Wavefront-guided or custom LASIK may be good for some eyes, but it is not appropriate for every eye. The marketing metaphor comparing custom LASIK to custom-tailored suits—"Off-the-rack suits may fit, but wouldn't you rather have a custom-made suit?"—ignores basic principles of optics, lasers and wavefront imaging.
Proper patient selection is the key to successful integration of custom LASIK treatments in your practice. In the right setting, custom treatments can improve night visual function, best-spectacle corrected visual acuity and patient satisfaction. Conversely, inappropriate use of custom LASIK may lead to higher enhancement rates, loss of BSCVA and increased medicolegal liability.
In my work with the Refractive Surgery Consultant Elite software, I have the opportunity to analyze outcomes with all the wavefront platforms (Alcon, Visx, WaveLight and Bausch & Lomb). Certain preoperative characteristics predict good custom LASIK outcomes, while others suggest that the patient may do better with standard LASIK based on a phoropter refraction.
In this article, I summarize my observations in four "rules" to help guide patient selection for custom treatments.
1. Manifest v. Aberrometer Refraction
The endpoint of a subjective manifest refraction is selected by the patient and is based on optical and psychological factors. The endpoint of an aberrometer-generated refraction is the mathematical average of the spherocylinder portion of the optical wavefront over the entrance pupil.
These two refractions may differ. If they differ, it is because the patient prefers a refractive endpoint that is different from the averaged wavefront. Any custom LASIK treatment will be based on the average refraction, so it will likely be the wrong endpoint for this patient. If the difference between the manifest and aberrometer refractions is greater than 0.50 D, convert to standard LASIK.
Note that most aberrometers calculate the spherocylinder refraction based on a 4-mm entrance pupil. This is done for two reasons. The first is to simulate the physiologic pupil size, which is about 4 mm under photopic conditions in most eyes. If your patient's photopic pupil is different from 4 mm, then have the aberrometer recalculate the spherocylinder refraction at the actual pupil size to obtain a more accurate comparison.
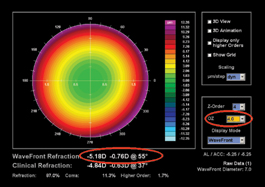
The second reason that aberrometers use a 4-mm pupil to calculate the spherocylinder refraction is to exclude higher order aberrations (See Figures 1 and 2). Since most higher-order aberrations exist in the periphery, using a 4-mm pupil prevents the calculated refraction from being affected by, say, large amounts of spherical aberration. The logic behind excluding higher-order aberrations from the calculated refraction is questionable, as studies have shown that they do affect the manifest refractive endpoint.1
 |
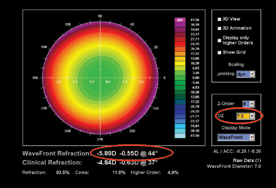 |
| Figure 1. Preoperative aberrometry in a myope with spherical aberration, demonstrating the effect of optical zone, which simulates the pupil size, in the calculated aberrometry refraction. The calculated refraction changes by - 0.71 + 0.21 D with a change in optical zone of 4 to 7 mm (red ovals). | |
Either way, a significant difference between the aberrometer and manifest refraction suggests that the refractive outcome from custom LASIK will be unsatisfactory to the patient. If the difference is more than 0.50 D, I recommend that you rely on the phoropter refraction and convert to standard LASIK.
2. Nomogram suggests sphere adjustment > 0.50 D.
Custom LASIK has not eliminated the need for nomograms. All lasers and surgeons are different and these differences persist regardless of the methods used to determine the refractive error to be treated, even with aberrometers. In fact, because the refractive error is being determined by a machine irrespective of surgeon judgment, the need for nomograms may be increased. A patient with a flat higher-order wavefront that is still blurry from residual spherocylinder error will not be happy.
While current technology precludes development of nomograms for each higher-order aberration, nomograms for sphere and cylinder are critical. Every surgeon must develop nomograms to independently adjust the sphere and cylinder treatment amounts for custom LASIK. These nomograms should consider the spherocylinder correction in the wavefront treatment as the "attempted" and the difference between the manifest postoperative and aberrometer refraction as the "achieved." Vector analysis should be used to quantify cylinder outcomes, and the analysis should consider the effect of concurrent sphere treatments on cylinder outcomes, and vice-versa, as previously described.2
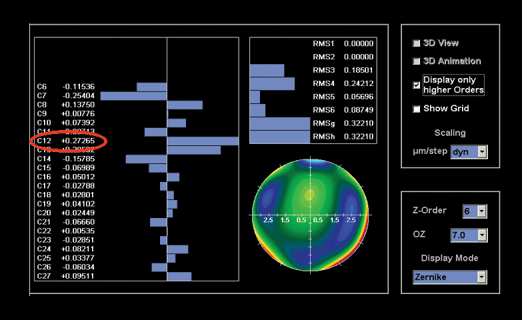 |
| Figure 2. Map of the higher-order aberrations for the eye shown in Figure 1, showing the large amount of spherical aberration. The coefficient for C12 in this map is + 0.273 (circled). |
Once nomograms are developed, they can be used to predict the outcome of custom LASIK treatments. Simply plug the spherocylinder refraction calculated by the aberrometer into the nomogram software. If the nomogram suggests modifying the sphere treatment amount by more than 0.50 D, then this eye may not do well with custom LASIK. Convert to standard LASIK.
Why? Even though most lasers will accept surgeon adjustments of the sphere treatment amount of up to 0.75 D, these adjustments only modify the sphere treatments, and do so by globally changing the defocus treatment. They don't modify treatments of all the other aberrations. If the sphere treatment requires that much modification to be accurate, then the other treatments probably do, also. Since the other aberrations cannot be nomogram-adjusted, the results will be unpredictable.
It is probably fine to make sphere adjustments of less than 0.50 D, but they should be done based on optimized nomograms based on prior results. You will find that sphere adjustments in custom LASIK vary based on concurrent cylinder treatments and other factors. To be valid, adjustments should be made using nomograms developed using proven methods.
3. Nomogram suggests significant cylinder adjustments.
Similar to sphere nomograms, cylinder nomograms based on prior custom treatments can be used to predict the cylinder outcome. Unlike sphere treatments, however, there is no surgeon adjustment of the cylinder treatment in custom LASIK, so the adjustment of the cylinder suggested by the nomogram predicts the residual cylinder to be expected after surgery. Also consider that if the nomogram suggests a smaller treatment amount than the aberrometer reading, the postop axis can be expected to be 90 degrees from the preop axis (flipped axis). Expressed differently: If this amount exceeds your comfort level, convert to standard LASIK using the nomogram-adjusted manifest refraction.
| Nomogram-adjusted cylinder treatment – Aberrometer cylinder amount _______________________________ = Expected postoperative cylinder |
4. Smooth topography with significant aberrations.
I have seen several data sets with increased rates of BSCVA loss with custom LASIK compared with prior results with standard LASIK. This may be due to the introduction of new aberrations on the cornea to compensate for lenticular aberrations.
If the topography is regular and shows few asymmetries but the aberrometry shows significant coma, then the aberrations are mostly in the lens. The custom LASIK procedure will put reciprocal aberrations in the cornea. Unless the postop optics align perfectly, this is likely to induce BSCVA loss. Convert these eyes to regular LASIK.
 |
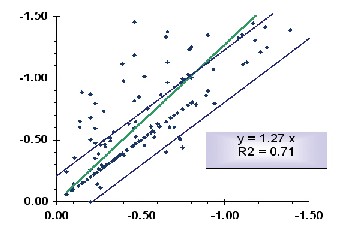 |
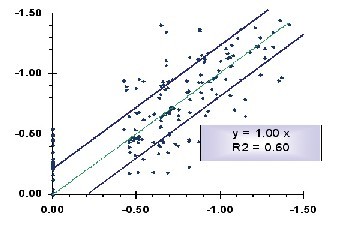
| Figure 3. Attempted vs. achieved cylinder plots contrasting the slope achieved with standard LASIK and custom (wavefront-guided) LASIK, in the same Alcon LADARVision laser by the same surgeon. This figure shows the tendency of the current LADARVision system to overcorrect cylinder and demonstrates that nomograms derived using data from standard treatments cannot be applied to custom LASIK. | |
As a final note, the practice of "tricking" the LADARVision custom system (Alcon) to allow you to treat more than the approved cylinder amount is to be avoided. Data show that the cylinder algorithm in the current LADAR software in some lasers overcorrects astigmatism by about 30 percent (See Figure 3). You should not treat cylinders over 0.5 D with the LADARVision system, or you may wind up with many flipped axes. I understand there is a new version that corrects this, but if you are not in the studies, you won't have it.
Careful patient selection is critical to the successful integration of custom LASIK treatments into clinical practice. These suggestions are not meant as a comprehensive guide but as a starting point to qualifying patients for custom treatments based on objective, rational criteria. Custom LASIK is not the best answer for every eye; for many, standard LASIK based on the manifest refraction will yield a better result.
Dr Kezirian is president of Refractive Consulting Group Inc., maker of the Refractive Surgery Consultant Elite software for refractive outcomes analysis and nomogram development, and is president of SurgiVision Consultants Inc., an ophthalmic consulting firm. Contact him at 2183 Hathaway Ave., Westlake Village, Calif. 91362. Phone: (805) 493-4200, fax (805) 493-4700, e-mail: Guy1000@Surgi Vision.net.
1. Holladay JT, Lynn M, Waring GO, Gemmill M, Keehn GC, Fielding B. The relationship of visual acuity, refractive error and pupil size after radial keratotomy. Arch Ophthalmol 1991;109:70-76.
2. Kezirian GM. LASIK Nomograms to Improve Outcomes. In: Probst LE, ed. LASIK: Advances, Controversies, and Custom. Thorofare, NJ.: Slack Inc., 2003.



