As every ophthalmologist knows, femtosecond laser cataract surgery is being heavily promoted as the “next big thing.” But the lack of data showing significant improvement in outcomes, and the half-million-dollar price tag—in a down economy—have caused most surgeons to balk. At the same time, many have complained privately that the rosy picture of this technology being painted in the media and on podiums may be unrealistic.
In this article, concerned parties offer a look at some of the potential downsides practices face if they invest in this technology, and question some of the assumptions the pro-femtosecond laser camp has put forward.
Investing in a Down Economy?
“At the advent of any new technology, to one degree or another there’s an immediate chorus of naysayers and doubting Thomases, and a countervailing chorus of, ‘This is the real deal, the next big thing,’ ” says John Pinto, president of ophthalmic practice management consulting firm J. Pinto & Assoc. “A tug of war ensues between those two cohorts, and one side or the other always wins.
|
Mr. Pinto says that in the present environment, as both an ophthalmic economist and a lay person who follows this industry closely, he has a hard time understanding how femtosecond laser cataract surgery is going to become the standard of care five years down the line. “The smartest ophthalmologists I know are telling me that they don’t think there’s going to be a material patient benefit from this, or if there is, the benefit will be negligible,” he says. “Meanwhile, the economics of this are overwhelming.”
Specific economy-related questions surgeons are asking include:
• How can we be sure we’ll recoup the investment? Some LASIK surgeons who chose to purchase a femtosecond laser for LASIK have had a tough time recouping their investment because of the economy. “Years ago many LASIK surgeons were convinced that if they didn’t purchase a femtosecond laser to do LASIK they’d be out of business,” notes Stephen Pascucci, MD, FACS, founder of Eye Consultants of Bonita Springs, in Florida. “In fact, many who never jumped on board are still in business, and quite possibly enjoying better surgical volume and margins because they had better price flexibility when the economy tanked.”
“I think we still don’t know from either an economic or clinical perspective whether this is the next big thing or a bridge too far,” says Mr. Pinto. “The situation might have been very different if this was 15 or 20 years ago and the economics of ophthalmology were a bit more robust. Back then, even if there was a sense that the new option was only slightly better for the patient and economically neutral or even negative, surgeons might have said, ‘Maybe it’s something we should get into.’ Today, ophthalmologists are not only being pressured by the macroeconomy in the United States—which is finally starting to show a little bit of freshness—but by the inevitable scissoring that’s going to occur on the Medicare side of things. Ten or 15 years ago, there was a sense that investing half a million dollars was rolling the dice on one year’s salary. Today, it might mean rolling the dice on 18 months’ salary. The risk-to-reward ratio is not very favorable.”
• Will we be able to bill insurance for this? “Presently, it seems that the legal justification to allow doctors to charge patients for use of this technology is astigmatism correction,” notes Dr. Pascucci. “We already have monofocal toric IOLs. What happens after we get multifocal toric IOLs? What’s the justification then? At the end of the day I think the best thing would be for the Centers for Medicaid & Medicare Services to allow balanced-billing of patients for use of the femtosecond laser system as a doctor sees fit, and let market forces control the costs.”
• Will the cost restrict patient access? “The way this technology is being sold and marketed, it’s only going to be useable for the patients who can financially afford it,” says T. Hunter Newsom, MD, founder of Newsom Eye Center in Tampa Bay, Fla. “That puts us doctors in a tough spot because there are definitely patients who cannot afford this technology but would benefit tremendously from it. And it’s not realistic to expect the surgeon to pay the $1,000 to use it. Considerations like this have made it tough for us doctors in the audience to swallow what we hear from paid consultants on the podium.”
Dr. Newsom says he doesn’t mean to bash the technology. “I just think it’s unfortunate the way this is being marketed and sold,” he says. “It should be sold as a $100,000 to $200,000 laser with no click fees, allowing us to have unrestricted access to this technology. Then we could use it on any patient that could benefit from it.”
Is the Technology Really Better?
Although there is reason to think that femtosecond laser cataract surgery may improve outcomes—at least a little bit—peer-reviewed, published evidence is still lacking. “I’m all for better outcomes because of better technology,” says Dr. Pascucci. “But so far I haven’t seen one scientific, peer-reviewed article that demonstrates clear, statistically significant better visual outcomes, such as better uncorrected visual acuity, with the use of the femtosecond laser for cataract surgery.”
Mr. Pinto agrees that claims of superiority wouldn’t have much basis today. “I spoke to several thought leaders at a recent meeting,” he notes. “Basically, they said flat out, ‘There is no published, refereed document in the world that reports that this favorably changes the outcome of cataract surgery. The patient will not be functionally seeing better as a result of using this tool.’ Without that evidence, companies are asking surgeons to spend a half million dollars to replace a $1.60 capsulorhexis needle.”
Even if femtosecond cataract surgery does improve outcomes, will the improvement be worth the cost, and will the people who need improvement the most be able to afford it? “Using the laser may improve results by 1 or 2 percent, but you’re going to be spending a half million dollars and slowing yourself down to get a very small improvement,” notes Dr. Newsom. “And unfortunately, I suspect the surgeons who can afford to purchase one of these new systems are the high-volume surgeons, the most-experienced surgeons, who already do a great job with all the parts of cataract surgery. The surgeons that could really benefit from this laser are your beginning surgeons and your less-experienced surgeons. It would give them perfect incisions and capsulotomies and make the surgery easier. The problem is, it’s priced so high that those surgeons won’t have enough volume to be able to afford a laser like this.”
Dr. Newsom believes this could change as residents in training become comfortable with performing laser cataract surgery in upcoming years. “When residents start training on the laser system, they’ll be doing fewer manual cases, and that will lower their comfort level with manual surgery,” he says. “I seldom do scleral tunnels any more, so my comfort level with that procedure is quite low. I expect the same thing will happen once residents are using the laser system. If they don’t feel comfortable doing manual surgery, demand for the laser system will probably increase dramatically.”
A Marketing Advantage?
One point that is often made in favor of adopting this technology for cataract surgery is that bladeless cataract surgery will draw patients in and leave femto-less competitors in the dust. Mr. Pinto, however, is skeptical of the marketing value of femtosecond cataract surgery, both because of the cost and because it may not be the overpowering marketing tool that some believe it will be.
“Minimizing and then eliminating the use of a blade did have a significant marketing benefit during the switch from RK to LASIK,” notes Mr. Pinto. “However, profound clinical, outcome and economic benefits also attended that transition; it wasn’t just a marketing point. Given the current economic situation, it’s questionable whether the same arguments apply. If we were talking about a $5,000 or $50,000 device, I think that the argument of marketing benefit would hold a lot of water, even if it were producing results equivalent to those of manual surgery. But when you’re talking about a $500,000 tool, it’s hard to argue for it on the grounds of elegance, patient confidence or marketing alone.
“Furthermore, it may not be an unbeatable marketing tool,” he continues. “I’ve spent billions of dollars of other people’s money proving what works and doesn’t work in the marketing/communications arena for the typical ophthalmology practice. Suppose we were going to have a shootout at the OK Corral between two otherwise equivalent cataract practices with the same marketing budget. One was going to use as their chief sales position: ‘Come to us, we’ve got the femtosecond laser.’ If I was marketing the other practice, and I had an open hand to use whatever other marketing points I chose, including the tenure of the practice in the market, the quality of the physician and other features and benefits of the practice, I think I’d win hands down every time. In fact, I’ve seen this over and over again with each new iteration of LASIK technology and cataract technology. The advertising-oriented practices that focus their marketing on the unique selling points of the new technology fare worse than the practices that stick with bread and butter appeals.
“Again, if this were a $5,000 or $50,000 tool, I’d encourage most clients to get it, even if the only benefit was marketing,” he says. “But it’s hard to build a case for it at the current price. The proof of that is that these devices aren’t getting placed. I recently spoke to a senior executive of one of the major companies active in Canada. I asked him, ‘What’s the buzz surrounding femtosecond laser cataract?’ He told me there was plenty of buzz, but no one was purchasing the units. I’m sure it’s very frustrating for the executives of the companies to figure out how to position this in the current environment.”
Some have noted that the femtosecond laser has done well in the LASIK arena, where it may become the dominant method for making LASIK flaps. However, Mr. Pinto doesn’t see this as a good parallel to the use of the laser for cataract surgery. “LASIK is a marketing-dependent procedure, unlike cataract surgery,” he notes. “The vast majority of cataract cases being done are not patient self-referrals. Most of them are referrals from other doctors, or you’re operating on patients who were already in your practice; the time has just come for the cataract to come out. The amount of marketing communication dollars being spent in the cataract arena is much lower than what’s being spent in LASIK. The bottom line is, buying an expensive tool to potentiate the marketing oomph of your LASIK practice is a much stronger argument than buying it to market your cataract practice.”
Other Ways to Go Bladeless
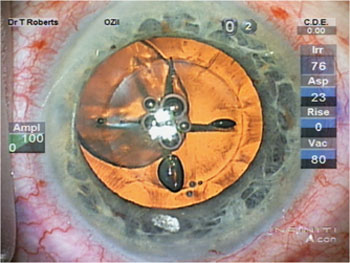
Even if it turns out that bladeless cataract surgery is a selling point, surgeons who have already invested in a LASIK laser may be able to make the same claim, thanks to a new device invented by Dr. Newsom. Dr. Newsom’s device is a small, inexpensive metallic disc that fits into the bottom of the Intralase interface cone. When the Intralase is set to create a circular incision for keratoplasty, the new device prevents the laser from making most of the incision, only allowing it to be made in the desired section of the cornea, thus creating the cataract incision. The laser can also make arcuate incisions to treat astigmatism using this approach, although it cannot perform a capsulorhexis or soften the nucleus. Nevertheless, it does eliminate the need for a blade during cataract removal.
Rhein Medical is working with Dr. Newsom to produce the device, which may be available for purchase in time for the 2012 American Society of Cataract and Refractive Surgery meeting in April. He’s begun conducting training courses at his office and will be offering courses at the major ophthalmology meetings as well. (Although the laser is approved for making lamellar cuts into the cornea, the disc is not approved by the Food and Drug Administration, so its use for this purpose is off-label.)
Dr. Newsom isn’t worried about the fact that this approach doesn’t allow him to create the capsulorhexis or soften the nucleus. “I think this approach makes a better cataract incision and LRI than we can make manually,” he says. “And patients do respond when they hear that the procedure is bladeless. This approach allows a surgeon who already owns a LASIK laser to offer that benefit without the economic risk.”
Dr. Newsom adds that his invention will eventually be outmoded. “AMO can simply change the software in its laser and make my disc obsolete,” he points out. “That will eventually happen, but the company will have to get a 510K approval from the FDA, which can take a couple of years to do. In the meantime, this inexpensive device should allow many surgeons to use their existing LASIK lasers to do bladeless cataract surgery.”
Will It Undermine Efficiency?
Although some surgeons who have used a laser cataract system for six to 12 months report that their patient throughput has returned to roughly the same level as when they performed manual cataract surgery, prospective purchasers remain concerned. Dr. Newsom says his experience using the Intralase to create the incisions hasn’t relieved those concerns at all. “When doing manual surgery I usually walk into the OR and leave the OR within a six- to nine-minute window, whether I’m doing a premium IOL or not,” says Dr. Newsom. “The fastest I’ve been able to accomplish cataract surgery using the Intralase to make the incisions is 16 minutes.”
Dr. Newsom adds that his protocol using the Intralase should be even faster than that of someone using a dedicated machine, because he has his laser in the OR rather than in a separate room. “However, we have to seat the patients, line them up, make them comfortable, hook them up, spend 90 seconds doing the laser and unhook them from the laser,” he points out. “We move the stretcher three feet over, put a drape on the patient and do the cataract surgery. In most cases this requires 20 to 22 minutes. We do about three cases per hour using the femtosecond laser to make the incisions, where we typically do about eight cases per hour with standard manual phaco. If we had the laser in a separate room, it would mean even more moving of the patient. Based on my experience, I can do 30 to 40 manual cataract surgeries in a day, but it would take me two or three surgical days to do the same number if I made all incisions using the laser. That’s certainly not an economic benefit.
“Of course, there’s no doubt that over time, as more people perform laser cataract, it will become more efficient,” he adds. “We’ve seen that using our protocol. Our first few cases took us 30 minutes apiece; now our best time is 16 minutes. It’s getting better, but it’s still a long way from saving us time.”
|
The Next Big Thing?
“After 33 years in this industry, I haven’t seen anything like this level of enthusiasm for a new technology that seems very limited in terms of potential science, clinical or business benefits,” says Mr. Pinto. “I see plenty of reason to doubt that this will be the next big thing. At the same time, I know there are lots of thoughtful people who have a contrary opinion, and I’ll be the first to admit that I could be 180 degrees wrong. Ten years from now, it may seem as primitive to do a manual capsulorhexis as it would be to do a planned extracap today.
“I think the jury is not only out of the courtroom, but out of the building,” he concludes. “It’s going to take years before we have the answer. If the first units placed in the risk-taking first-adopter practices work clinically, it should be obvious. And it should only take a few years to see whether the business model works out with the present generation of devices and current price points. If it does, people will say, ‘Now we’ve got 10 empiric examples of this really being a success. I’m going to get into it too. Let’s mortgage the house!’ But I don’t think the answer will appear too quickly. I suspect that two years from now we’ll still be scratching our heads and saying, ‘This still doesn’t seem to work in terms of the value gained for the cost expended.’ One way or the other, time will tell.” REVIEW
Dr. Pascucci and Mr. Pinto have no financial ties to any company or device discussed. Dr. Newsom developed his disc with Rhein but will not receive royalties from its eventual sale.