M844 Microscopes
Leica Microsystems has several ophthalmic surgical microscopes to choose from. They feature a low-light concept, with direct halogen illumination and high-intensity transmission optics, which provide the necessary contrast ratio for retina procedures.
The coaxial double-beam stereo illumination and OttoFlex II provide a stable red reflex, even in patients who have anatomical conditions that make this difficult, such as small pupils. These microscopes are modular and expandable.
Two of Leica’s offerings are the M822, which is a red reflex surgical microscope, and the M844, which is its premium microscope.
The M844 is especially helpful for posterior and high-end anterior segment surgery. When this microscope is combined with the APO OptiChrome optics and direct halogen illumination, it offers optimal clarity, contrast and sharp, true anatomical color images at safer low-light levels. Features like the QuadZoom technology, the Double Wing Assistant Bridge, and HD recording make it especially useful for teaching institutions.
The M822 is a surgical microscope with enhanced red reflex, which enables precise and efficient cataract surgery. It achieves this with a unique illumination system that combines LED and halogen. It has an ergonomic design for intuitive control of the system. It also offers high-definition video, open architecture for easy integration of vitreoretinal accessories, and interchangeable floor stands.
TrueVision
This is a stereoscopic high-definition visualization system for refractive cataract, glaucoma, and retinal procedures that displays the surgical field of view in real time on a 3D flat-panel display in the OR. It enables the surgeon to operate in a heads-up manner by viewing a large screen instead of traditional microscope oculars.
“TrueVision provides surgical templates for the pupil, for the capsulorhexis and for the steep axis. It allows 3D visualization of the cataract procedure so that the incision can be done either through a microscope or through a heads-up display,” Dr. Donnenfeld says. “The quality of this imaging has improved so dramatically over the past five years that it’s rivaling what can be achieved through a surgical microscope directly. One of the nice things about these new 3-D microscopes is that they provide an incredible increase in depth of field so that you can judge depth in the eye more accurately and the distance between your phaco needle and the posterior capsule. Not only does it allow visualization during surgery, but it allows everyone in the operating room to have the same view as the surgeon for the first time. It provides a wonderful teaching tool in the OR as well as at meetings.”
He notes that LensAR has now partnered with TrueVision to provide 3-D video imaging with femtosecond laser cataract surgery, which is a new application.
According to Dr. Miller, the resolution and the visual quality of this system have come along in the last few years. “TrueVision integrates with the i-Optics Cassini topographer to provide many of the intraoperative capabilities of Verion, Cassini and Cirle,” he says. “The only negative with TrueVision, and it is minor, is that there is a lag of 100 milliseconds or so between what your hands are doing and what you see on the microscope.”
Dr. Miller believes that all microscopes will be digital in the future, because they provide capabilities that cannot be duplicated by optical microscopes. “The main problem with current digital microscopes is that the camera hangs on a traditional optical microscope, and the surgeon has hardware right in front of his or her face,” he says. “To look at the monitor, we have to look to the side, which is awkward. It’s like driving a car straight but having to look 30° to the right or left. Digital microscopes will become more compact, and ultimately the associated flat panel displays will be mounted on the other side of the patient’s head, where they belong.”
Oculus Wide-Angle System
The SDI/BIOM system from Oculus Surgical is used to observe the retina during vitrectomy procedures. The BIOM 5 is aligned coaxially with the operating microscope while observing the vitreous and the fundus. During the extraocular parts of the surgery, it can be moved out of the way of the observation beam while the inverting action of the SDI is neutralized. The BIOM 5c has electronic focus, and, when used with the SDI 4c, it offers the convenience of electronic foot pedal focusing and intelligent and automatic image inversion.
HOM-700
The latest addition to the marketplace is the HOM-700 by Coburn Technologies. This microscope streamlines all surgical workflow and maximizes surgical efficiency. Key features include the following:
- • A high-resolution optical system that provides enhanced images even in low-intensity illumination situations, enabling sharp, crisp, high-resolution 3-D observations.
• Fatigue-free surgery with a 10 x 21 mm visual field.
• An optimized halogen-illumination system that reduces shadowing in deep cavities, provides high quality illumination, and prevents heating and UV transmission.
• Optimized red reflex that allows instant and perfectly stable red reflex from the illuminator, providing the optimum brightness and observation angle.
• An optional high-resolution imaging system to capture high-quality videos and still images.
• A foot pedal control for hands-free surgery.
• A stable suspension stand.
• A built-in, rotatable, 7-in. color TFT LCD control panel.
• A straightforward GUI display.
• Custom settings to save and recall up to four surgeons individual parameters.
• Full compatibility with industry-leading peripheral lens systems.
According to Uday Devgan, MD, the next step is integrating biometry equipment into the actual microscope, such as aberrometers, keratometers, and more.
“These technologies are in their initial stages, and we can expect that every generation will get better,” says Dr. Devgan. “Intraoperative aberrometry now requires input of preoperative biometry, such as keratometry and axial length, but in the future, a truly accurate system would not require any preoperative IOL power calculations. The eye in its aphakic state would be measured, and then the appropriate IOL power would be determined on the spot.” Dr. Devgan practices at Devgan Eye Surgery in Los Angeles and is chief of ophthalmology, Olive View UCLA Medical Center, and a clinical professor at the Jules Stein Eye Institute, UCLA School of Medicine.
He notes that one challenge to improving the technology is the cost. “These new technologies can be very expensive,” he says. “Reimbursement from surgery becomes lower every year, so balancing the cost:benefit ratio becomes tougher for routine cataract cases. It’s imperative that patients understand that cataract surgery just fixes the cataract. If they want a specific refractive outcome, that falls under refractive surgery and services. When patients are willing to pay out of pocket to have a precise refractive outcome, we can use these new technologies to provide the very best vision.” REVIEW
Dr. Kershner has no financial interest in any of the products mentioned in this article. Dr. Donnenfeld is a consultant to Alcon, TrueVision and Zeiss. Dr. Miller is a consultant to Alcon. Dr. Hoffman is a consultant to Zeiss. Dr. Devgan is a consultant for Alcon and Bausch + Lomb.