Michael Gordon, MD, in private practice in La Jolla, Calif., points out that approved and available treatments today are not ideal. “Today, we have poor attempts at doing presbyLASIK, particularly in the United States, because we are limited in how we use lasers,” he says. “We have presbyopia-correcting intraocular lenses, which are good but not perfect because we really don’t have any true accommodating IOLs. We have monovision with LASIK and monovision with IOLs, which is tried-and-true and has been around for a long time in many forms. I think it works very well, but it’s not the ultimate answer because a little bit of stereopsis and distance vision are lost.”
Understanding Presbyopia
Daniel Durrie, MD, in private practice with Durrie Vision in Overland Park, Kan., says ophthalmologists are changing the way they talk to patients about correcting presbyopia. “It has made it a lot simpler to come up with the best solution for each patient,” he says.
Dr. Durrie notes that presbyopia is part of dysfunctional lens syndrome, which has three stages. Stage 1 typically starts around 43 years of age and goes until the early 50s. During this time, the lens loses its ability to focus. In stage 2, which occurs during the 50s and 60s, the lens turns yellow and hazy. During this time, patients begin to experience night vision problems and need more light to read. The third stage, which typically doesn’t occur until the 70s, is true cataract formation.
“When we are evaluating someone who is having difficulty with reading glasses and bifocals, we really want to find out where he is in the stages of dysfunctional lens syndrome, and that helps us in coming up with a treatment,” Dr. Durrie says. “If it is obvious that someone is in late stage 2 or early stage 3, we are going to lean towards lens replacement surgery, because anything we do on the cornea isn’t really going to benefit them for very long. This discussion also lets patients know that presbyopia is a progressive condition. It is going to require lens replacement at some point in time. That has helped us look at the procedures of today as well as the procedures that are coming in the future and how we are going to fit them into practice.”
Corneal Inlays
|
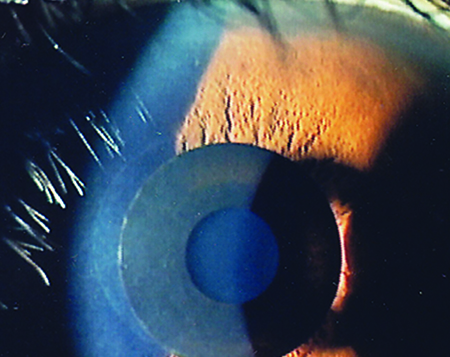
Richard Lindstrom, MD, in private practice in Minneapolis, says the Kamra inlay uses small-diameter aperture optics or pinhole optics. “Just as you would use a pinhole to improve someone’s vision in the office, this concept is used by this corneal implant or inside an IOL,” Dr. Lindstrom says. “It’s not a multifocal, and it’s not accommodating. Instead, it generates an increased depth of focus. This concept is used in disposable cameras that can take pictures at every distance. You target slight myopia. That along with the pinhole creates hyperfocality, which is widely used in the disposable camera industry. These patients see well at all distances. Typically, the inlay is only implanted in the nondominant eye. It looks very promising.”
Jay Pepose, MD, PhD, in private practice in Chesterfield, Mo., agrees. “The Kamra inlay is a neat concept because there is not as much disparity in uncorrected distance acuity between the two eyes as there is with full monovision, and there is not as much compromise in contrast sensitivity or stereopsis as there is with full monovision. Unlike LASIK, where permanent changes have been made to the eye, the inlay can be removed if the patient doesn’t like it or can’t adapt to it,” Dr. Pepose says.
In June 2014, the FDA Ophthalmic Devices Advisory Panel concluded that the benefits of the Kamra inlay outweigh the risks for patients with presbyopia. The panel reviewed data on 508 patients implanted monocularly with the inlay in the U.S. IDE clinical trial. In September 2014, the Kamra inlay received the CE Mark approval in Europe. It is not FDA-approved.
A study with three years of follow-up supports the safety and efficacy of the Kamra corneal inlay to correct presbyopia.1 This study included 32 naturally emmetropic presbyopic patients, and the corneal inlay was implanted in the non-dominant eye. Patients’ mean uncorrected near visual acuity improved from J6 preoperatively to J1 at three years, and the mean uncorrected intermediate visual acuity improved from 20/40 to 20/25 at three years. Additionally, at three years, 97 percent of eyes had an uncorrected near visual acuity of J3 or better, and 91 percent had an uncorrected intermediate visual acuity of 20/32 or better. The mean uncorrected distance visual acuity was 20/20, with all eyes achieving 20/32 or better. Nine eyes lost one line of corrected distance visual acuity, one eye lost more than two lines, and three eyes gained one line.
Another corneal inlay is the Flexivue Microlens (Presbia, Los Angeles). “This is a refractive inlay, meaning that the power can be changed because it is a different refractive index than the cornea,” Dr. Gordon says. He is an investigator for this inlay and says that it is in the initial stages of the Phase III clinical trial. “The results are extremely good. It is considered ‘smart’ monovision because vision will change depending on pupil size both at near and far; however, it is still a form of monovision. The advantage is that it’s an inlay that is very bioinert, so it can be removed or replaced as the patient ages, and a new power can be inserted.”
A recent study evaluating the efficacy and safety of the Flexivue Microlens found that, 12 months after implantation, the inlay seems to be an effective method for the corneal compensation of presbyopia in emmetropic presbyopes between the ages of 45 and 60 years of age. The study included 47 patients.2
The Raindrop corneal inlay, formerly known as PresbyLens, by ReVision Optics (Lake Forest, Calif.) is also currently under investigation. It is a microscopic hydrogel inlay that creates a prolate-shaped cornea and is easily placed under a femtosecond laser flap.
Scleral Implants
Another alternative to correct presbyopia is the VisAbility scleral implant (Refocus Group, Dallas). “VisAbility uses four small implants placed in scleral tunnels, 4 mm posterior to the limbus,” says Barrie Soloway, MD, director of vision correction surgery at the New York Eye and Ear Infirmary. “The VisAbility Implant System uses a scleral approach to treat presbyopia that is fundamentally different from the optical or multifocal approach. The hypothesized mechanism of action of the VisAbility surgery is a retensioning of the posterior zonules, giving the ciliary muscles more efficiency in reshaping the lens in these presbyopic patients.”
He notes that there are two advantages to this approach. First, surgery is well off the visual axis, so there are no changes in distance vision, such as problems with halos or glare, as might occur with most other approaches. “And, unlike bifocal laser or presbyopia-correcting IOLs, with VisAbility surgery, patients have a continuous range of focus from far through intermediate to near,” Dr. Soloway adds.
He says that results of this surgery in a recently completed FDA clinical trial were promising, with 96 percent of patients seeing J3, 20/40 or better uncorrected at near monocularly, and all were better still binocularly. “During the course of the study, a number of radically new instruments, including a docking station, were developed, which marked a quantum leap improvement in the consistency and ease of the surgery,” he says. “In Europe, where the CE-marked VisAbility Implant System is in use, surgeons report that their patients are having faster and better improvement in near and intermediate vision.”
FDA IDE clinical trials are currently under way in the United States, and enrollment of 360 patients at a dozen sites should be completed this year.
Laser Procedures
Laser procedures are not ideal for treating presbyopia, mainly because the results are not reversible. “Once you’ve done it, you’ve removed tissue in a complex pattern, which can be impossible to undo, not to mention how to measure these eyes for their lens replacement when they need cataract surgery,” Dr. Soloway explains.
|
Monovision with an excimer laser is one option. A study conducted in Spain found that this procedure improved functional near vision in presbyopic patients.3 However, although distance visual acuity was good, contrast sensitivity and stereoacuity diminished significantly. In this study, LASIK was performed with the Allegretto Wave Eye-Q 400-Hz laser. The dominant eye was corrected for distance vision, and the non-dominant eye was corrected for near vision by targeting -1.25 D of myopia. The study included 50 eyes of 25 patients with a mean age of 49.3 years ±4.5. Postoperatively, more than 90 percent of patients had a binocular uncorrected distance and near visual acuity of 0.0 logMAR or better. However, the contrast sensitivity function diminished, especially in the non-dominant eye and with binocular vision. All patients experienced significantly worse stereoacuity. Visual discrimination capacity declined in non-dominant eyes and under binocular conditions. No significant changes occurred in dominant eyes.
Another refractive surgery option is presbyLASIK. In a recent study of myopes and hyperopes, presbyLASIK using the MEL 80 platform induced significant changes in spherical aberration. This study concluded that presbyLASIK appears to offer an improved response over LASIK when correcting myopes due to an apparent increase in depth of focus resulting from changes in spherical aberration. Additionally, presbyLASIK provides a more consistent spherical aberration effect in hyperopes, independent of refractive change.4
Intraocular Lenses
For patients who have late stage 2 or stage 3 dysfunctional lens syndrome, lens replacement surgery is required. “In the United States, we are still limited to the big three: ReSTOR, Crystalens, and Tecnis multifocal,” Dr. Pepose says. “I think we will likely see low add powers of the Tecnis multifocal available in the United States in 2015. Right now, the Tecnis lens is a +4 add on the posterior IOL surface, which has the near focal point optimized around 32 cm. The lower powers would move the point of focus farther out. For some people, that would afford a more comfortable reading distance for a book or computer. Fewer rings may mean fewer photic phenomena.”
On the more distant horizon, there are some other lenses like the FluidVision accommodating lens by PowerVision, which has fluid-filled haptics that actuate a central curvature change in the lens with accommodative effort. “In Europe, there is the AkkoLens, where two lenses are sliding across with different optical features (spherical refractive and cubic),” Dr. Pepose says. “One of the most exciting lenses that I saw in Europe this year is the lens by AMO called the Symfony, which is an extended depth of focus lens. It’s a diffractive multifocal, and instead of having two foci, near and distance, it is spread out so that there is sort of a continuum of focal points. In order to offset the decrease in visual quality that you get by doing that, they offset the average corneal spherical aberration of the eye, and they also have offset chromatic aberration. This is a whole new class of lenses—extending depth of field lenses.”
“If we could get a truly accommodating IOL that is safe and effective, that would be a panacea. In certain age groups, this would be an excellent avenue to correct presbyopia,” Dr. Gordon adds. REVIEW
Dr. Durrie is a clinical investigator for AcuFocus. Dr. Gordon is an investigator and option holder for Presbia. Dr. Lindstrom has a financial interest in AcuFocus, AMO, Alcon and Bausch + Lomb. Dr. Pepose is a consultant for AcuFocus, AMO, Alcon and Bausch + Lomb. Dr. Soloway is the medical director of Refocus Group.
1. Seyeddain O, Hohensinn M, Riha W, et al. Small-aperture corneal inlay for the correction of presbyopia: 3-year follow-up. J Cataract Refract Surg 2012;38:35-45.
2. Limnopoulou AN, Bouzoukis DI, Kymionis GD, et al. Visual outcomes and safety of a refractive corneal inlay for presbyopia using femtosecond laser. J Refract Surg 2013;29:12-18.
3. Alarcon A, Anera RG, Villa C, Jimenez del Barco L, Gutierrez R. Visual quality after monovision correction by laser in situ keratomileusis in presbyopic patients. J Cataract Refract Surg 2011;37:1629-1635.
4. Gifford P, Kang P, Swarbrick H, Versace P. Changes to corneal aberrations and vision after Presbylasik refractive surgery using the MEL 80 platform. J Refract Surg 2014;30:598-603.