Usually, when an ophthalmologist encounters these conditions, the signs and symptoms are sufficiently different to make identification straightforward. However, that’s not always the case. Here, three experienced ophthalmologists share their advice for identifying and managing these problems when the nature of what you’re dealing with isn’t obvious.
Ask the Right Questions
“It’s not often a clinician encounters a patient that’s truly tough to diagnose,” says Stephen C. Pflugfelder, MD, a professor and director of the Ocular Surface Center at Baylor College of Medicine’s Cullen Eye Institute in Houston. “When faced with a patient who has dry eye, allergy or infection, most of the time the clinical features speak for themselves. But there can be occasional cases where it’s hard to distinguish.”
“Determining the nature of the problem starts with a good history and physical,” says Bruce Koffler, MD, director of the Koffler Vision Group in Lexington, Ky., and associate clinical professor of ophthalmology at the University of Kentucky Medical Center. “It’s important to ask the right questions. What is the chief ocular complaint? How long has this been going on? What are the signs and symptoms? Is anyone else in the family having similar problems? Does the patient have any systemic medical problems or indications that might play a role—for example, an immune disorder such as rheumatoid arthritis, lupus or vascular disease? Does the patient have a severe allergic condition, or any dermatologic problems relating to that such as psoriasis? The latter would suggest that the patient might have an unusual tendency towards allergy.
| ||||||||||
Dr. Koffler notes that failing to ask the right questions is often simply the result of being pressed for time. “In our busy days, with new factors such as electronic records to manage, digging deep looking for clues can get bumped down the priority list, especially for a non-specialist. We’re busy running from room to room, and sometimes these probing questions take extra time to ask. Of course, if you’re a cornea and external disease specialist, you’re more likely to see cases that have not been diagnosed. In that situation you have to take the time to consider every possible factor that might be contributing to the problem.”
Steven E. Wilson, MD, professor of ophthalmology and director of corneal research at the Cole Eye Institute of the Cleveland Clinic, agrees that in most cases, telling infection from allergy or dry eye isn’t hard to do. “Usually a careful history and exam will enable a trained ophthalmologist to determine which condition is present,” he says. “Most of the time they appear separately and present differently. However, sometimes it’s hard to be sure whether you’re seeing dry eye or allergy, or both, because one can exacerbate the other and there can be some overlap in the symptoms. It’s even possible for a patient to have dry eye, allergy and an infection all at the same time; a patient could have blepharitis with chronic dry eye and get allergic symptoms once a year, too.”
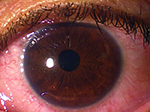
Allergy vs. Dry Eye
| ||||||||||
“If the patient has a red eye, boggy conjunctiva, watery discharge and itching, that’s certainly allergic conjunctivitis,” says Dr. Wilson. “On the other hand, if the symptoms are more subtle, where the eye isn’t very red but appears irritated, that’s the kind of patient that might make you wonder whether the problem is allergy or dry eye. Again, a detailed history is crucial. What symptoms does the patient have? Is itching a part of the symptom complex? That will make you lean more toward allergy. Is there a seasonal nature to it? Do the eyes get a very red conjunctiva periodically? Usually dry eye is not as much associated with that. Seasonal allergies tend to be more obvious to the clinician, based on the history and exam, especially when it’s the right time of year for this patient and itching is the dominant symptom. That’s not likely to be a dry-eye problem.”
Dr. Wilson notes that while there is underlying inflammation in dry eye, it’s a pathological diagnosis. “You don’t necessarily see redness when looking at the whites of the patient’s eyes, but you see it when you do a conjunctival biopsy or lacrimal gland biopsy,” he points out. “In contrast, allergy patients often do have injection as a part of their signs. Itching and injection of the conjunctiva may not be constant, but they do recur. Another key question is whether the patient has other allergies, such as allergies to grass or certain foods, or has other conditions associated with allergy such as dermatitis or asthma. You can elicit that in the history.”
Dr. Wilson adds that sometimes a patient doesn’t believe he’s having an allergic reaction simply because it’s new to him. “I often see a patient who is 30 years old and having terrible itching, watering of the eyes and redness who tells me he’s never had this before,” he says. “My response is, ‘Well, at some point everybody has it for the first time. This just happens to be your time.’ ”
Beyond the Exam and History
If the signs and symptoms are subtle, and you remain unsure whether the patient has dry eye or allergy (or both) after taking the history and conducting your exam, two more options remain: you can run tests, and/or you can see whether or not the patient responds to a given treatment.
| ||||||
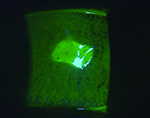
Dr. Wilson agrees. “If you’re still unsure, you can do lissamine green staining and examine the ocular surface and under the eyelids,” he says. “Other tests such as Schirmer’s might be helpful, although dry eye doesn’t always have low tear production.
“If you examine the patient and you still can’t decide whether you’re dealing with allergy or dry eye, a common way to proceed is to decide on an initial therapy and see if the patient benefits from it or not,” he continues. “Often the least expensive option is to prescribe one of the topical antihistamine medications and see if that relieves the symptoms. If the symptoms are very severe and I believe the problem is most likely allergy, I’ll give the patient both a corticosteroid and an antihistamine. If the patient responds dramatically to that, I’m fairly certain the primary problem is allergy.”
Dr. Pflugfelder says that if he really isn’t sure, he might take a conservative approach and have the patient just lubricate the problematic eye. “There’d be no harm in also using topical antihistamine drops, or a combination antihistamine and mast cell stabilizer like Pataday or Elestat,” he says. “Neither of those would cause any harm. However, I’d be reluctant to start corticosteroids if I really wasn’t sure what the problem was.”
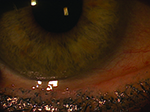
Uncovering Infection
Making sure that any infection is diagnosed is key, both because of the potential for damage to the eye and the possibility of the infection being contagious. A common infectious finding is viral conjunctivitis.
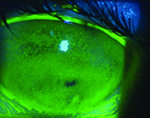
“A classic situation in which you might have a little bit of uncertainty as to whether you’re dealing with infection would be an early viral conjunctivitis,” says Dr. Wilson. “The patient is just starting to get symptoms and has a little bit of injection. In most cases you probably wouldn’t be thinking that the problem is dry eye, given that presentation, but you might be debating whether the patient has allergy or early viral conjunctivitis.”
| ||||||||||
“If I suspect it might be a viral infection, I may use AdenoPlus, which is a rapid, in-office diagnostic test that confirms the presence of adenoviral antigens in the tears or on the conjunctiva,” he continues. “If that’s positive, that would solidify the diagnosis of viral conjunctivitis. The only other viral conjunctivitis would be herpes, which is rare, and might also produce corneal involvement such as dendrites in the epithelium.”
“Usually, viral conjunctivitis will run its course in seven to 10 days,” says Dr. Wilson. “In the winter and early spring here in Ohio we see hundreds of viral conjunctivitis patients. I tell them that I expect it to run its course in seven to 10 days, and only rarely will a patient come back. Actually, timing can also be an important part of telling viral infection and allergy apart. If the patient has established that this is a persistent problem, and it involves a lot of itching, the odds are very good that this is an allergy problem rather than a chronic infection. And, if you’ve treated what was really viral conjunctivitis with antihistamines and discover that this doesn’t improve the patient’s problem, the viral conjunctivitis will likely run its course in a few days. If it doesn’t, and the patient is still having symptoms at that point, I’d do more testing and possibly initiate a different course of treatment.”
He notes that the history may give you a strong indication that the problem is viral conjunctivitis. “The patient may report being exposed to someone who has pink-eye at work, school or home,” he says. “During an epidemic of viral conjunctivitis 30 to 50 percent of people are aware that they were exposed to someone with pink eye. That makes identifying the problem easy.”
“If the patient has herpes, there are good antivirals you can prescribe, but for adenovirus there’s no specific treatment,” adds Dr. Pflugfelder. “About all you can do is inform the patient that he or she has it and warn the patient to be careful to not contaminate the other eye if it’s not yet involved, as well as to avoid contaminating other people. It’s usually advisable for the patient to stay home from work or school. Sometimes these patients have already infected other people, but at least you can prevent further exposure by having them stay home for a while.”
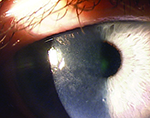
Viral vs. Bacterial
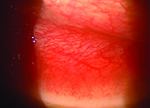
Although less common, bacterial conjunctivitis is always a concern. “When it comes to confusing dry eye or allergy with infection, it depends on what type of infection you’re talking about,” says Dr. Wilson. “Keratitis usually isn’t confused with allergy, but there are some situations in which patients with allergic conjunctivitis can have sufficient corneal involvement that they get infiltrates. Then you could find yourself wondering whether the patient simply has an allergy or if he’s developed a secondary bacterial infection. If the uncertainty cannot be resolved, the clinician may find it necessary to perform cultures and treat for infection, and then monitor the response to the treatment.”
| ||||||
Dr. Pflugfelder says he’d only consider using antibiotics if he found a purulent discharge. “Severe dry eye can sometimes be accompanied by discharge,” he notes. “In fact, these patients are probably a little bit predisposed to develop bacterial conjunctivitis. So if the problem was dry eye and the eye had a lot of pus, I would treat with topical antibiotics, just as I would if the problem was bacterial conjunctivitis. Otherwise, I’d avoid antibiotics; they might not cause any harm, but they’re expensive and you could enhance resistance.”
“If you have a patient who is a diagnostic dilemma and you need to rule out some form of infection, getting a good culture can be very helpful,” says Dr. Koffler. “If a patient has been suffering for a long time, I don’t hesitate to do this. In fact, the chronicity of the disease is an important consideration when deciding whether a culture is appropriate. If the patient comes in with a 24-hour or 48-hour history, we don’t usually get a culture. But if the patient has been suffering for three months, then we’re looking for something different. Most patients in this situation have seen a lot of different doctors, and no one has come up with the answer. So I would definitely consider getting a culture in that situation.”
Dr. Wilson notes that some forms of bacterial conjunctivitis can be persistent and chronic. “Chlamydia conjunctivitis can persist until it’s treated, and it often does,” he says. “We sometimes encounter patients who have been seen by two or three other doctors and treated for dry eye or allergic conjunctivitis—despite the fact that the signs and symptoms of chlamydia are somewhat different from those of allergic conjunctivitis. The presence of a persistent follicular conjunctivitis should always raise the possibility of chlamydia in the doctor’s mind. Cultures and immunofluorescent testing for chlamydia can be performed. If these are not available, clinicians often treat the patient presumptively for chlamydia—for example, with doxycycline 100 mg b.i.d. for four to six weeks.
“If a patient has already been treated before coming to us, we have the advantage of knowing that the previous treatments were ineffective,” he adds. “If the patient is a sexually active adult, we always consider chlamydia as a possible cause. We may even consider this possibility when the patient is a child if there’s any indication of abuse. We can culture for chlamydia to get confirmation; however, the results are not always positive even when chlamydia is present. So if we’re suspicious this is the problem, we may go ahead and treat the patient with a course of doxycycline.”
The Newer In-office Tests
In recent years a number of new in-office tests for factors associated with dry eye and other conditions have become available, but doctors have mixed feelings about how helpful they might be in this situation.
Like Dr. Pflugfelder, Dr. Koffler says he sometimes uses the AdenoPlus test, among others, to confirm a diagnosis. “Viruses are difficult to culture, but we now have immunoassays such as the AdenoPlus that can help confirm the presence of adenovirus,” he says. “There are also herpetic assays that can also be helpful in difficult cases. I find it useful to have these handy in the office. If everything points me towards an adenovirus infection, and I get a positive AdenoPlus diagnostic test, I’m feeling pretty good that that might be my diagnosis. This is important, since patients with active adenovirus are encouraged to not go to work and to take infection-control measures at home.”
|
“The same thing could be true of testing for matrix metalloproteinase 9,” he adds. “If the level is high, I think it would supplement the clinical diagnosis. On the other hand, there might be enough of an increase in MMP-9 in allergy or viral conjunctivitis to make the test positive as well. I don’t think this question has been resolved, so the specificity of these tests remains to be determined.”
Dr. Wilson agrees. “The biggest problem with a test like the MMP-9 test is that it’s non-specific,” he says. “It can give a positive result in dry eye, in infection or in any inflammatory condition affecting the eye. Basically, all it tells me is that there’s inflammation, which I often already know from my examination. Osmolarity testing is also problematic in this situation. People are using osmolarity to try to be more specific when diagnosing dry eye; the problem is, there’s so much variability in the test. Even if you take a group of completely normal patients with no signs or symptoms of dry eye, the test could be positive. So in my mind, the jury’s still out on these adjuvant tests. I think this kind of test can be useful, but I don’t think it’s a panacea for making a diagnosis that eliminates the need for a good history and examination.
“I think it would be really wonderful if we had much more specific molecular markers that could be tested,” he adds. “That might allow us to say, ‘This is definitely dry eye,’ or ‘This is definitely allergy.’ I think the potential for this exists because the molecular pathways are different, but at this point we don’t have tests that can do that.”
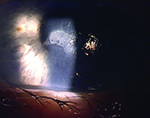
Using Steroids
Corticosteroids can be helpful in many situations, but there are a host of caveats. “With a bacterial infection, I like to have 24 to 48 hours of antibiotic drops on the eye before I think about steroids,” says Dr. Koffler. “Even when I believe the problem might be a Staphylococcus hypersensitivity reaction, I’ll still often use plain antibiotics and add a steroid 48 hours later, after I feel that I have a better handle on the situation. Within 24 hours I’ll be getting back information from the cultures, and that will give me a better idea as to whether antibiotics are the right approach. The main point is, don’t rush with steroids. You can add them later. If you don’t really know what the problem is, stick with an antibiotic first.”
“Corticosteroids work well in dry eye or if the problem is allergy and the patient is pretty symptomatic,” says Dr. Pflugfelder. “Corticosteroids also can do a good job of suppressing inflammation caused by viral conjunctivitis, but there’s a debate about how advisable that is. Some people feel that you might prolong the viral infection by using steroids. So steroids generally improve dry eye and allergy, and improvement will be seen in viral conjunctivitis, but they are generally reserved for severe membranes or subepithelial infiltrates. On the other hand, treating bacterial conjunctivitis with steroids would not be advisable. Fortunately, bacterial conjunctivitis is pretty rare. It’s usually only seen in sick or elderly people, and sometimes in children who have pharyngitis or otitis media.”
Dr. Wilson notes that if you’re not certain whether the patient has allergy or early viral conjunctivitis, caution is warranted. “If this patient actually has early viral conjunctivitis and you mistake it for allergy and treat with a corticosteroid, you might make the patient worse by inhibiting the patient’s immune response,” he says. “The outcome might not be too bad if the problem is actually adenoviral conjunctivitis; but if the problem is primary herpes simplex, and you give the patient corticosteroids thinking it’s allergy, you could potentially have a very serious problem on your hands. For this reason, you have to be as sure as possible about the diagnosis before you give the patient corticosteroids.” Dr. Wilson adds that you also have to be careful about steroid side effects, such as the possibility of a spike in intraocular pressure.
“The other problem that sometimes arises is that the relief may be so thorough and quick that the patient wants to know why he can’t use the steroid drops all the time,” he adds. “You have to be careful to explain to the patient right up front: ‘This is something you can maybe use a couple of times a year, for a period of time, but you can’t use this chronically because it can cause cataracts, glaucoma, increased risk of infection and so forth.’ ”
Managing Multiple Problems
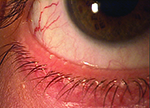
“Sometimes one condition can lead to another,” notes Dr. Koffler. “For example, allergy might end up plugging the meibomian glands, which then have Staphylococcus captured in them, potentially causing sties and chronic infectious blepharitis and conjunctivitis. Contact lens wear with chronic touching of the eye, along with the use of different disinfection agents, can go on to cause blepharitis, both infectious and noninfectious. And dry eye is associated with meibomianitis 50 percent of the time. So, one problem can definitely lead to another.
“I think you should always go after the infection first, unless you’re very sure that it’s something different,” he continues. “If you don’t immediately treat allergy or dry eye, you’re not going to hurt anything. But if you let an infection go on, you may get further scarring; it may even go on to ulceration. So if you’re faced with multiple problems, work on the infection; maybe start some lid hygiene to quiet down the lids. Later on, after you feel things are under control, you might want to come in with a steroid or a specific antibiotic that’s better at handling the inflammatory component of meibomianitis. The use of nighttime ointments can also be helpful for allowing the patient to get a good dose of antibiotic at nighttime.”
Dr. Wilson points out that allergic conjunctivitis can sometimes lead to dry eye. “Patients with year-round allergies tend to be more problematic, especially if they’re severe,” he notes. “They may have ongoing atopic changes in the conjunctiva with a lot of irritation and itching, although sometimes that component isn’t as prominent. You look at these patients and your exam tells you they most likely have allergic conjunctivitis—but a patient in this situation can also develop dry eye. So sometimes you have to treat both.”
Dr. Pflugfelder says that in the rare instance where he encounters someone with all three problems, he focuses on the most symptomatic concern. “If I was sure that the patient had acute viral conjunctivitis, I probably wouldn’t use corticosteroids,” he says. “I’d just treat with lubricants, and treat the itching with an antihistamine drop. Once the viral conjunctivitis resolved, I might use other things such as corticosteroids or Restasis.”
Going Down the Right Path
These pearls can help ensure that your diagnosis is correct and treatment goes according to plan:
• When taking the history, ask about workplace and home environments. “Nowadays, many of us sit at a desk for long periods of time,” notes Dr. Koffler. “Ask whether the patient is aware of air blowing on him during working hours. This could cause dry eye, or an allergic reaction if the vent is spreading some kind of allergen. The air at home could be a problem as well. Are there dust mites or other allergens in the house? Does the patient need a humidifier? The reality is, if you’re not sure about the nature of the problem, you really have to search deeply.”
• Don’t forget to ask about eye drops and systemic medications the patient may be using. “These may explain dryness or irritation and help you avoid making an incorrect diagnosis,” says Dr. Koffler. “Topical eye drops of different kinds can cause toxicity and irritation that presents in any one of a number of ways, from chronic dry-eye symptoms to meibomian gland disease to chronic red eyes. Often I’ll just stop the chronic glaucoma drop a patient has been using, and her red eyes start to get better.”
• Remember that a reaction to an eye drop may not happen for the first few months of use. “Eye drops can cause delayed sensitivity, which means that initially the patient may appear to be doing fine,” notes Dr. Koffler. “Then after six months or a year all of a sudden the patient starts to have an allergic reaction to the drop or to the preservative in the drop. The fact that the reaction just appeared doesn’t mean you should eliminate the eye drops as a possible cause.”
• Warn your staff to be careful around red-eye patients. “This is something many clinicians are not careful enough about,” says Dr. Koffler. “Until you’re sure what you’re dealing with, avoid physical contact with this kind of patient. If the red eye is caused by an infection, it can easily be transmitted. I’ve seen a couple of ophthalmologists get nasty adenovirus infections—most likely from their patients—that put them out of work for a significant amount of time.
“I make every attempt to not touch the infected patient physically,” he continues. “I like to shake hands with most patients, but I don’t shake hands with red-eye patients. I also never touch the patient’s eyelids with my hands; I always use cotton applicator sticks to hold the lids when doing the examination. Of course, you also have to instruct your staff to do the same, because they’ll see the patient first. I tell my staff that when a patient has red eyes, don’t be in a hurry to take pressures. A glaucoma attack could present as a red eye, but until I see the patient and get the feeling that glaucoma is the problem, I don’t want them to touch the patient or use my instruments on the patient. Also, I have to assume that by the time I get into the room, the patient has touched several tables or my slit lamp. So when we’re finished in a room that I think is infected, I quarantine the room. My team comes in with gloves and alcohol and completely wipes down all the surfaces—and they don’t spare the alcohol.
“Of course, if I think the problem is not infectious—viral or bacterial—then I’m not going to worry about this,” he adds. “But sometimes you’re not sure. That’s why you really should back away from contact with a red-eye patient until you know what the problem is. We don’t think about this enough, and we can suffer the consequences.”
• Check for swelling in the preauricular lymph node. “A swollen lymph node in front of the ear is a classic sign of viral conjunctivitis,” Dr. Pflugfelder points out. “Chlamydia can also cause that. So, that’s one of the first things I check when I see someone with pink eye. If that node is swollen and other signs are present, it’s almost diagnostic.”
• Ask whether the patient is self-treating. “You have to be careful that the patient isn’t mixing up something of his own and putting it on or in the eye,” notes Dr. Koffler. “People may hear or read on the Internet about a do-it-yourself remedy using herbal medications, or putting a tea compress on the eye, thinking it will treat pink eye. It’s important to know what they’ve been doing on their own.”
• If allergy might be the explanation, consider getting smears when culturing for eosinophils. “If you take a culture, you can set aside some of the specimen on a slide and ask pathology to look at the cells,” notes Dr. Koffler. “Increased eosinophil cells are a typical sign of allergy. You could also have an eosinophil blood count done, to see if the number is elevated, which would indicate a significant allergic reaction.”
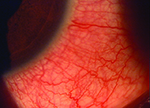
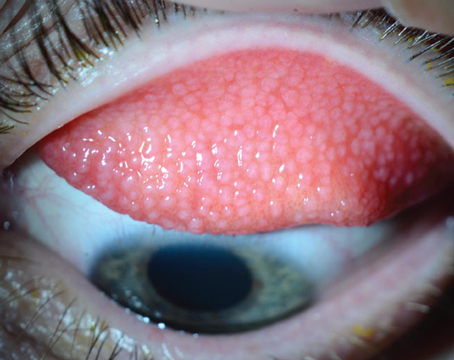
• In case of infection, look carefully at both the conjunctiva and cornea. “Bacterial infection usually causes a papillary conjunctivitis, and the corneal lesions tend to be round, whitish infiltrates,” notes Dr. Koffler. “Viruses like herpes simplex or adenovirus tend to cause more of a follicle reaction on the conjunctiva. On the cornea, adenovirus tends to produce classical stellate lesions, while herpetic disease tends to produce dendritic lesions. These signs can be very helpful to us in differentiating whether the infection is bacterial or viral.”
• Consider topical cyclosporine A when treating both allergic conjunctivitis and dry eye. “If a problematic seasonal or year-round allergy patient is not controlled by antihistamine products or is in danger of steroid overuse, sometimes topical cyclosporine A will be very beneficial and keep the condition under control,” says Dr. Wilson. “And if the patient also has dry eye, you’re treating that, too. Cyclosporine A treats inflammation, which is a component in the pathophysiology of most dry eye, and there’s an inflammatory component to allergic conjunctivitis as well. The inflammation in dry eye vs. allergy is mediated by different cell types, but cyclosporine A seems to address both types well.”
“There’s no harm in using Restasis in the presence of allergy,” agrees Dr. Pflugfelder. “In fact, Restasis would probably help with severe allergic conditions, such as vernal conjunctivitis or atopic keratoconjunctivitis. I don’t know that anyone has proven that it’s good for seasonal allergic conjunctivitis, but again, it wouldn’t hurt.”
• Remember that you don’t always need to treat. Dr. Pflugfelder notes that viral conjunctivitis is self-limiting. “Viral conjunctivitis will get better on its own, in most cases,” he says. “There’s really no specific treatment for viral conjunctivitis anyway. All we have are palliative treatments like using artificial tears and cold compresses. If the viral conjunctivitis produces corneal problems such as subepithelial infiltrates, then steroids or Restasis will help. In any case, there’s really nothing you can do to prevent that from occurring; whether or not corneal problems occur depends on the particular virus you’re dealing with, and they would occur subacutely after 10 days or two weeks.
“For viral pink eye, there’s no harm in deferring treatment and reassessing in a week or so,” he continues. “In fact, even mild, non-severe bacterial conjunctivitis is usually self-limited, even without antibacterial treatment, so there’d probably be no harm in waiting a week or two and then reassessing the patient in mild bacterial cases. In either situation, once the conjunctivitis has resolved you can deal with any remaining condition such as dry eye.”
• Know when it’s time to let someone else investigate. “Don’t keep trying endlessly to treat a nonresponsive problem,” says Dr. Koffler. “If you need a cornea-external disease specialist for a given patient, go ahead and send the patient on to that individual. If the problem is systemic, consider getting help from an allergist. The latter is something we don’t often think of, but in some cases it could be useful. A specialist in that area can delve into things even further and get allergy testing done.”
The Diligent Detective
Ultimately, getting to the bottom of a mystery largely depends of the thoroughness of your exam and history, and being willing to stay on the case. “Doctors should get in the habit of doing a careful slit-lamp examination, checking for a preauricular lymph node, using diagnostic dyes and supplementing with tests for adenoviral antigens, MMP-9 or high osmolarity, if appropriate based on the clinical findings,” says Dr. Pflugfelder. “And of course, take a good history. If the patient mentions that two people in the office had pink eye last week, that pretty much tells you what you’re dealing with.”
“Look at the situation systematically,” advises Dr. Koffler. “Get a good history and physical. Examine the conjunctiva—are there papules or follicles? If appropriate, get a culture or smear. Have some diagnostic tests available, such as rapid immune tests for herpes simplex or adenovirus. And be very careful to safeguard yourself, your staff and other patients from individuals who may have contagious conditions.”
Dr. Wilson admits that it’s always possible to be fooled. “All of us who practice medicine are faced from time to time with a situation where we think we’re dealing with one thing, and then it becomes clear that we’re actually dealing with something else,” he says. “For example, herpes can be like that. It’s known as the great masquerader, because you think you’re dealing with one thing and then the patient gets worse because you didn’t treat him with an antiviral. The patient may go on to develop corneal epithelial lesions with or without infiltrates that are characteristic of herpes simplex, and you realize that you were fooled.
“Medicine really is a mix of art and science,” he adds. “Sometimes a patient is a bit of a mystery case, where you have to explore and do multiple tests and try more than one treatment until you discover what the problem really is. The best approach is to take a thorough history and do a careful examination, looking at all the signs and symptoms. If necessary, you can run appropriate tests. However, be careful not to rely too much on tests. It’s the history and exam that usually will lead you to the correct diagnosis.” REVIEW
Dr. Wilson is a consultant for Allergan. Drs. Koffler and Pflugfelder have no financial ties to any product mentioned.