Lenses in Use
There are a few IOLs in use in the United States and/or abroad that may give increased depth of field without qualitative issues.
• AMO Tecnis Symfony. In June 2014, AMO received the CE Mark to market the Tecnis Symfony Extended Range of Vision IOL in Europe. The Symfony takes a different approach to maximizing a patient’s range of vision by addressing the optical property known as chromatic aberration.
Because it tackles this chromatic aberration, the Symfony is an example of an emerging class of IOL known as the extended-depth-of-focus lens. Though the nomenclature has yet to solidify, surgeons say the current hallmark of the EDOF lens is that it gives cataract patients a somewhat expanded depth of field without the drawbacks associated with a multifocal visual system.
Jack T. Holladay, MD, MSEE, FACS, a clinical professor of ophthalmology at Houston’s Baylor College of Medicine, says the EDOF lens may fill a niche for certain surgeons and patients. “About 8 percent of the lenses used today are multifocals,” he says. “The reason for this relatively low usage is a result of the typical surgeon not wanting the possibility of a lens exchange if the patient has intolerable halos or glare. This isn’t the end of the world, but it is another surgery, there are costs involved, the patient often goes to another doctor for this, et cetera. So, for this surgeon, it’s easier to put in a non-multifocal lens where the risk is that if the patient doesn’t have adequate near vision you can give him a pair of reading glasses.
|
To understand how the Symfony can give more depth of field, it helps to understand the natural steps of accommodation, surgeons say, because the lens actually builds on them to get its effect. “When we look up close, we experience the depth-of-field effect,” explains Dr. Holladay. “Our pupils constrict. That constriction ends up giving us the equivalent of about 0.75 to 1 D more near vision than we’d have when looking into the distance because of the pinhole effect.”
Building on this natural accommodative effect, the Symfony uses diffractive optics to both improve the quality of vision from the lens and expand the range of distances the lens at which the lens can adequately focus. “The first thing to understand is that the term diffractive optics doesn’t necessarily imply multifocality,” says Daniel Chang, MD, an ophthalmologist from Bakersfield, Calif., who is an investigator for the U.S. trial of the Symfony. “This is not a multifocal lens, but it does use diffractive optics to do two things: First, it corrects chromatic aberration. Second, it uses these optics to extend the range of quality vision.” As Drs. Holladay and Chang explain it, with optics you can’t gain an expanded range of vision without losing something in terms of the sharpness of vision; this is just the nature of the beast. However, by correcting chromatic aberration, even without using diffractive optics to expand the visual range, the lens would have extremely sharp distance vision on the order of 20/12 or even 20/10. The process is not yet done, however, in the Symfony. The diffractive optics are then used to expand the range of vision. Expanding the depth of focus degrades the tack-sharp “starting point” (something must be lost, as Dr. Chang pointed out), but since the lens started with such sharp vision, it only degrades to about the level of 20/20. “So the amount you degrade takes you back to the level of a good monofocal IOL,” Dr. Chang says.
The idea behind chromatic aberration correction is simply to get the colors of the spectrum focused at the same point. “The different colors of the spectrum focus differently,” Dr. Chang explains. “Different materials have different dispersive properties with light; some focus colors closely together and some spread them out. The idea is that if you focus all of the colors together, you can have a higher quality of vision. The Symfony takes the AMO acrylic that focuses colors well—meaning it has a low dispersion—and improves upon it.”
Dr. Chang says he can’t discuss any of the current FDA results, but based on information from New Zealand and Europe, the Symfony gives 20/20 or better vision at distance over a range of about 1.5 D, and 20/40 or better over a range of 2.5 D. “Ninety-six percent of patients had 20/25 or better vision at intermediate,” he says. “At near, 92 percent have 20/40 or better vision. In terms of quality of vision, it’s comparable to a monofocal from a night vision and a contrast sensitivity perspective.” The U.S. FDA trial of the Symfony lens is ongoing.
• Bausch + Lomb Crystalens AO and Trulign Toric. One of the originals from the first wave of presbyopic lenses, the Crystalens doesn’t need much introduction. Though surgeons and patients achieve varying degrees of near vision from the proposed forward movement of the lens due to its flexible, hinged haptics, Crystalens doesn’t pose the risk of visual problems such as halo or contrast sensitivity loss that can crop up with a multifocal lens. The Crystalens AO has prolate, aspheric optics that are free of spherical aberration. There’s also a toric version of the lens, the Trulign.
In a recent study of 78 patients randomized to receive the Crystalens AO, the Alcon ReSTOR +3 D or the Tecnis Multifocal, the Crystalens patients had significantly fewer halos than the Tecnis, and less optical scatter than either the ReSTOR or the Tecnis MF.1 Though binocular uncorrected distance acuity wasn’t significantly different among the lenses, the AO had better monocular and binocular uncorrected and distance-corrected intermediate acuity than the ReSTOR or the Tecnis MF. However, the ReSTOR and the Tecnis MF had better uncorrected and distance-corrected near acuity than the Crystalens.1
Bloomington, Minn., surgeon Y. Ralph Chu has been implanting the Crystalens, in addition to other premium IOLs, for more than 10 years, and says his approach to the lens has evolved over time. “While I believe multifocal IOLs can be effective, it’s hard to predict who’s going to be very unhappy with the loss of quality of vision that they have,” Dr. Chu says. “For that reason, I feel like offering a lens that has a lower risk of these issues, yet still gives some extended range of focus, is something patients understand and appreciate.
“Our discussion with candidates for presbyopic IOLs has changed,” Dr. Chu continues. “We used to give those talks [from the podium] about patient selection, but we’ve evolved into educating all patients about their options. There is no perfect lens platform out there right now, so patients have to understand the limitations of the technology and see how it would fit into their lifestyle. Having that education is more important than saying, ‘You drive a truck so you shouldn’t get this type of lens.’ ”
As to what a patient’s postop near vision will be, Dr. Chu says his view of this has evolved, also. “I see it as an individualized process vs. a specific endpoint,” he says, “because we know there are people who see 20/20 and J1 with a multifocal who are unhappy and we’ve had patients with great intermediate and distance vision, but who still wear readers, who are very happy. I really emphasize it’s a binocular system, and our goal is to use both eyes together. We try to understand at what distance the patient needs to see and achieve that goal for him. We will actually say that there’s a possibility of wearing glasses at some distance for some activities, and this goes for any lens platform.
“I don’t target getting everyone to 20/20 and J1 because it may not be what some want,” he continues. “Some want to see the computer and at distance and are fine with wearing a light reader, while some might like the computer and near vision distances and are fine wearing glasses for distance.” Dr. Chu says he’ll often employ monovision with the Crystalens to boost the near vision. “We’ll work in a little mini-monovision, setting the non-dominant eye for a little more near,” he says. “That’s a great technique to help maximize the range that patients get with the Crystalens. We customize it to the patient; there’s no one set way we treat every Crystalens patient.”
The Crystalens platform also gives surgeons an option for treating a patient’s astigmatism in the form of the Trulign IOL. In the FDA study of the Trulign, it achieved an average reduction in cylinder of 86 percent, with 78 percent of the patients ending up within 0.5 D of the intended refraction. In terms of postop rotation, there was an average rotation of less than 2 degrees between four and six months postop. Ninety-seven percent of eyes rotated 5 degrees or less.2 “The Crystalens design, with its haptics and rectangular shape, fits a toric platform well,” opines Dr. Chu. “It’s been incredibly stable rotationally.”
• Monofocal IOLs with some depth of focus. Over the years, surgeons have noted that some monofocal IOL patients will achieve more depth of focus than one would think possible with a touch of monovision.
|
One monofocal lens that’s gotten some buzz for its near effect is the Lenstec Softec HD, a flexible acrylic IOL with an aspheric optical design on both the front and back surfaces. At the 2011 meeting of the American Society of Cataract and Refractive Surgery, Tampa, Fla., surgeon Jim Gills reported on a study from his practice in which 28 percent of Softec HD patients could read J3 [20/40] or better uncorrected monocularly.
Los Angeles surgeon Paul Dougherty says he’s experienced similar results. “The lens is composed of the same material as the Tetraflex [accommodating IOL],” says Dr. Dougherty, who thinks this may contribute somewhat to the lens’s apparent ability to give a better range of vision in some patients. “Though these patients don’t get full accommodation, I don’t need to do as much monovision on them as I would with a pure conventional monofocal lens to get them out of reading glasses. If we set them for distance, they’ll get distance and maybe some intermediate vision, but they’ll still need reading glasses.”
Lenses in the Pipeline
In addition to the handful of non-multifocal lenses that can expand patients’ range of vision, there are also other innovative designs in the works.
• Calhoun Vision Light-adjustable Lens. The LAL’s design is unique in that its power is adjustable by the surgeon, with input from the patient, after the lens is in place. The adjustment is made by irradiating the lens’s special silicone material with ultraviolet light, which changes the lens’s shape and therefore its power. The same light is then used to lock in the shape change when the refraction is optimal. The LAL is currently in a U.S. FDA trial.
An interesting application of the adjustability of the LAL is using it to induce special aspheric changes to the lens, broadening a patient’s range of vision. Calhoun calls this process adjustable blended vision.
Tijuana surgeon Arturo Chayet, who consults for Calhoun Vision and has used ABV in patients, explains how the process works. “The idea is to bring the patient to emmetropia and then add asphericity to the optical component of the lens,” he says. “The protocol typically calls for the dominant eye to be adjusted for low asphericity, and the non-dominant eye for high asphericity, with the goal being all three ranges of vision. Typically the dominant eye will be set for distance and the non-dominant for near, and both together will give good intermediate vision. In the non-dominant eye, they give up a little distance vision for more near vision, so it’s typically around 20/32 uncorrected in that eye for distance, but it will be able to read J2 or J3.”
In a study of binocular vision results in 20 ABV patients at Dr. Chayet’s practice, 75 percent could see 20/16 or better at distance after lock-in. Eighty-five percent now see 20/20 or better and 100 percent see 20/32 or better. In terms of binocular intermediate vision at 60 cm, 60 percent see J1+ versus zero patients preop, 75 percent see J1 versus 20 percent at this level preop and 100 percent see J2 or better compared to 45 percent preop. Ninety percent see J2 or better binocularly at near (40 cm) versus 15 percent preop. Fifty-five percent now see at least J1, compared to 5 percent who could see that well preop.
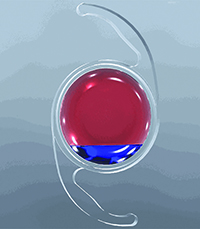
• PowerVision FluidVision lens. The FluidVision lens is an acrylic IOL with anterior and posterior optics with a central cavity between them. The compressible haptics contain a silicone-oil-based fluid. Paul Roux, MD, of Pretoria, South Africa, is the lead investigator on the FluidVision’s latest international study, and says the haptics work together with the eye’s natural processes to aid accommodation. “The two large haptics are connected to the central fluid cavity,” Dr. Roux explains. “When the eye’s normal physiological accommodation occurs and the zonules release tension on the capsule, it compresses the two large haptics. This pushes the silicone fluid between the two optics and creates an accommodative effect.”
In a pilot study of the lens, 20 patients underwent monocular implantation with it. At six months, uncorrected distance vision averaged slightly better than 20/20, intermediate averaged 20/25 and near averaged 20/33. “The average objective accommodation measured is just under 2 D,” says Dr. Roux. “The subjective accommodation is actually more, around 2.5 D, because of pupil size reduction during accommodation. This effect appears to be lasting.
At this stage, the one thing about the lens that’s slightly unpredictable is the initial refraction after you’ve put it in,” Dr. Roux adds. “Initially, we’d have a patient who was -2 or +1 postop. It’s taken some changes to get the initial refraction as close to plano as possible. Now the majority of patients are within 1 D of emmetropia.”
Right now, the lens injector goes through a 4-mm incision. “It’s a large lens because it’s got to fill the bag,” explains Dr. Roux. “That’s the basis on which it works. However, there’s a drive to make that smaller, to around 3.5 mm or even less.”
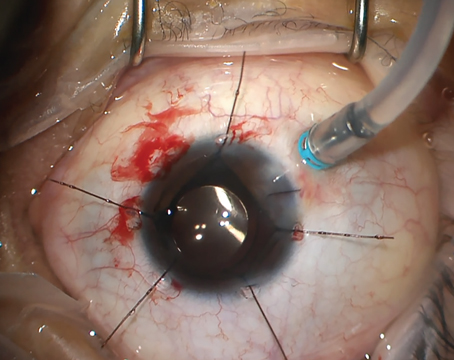
• Akkolens Lumina. Similar to the way the FluidVision lens uses physiological processes in its operation, the Lumina is a dual-optic lens that relies on the action of the ciliary body for its effect.
Alicante, Spain, ophthalmologist and Lumina researcher Jorge Alio says one of the keys to the lens’s mechanism is its placement in the sulcus, which allows it to move. “The sulcus is stable and isn’t influenced by fibrosis,” he says. “We have a paper that’s been accepted for publication in the Journal of Refractive Surgery in which we implanted the lens in the sulcus of one group of non-human primates and in the capsular bag in another group. After six months, the lens in the capsular bag is totally blocked but the lenses in the sulcus are still working.
“Once in the sulcus, action of the ciliary body causes one of the optics to slide over the other optic, creating a continuous change in the total lens power,” Dr. Alio continues. “Currently, the limits of accommodation in the pilot study have been between 1.5 and 6 D, and the effect has remained at one year. Obviously, a lot still has to be demonstrated to use the lens clinically on a standard basis. I think it will accommodate 2 to 3 D easily, probably more in some cases.”
Dr. Alio says the study has included 75 cases, 55 with the Lumina and 20 monofocal lens controls. Though the exact results are currently confidential, he says the distance vision is similar to that of a monofocal IOL and that intermediate is very good, owing to the fact that 2 to 3 D of power is helpful with intermediate distances. “Near vision is good,” he says. “Even though some patients find 1.75 D to be a little less than necessary to keep near vision sustained, we have many who can see at near without glasses.
|
• Vision Solutions Technologies’ Liquilens. Also taking the liquid route to accommodation is a lens invented by Rockville, Md., optometrist Alan Glazier. However, instead of relying on the body’s anatomical forces, the lens uses gravity.
“Liquilens is kind of like putting on a reader,” Dr. Glazier explains. “It uses the fluidics of two immiscible optically clear biocompatible fluids and their interplay to introduce an additional index of refraction into the line of sight that provides additional power when the patient looks down at a 60 to 70 degree angle.” When the patient looks forward the fluid is out of the way and the lens provides distance vision. “One thing that some lens designers miss is that the act of reading isn’t only an act of having near vision but sustaining it over time,” Dr. Glazier says. “You have to have accommodation to see a certain distance but you need a certain amount in reserve, as well. So, to shoot for 2.5 D of focus, you might get that and the patient would be able to glance and see something, but the act of reading requires him to sustain that. To do that, you need extra power.” Dr. Glazier says the lens has been able to achieve 9 D of accommodation in lab bench testing.
Intermediate vision won’t be strong at the outset, though. “In the lens we’re planning on entering the market with, it’s like a bifocal so it won’t have much intermediate vision,” Dr. Glazier says. “But we have patents on designs that will provide intermediate in second- and third-generation products.” Dr. Glazier is seeking CE certification for the lens in Europe.
In the future, Dr. Chang says some of the innovations occurring today will work their way into common ophthalmic parlance. “Chromatic aberration is an issue that most surgeons don’t commonly think about, but correcting it can make a difference,” he says. “It’s kind of like 15 years ago when researchers began talking about spherical aberration and physicians were mystified. However, when we started correcting for it, it made a difference and people appreciated it. Chromatic aberration is basically the other half of that story.” REVIEW
Drs. Holladay and Chang are consultants for AMO, Dr. Dougherty owns stock in Lenstec, Dr. Chayet consults for Calhoun Vision and Dr. Chu is a consultant to Bausch + Lomb. Dr. Alio and Dr. Roux are consultants to Akkolens and PowerVision, respectively. Dr. Glazier owns the rights to the Liquilens.
1. Pepose JS, Qazi MA, Chu R, Stahl J. A prospective randomized clinical evaluation of 3 presbyopia-correcting intraocular lenses after cataract extraction. Am J Ophthalmol 2014;158:3:436-46.
2. http://tinyurl.com/qfp7omf. The FDA Medical Devices Advisory Committee on the Trulign IOL. Accessed 11 Dec 2014.
3. Boerner CF, Thrasher BH. Results of monovision correction in bilateral pseudophakes. J Am Intraoc Implant Soc 1984;10:1:49-50.