|
Here, three surgeons share their reasons for believing that femtosecond cataract surgery will produce better results than manual surgery, thanks to more accurate astigmatic arcuate incisions; a more “perfect” capsulorhexis; being able to soften the nucleus; creating fewer complications; and—at least in some respects—increasing efficiency.
Treating Astigmatism
Jack T. Holladay, MD, MSEE, FACS, clinical professor of ophthalmology at Baylor College in Houston, sees femtosecond laser cataract surgery as offering a dramatic improvement in surgeons’ ability to make both consistent cataract wounds and extremely accurate astigmatic arcuate incisions. “The incisions a surgeon makes with the laser will be much more precisely placed on the cornea and repeatable than can possibly be made manually using a diamond knife,” he notes. “Both cataract incisions and arcuate keratotomy incisions are going to be substantially more precise. You can’t make an arcuate incision at exactly 43 degrees, exactly 80 percent of the measured depth of the cornea and exactly 46 degrees in arc width, using a diamond knife—I don’t care how good you are.
“Most cataract surgeons don’t do refractive surgery,” he continues. “About 80 percent of them are not comfortable making arcuate incisions in the cornea to correct astigmatism. That’s why the arcuate incision has never become the predominant method for correcting astigmatism, and the toric lens has increased much more rapidly than arcuate keratotomy. But that’s going to change, because the cataract surgeon won’t have to make that precise incision himself. A nomogram in the laser will determine where to put it, and how wide and deep to make it. The surgeon will just press a button.“
|
Dr. Mackool says so far, the laser has been great at incisional astigmatic surgery. “It makes perfect cuts, and our results are really excellent,” he says. “More than 95 percent of the patients treated for astigmatism have demonstrated less than 0.5 D of residual astigmatism two weeks after the procedure. No one can make manual incisions of a predictable, consistent depth the way the laser can.”
Better Than Torics?
Today, toric IOLs have become increasingly popular as a means to address regular astigmatism, but Dr. Holladay points out that arcuate incisions have some key advantages over toric IOLs. “An arcuate incision is more forgiving and may produce better outcomes than toric lenses when we’re dealing with higher levels of astigmatism,” he says.
“Suppose a patient has 4 D of corneal astigmatism,” he continues. “In a normal eye you need about 6 D of cylinder in the IOL to offset that corneal astigmatism. You’re actually trying to balance the cylinder at the corneal plane with cylinder from the IOL. If you line up that toric IOL absolutely perfectly, you’ll end up with a wonderful result. However, studies have found that surgeon accuracy of rotational placement is about ±7 degrees. That discrepancy is caused by factors such as the visual axis used in keratometry not being the same as the anatomic center of the cornea used at surgery. So perfect toric IOL alignment is hard to achieve. If the surgeon is 10 degrees off with a 6-D lens, he’s going to end up with 35 percent of the original astigmatism or about a diopter and a half of residual astigmatism at the corneal plane, which is unacceptable.
“In contrast,” he says, “if the surgeon addresses the astigmatism by making two 90-degree arcuate incisions at the steep axis, what he’s doing is reducing the power of the astigmatism to about +1 D. The point is that arcuate incisions reduce the astigmatism to a smaller amount, whereas with a toric IOL we’re using plus and minus lenses to neutralize each other. The smaller remaining cylinder in the cornea is much more forgiving. Furthermore, an error made with an arcuate incision has far less consequence than the same error made with a high-power toric IOL. Suppose the cornea has 6 D of astigmatism at 90 degrees, and the surgeon ends up with the toric IOL at 80 degrees. Not only will this leave residual astigmatism of about 2 D, but the residual astigmatism will not appear halfway between those two angles at 85 degrees. Instead, the residual astigmatism will appear at 130 degrees, oblique to the corneal astigmatism and the IOL.
“If an arcuate incision were to be off by 10 degrees, it would still reduce the astigmatism down to about 2 D, and the residual astigmatism would be halfway between those two angles,” he says. “And when the laser is making these incisions they’ll be incredibly precise; a typical laser tolerance is 1 degree. Furthermore, the targeting will be based on registration of specific features of the patient’s iris with the same device that measured the astigmatism to begin with.
“Of course, this level of precision will require more precise astigmatic nomograms,” he says, “but those will be developed as data from use of the laser comes in. With the variability of manual incisions eliminated, we’ll see the true variability introduced by things like the age of the patient, the IOP, the magnitude of the corneal astigmatism and the location of the steep axis of astigmatism—all of the things that currently are below the noise level the surgeon introduces. You won’t see any 10-degree errors unless something is seriously wrong.
“For that reason, I believe we’ll see a transition from toric lenses back to arcuate incisions as the femtosecond laser begins to take hold and increase its percentage of the marketplace in the next year or two,” he concludes. “And I think this will give us one improvement in outcomes that we’ll be able to quantify, to show the superiority of femtosecond incisions over manual incisions.”
A ‘Perfect’ Capsulorhexis
“There’s no question in my mind that the laser can make a better capsulorhexis than you can make manually,” says Dr. Holladay. “And if the capsulorhexis is more regular, or more circular, and it’s placed exactly where you want it to be, then it’s possible that we’ll get a more consistent centration and positioning of the IOL. For example, a symmetrically circular capsulorhexis may make a difference in the lateral position, in terms of centration, which in turn can have a small effect on the IOL power calculation.
“However,” he continues, “that effect might not be significant. It’s possible that when the capsule begins to contract and opacify peripherally, having a perfectly centered lens with an even capsule overlap will equalize the forces and result in a lens that doesn’t move at all. But of course, nature doesn’t always follow simple logic. So we’ll have to see whether a perfectly circular capsulorhexis has any impact on the lateral and axial (effective lens) position of the IOL after surgery.”
Dr. Holladay notes, however, that a more circular capsulorhexis could have an effect on posterior capsular opacification. “Ideally you want the rhexis to cover the outer quarter- or half-millimeter of the lens, and you want it to overlap the lens all the way around, uniformly,” he says. “Studies have shown that two things help to reduce PCO. First, a sharp posterior IOL edge pushed against the posterior capsule helps prevent epithelial cells from getting under the lens onto the posterior capsule. Second, a consistent overlap by the anterior capsule sequesters the epithelial cells into the little peripheral chamber that’s created along the edge of the lens, and they can’t get out. There’s a much better chance that you can get that perfect overlap with the femtosecond laser than manually.”
Softening the Nucleus
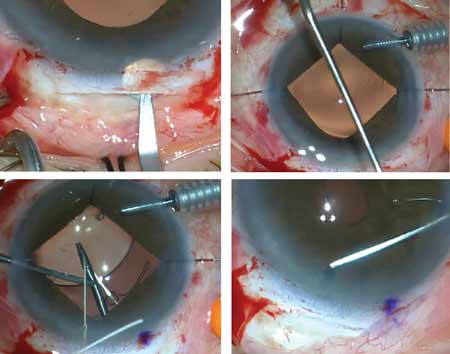
Dr. Mackool says he’s most impressed by the femtosecond laser’s ability to facilitate the division of the nucleus. “We’ve tried different approaches with this part of the procedure,” he says. “We tried dividing the nucleus into four pieces or six pieces, adding circumferential cuts, and so forth. Sometimes the laser would divide one part of the nucleus well but not another, and we weren’t sure why. But this is the kind of thing that gets worked out over time. We’ve learned to dock the laser more accurately, for example.
“Now we’ve settled on an approach that works well for us, and it’s not uncommon for the entire division and removal of the nucleus by phaco to take less than 60 seconds,” he says. “That’s from the moment you introduce the phaco handpiece to the moment you remove the last piece of nucleus.”
Dr. Mackool sees several advantages to facilitating the removal of the nucleus. “First, removal of the nucleus is clearly the most difficult part of phaco, and the most difficult part of removal is dividing the nucleus,” he notes. “After using the femtosecond laser the nucleus divides easily and removing the segments is pretty simple. So, this tool helps you with the hardest part of the surgery. That’s huge. Furthermore, if it takes less time to divide and remove the nucleus, there are clearly benefits to that, including less trauma to the eye. You’re running less fluid through the eye, manipulating tissue less and preserving more endothelial cells.”
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Dr. Mackool sees this as potentially affecting refractive outcomes as well. “The other thing that manipulation inside the eye does is stress the zonule,” he points out. “People have theorized that it’s a more consistent capsulorhexis that gives you a more consistent effective lens position, but the tautness of the zonule is what determines the position of the IOL. So to the extent that you don’t stress the zonule, I think you’ll end up with a more predictable ELP.
“Is a more consistent capsulorhexis a desirable thing? Of course,” he adds. “But those of us who’ve done tens of thousands of these surgeries can do a good capsulorhexis and get the edges on the optic 360 degrees pretty much every time. So when a surgeon like Bob Cionni reports that in his hands ELP is more predictable with the laser, I suspect that the reason is that the division of the nucleus is less traumatic. It doesn’t stress the zonule as much, so lens position becomes more predictable.”
Overall Refractive Outcomes
Although clinical evidence is still lacking, some surgeons are reporting better refractive outcomes. One of the first locations to purchase the Alcon LenSx femtosecond system was the Vision Eye Institute in Sydney, Australia. They began using the system in April 2011; to date they’ve performed more than 1,300 laser cataract procedures. Tim Roberts, MBBS, MMed, FRANZCO, FRACS, a consultant ophthalmic surgeon at the Royal North Shore Hospital and clinical senior lecturer at the University of Sydney, says he’s performed more than 350 laser cataract surgeries.
“I compared the absolute difference and standard deviation from intended spherical error in a series of 40 manual cataract procedures using the AcrySof IQ IOL, vs. the initial 114 laser cataract procedures using 67 AcrySof IQ lenses and 47 Zeiss AT TORBI toric lenses,” he says. “The results were better with laser cataract surgery. The absolute difference from the intended spherical equivalent was 0.39 ±0.3 D in the manual group; it was 0.27 ±0.25 D and 0.31 ±0.24 D respectively in the laser groups. With enhancements in laser technology and surgical technique I would expect these results to improve further.”
Other surgeons are less certain that their outcomes are significantly better. “Outcomes with the laser are no better than your best outcome in your best manual case,” says Dr. Mackool.
“If I do a really challenging case with the laser—a denser nucleus, or pseudoexfoliation—I don’t know how that would have come out if I’d had to spend more time in there chopping and stressing the zonule. I don’t have a controlled study. But I know when things are easier.”
Dr. Mackool notes that even if no one can prove that the laser produces better outcomes right now, the technology keeps improving. “The LenSx laser is getting faster and faster,” he points out. “What used to take us two minutes to do with the femtosecond laser now takes 20 seconds—and that makes it more reproducible because the longer something takes, the greater the possibility that the patient will move or squeeze his eye, leading to an incomplete cut or a partial treatment. I just watched the video of a case done by my son, where the eye had a moderately dense nucleus, close to a grade 3; he did the entire phaco following the femtosecond laser in 42 seconds. The nucleus fell into six little pieces, and he quickly removed them. Not many surgeons could do a case like that in less than three to five minutes.
“This increasing speed means that results will be better in the future,” he adds. “They’re already better than when we started with the laser, and a part of that is that the laser is faster. This technology has tremendous potential, and it already achieves that potential in a significant percentage of cases. And, it keeps getting better.”
Complications
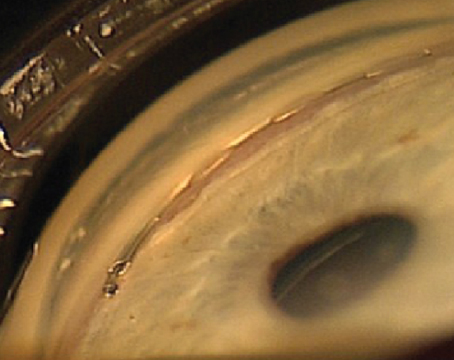
Early adopters have reported some problems at the outset, although it appears that these problems are attributable to the human learning curve, not laser error. Dr. Roberts’ group in Australia published a study in 2011 reporting an uncommon complication they encountered during their early use of the LenSx system.1 The report focused on two of their first 50 patients, who developed intraoperative capsular block syndrome. Although the corneal incisions, capsulotomy and laser fragmentation were uneventful, following hydrodissection in the operating room the surgeons discovered posterior capsule rupture, resulting in posterior dislocation of the lens; this required pars plana vitrectomy, removal of the lens and sulcus IOL implantation. (Final visual outcomes were good in both patients.)
The authors note that use of the femtosecond laser to fragment the nucleus causes changes in the intraoperative environment, including the generation of intracapsular gas. They also note that after modifying their surgical technique in response to these events, no further events of this kind occurred in the next 550 cases. However, even though their 2011 report indicated that the intraoperative problems were eventually resolved, it added to many surgeons’ concern about the safety of the laser cataract approach. (Importantly, Dr. Roberts notes that a careful review of the surgical recordings and laser parameters confirmed that the femtosecond laser performed exactly as programmed; there was no evidence of photodisruption of the posterior capsule.)
“All of our surgeons using the new system experienced a learning curve, although previous experience with a femtosecond laser in the refractive setting helped to flatten the curve,” says Dr. Roberts. (A second report outlining their group’s early clinical experience is currently in press.2) “Since the initial installation, the unit has undergone several software upgrades, and with greater surgical experience our femtosecond cataract surgery now consistently results in a superior wound, a more circular and consistently sized capsulotomy, and a reduction in the average phacoemulsification energy used and time required compared to routine manual surgery. Furthermore, the rapid evolution of the software/laser algorithms and surgeon experience has resulted in a significant decrease in complications. All of this should translate to a safer, more accurate outcome for patients.
“The initial complications we experienced reflected the learning curve and the realization that ‘laser phaco’ is different from manual phaco,” he continues. “Differences include that laser-generated gas increases the capsular bag volume; laser nuclear fragmentation requires changes in surgical technique; the laser-cut capsulotomy seals perfectly; the laser induces changes in the cortex; and a deep anterior chamber isn’t required for continuous curvilinear capsulorhexis.
“Our experience has shown that awareness of the changed intraocular environment and appropriate modification in surgical technique makes laser cataract surgery as safe and predictable as manual surgery,” he says. “The learning curve is similar to when phacoemulsification was introduced and surgeons converted from performing manual extracaps. Our complication rate is now trending lower than with manual cataract surgery.
“As the safety level and our results have improved with experience, all of our operating surgeons now perform laser cataract surgery in the majority of suitable cases,” he adds. “Unsuitable cases include eyes with corneal opacities and scars, a small pupil, too narrow a palpebral fissure or advanced glaucoma. These conditions can make laser cataract surgery technically impossible, or inadvisable due to the induced IOP rise.”
Dr. Holladay believes early problems with a new laser are inevitable. “I’m sure there will be technique and algorithm adjustments over time,” he says. “But I’m also sure it won’t be a long learning curve. This is the first generation of these instruments, so there will be improvements in every area, just as there were with the Intralase. But these things won’t be an impediment to the penetration of the femtosecond laser in the cataract arena.”
The Efficiency Factor
Another concern that many surgeons have expressed relates to the extra time required to move patients in order to incorporate the laser into the procedure. However, surgeons who have used the laser for several months say this problem is mitigated by clever patient management and increasing experience.
“It does take time to use the femtosecond laser, even though the laser reduces the time the phaco takes, and that reduction will get more and more significant as it gets better at dividing the nucleus,” says Dr. Mackool. “The patient has to be moved from the laser area to the OR, and that takes time.
“So, how can we do that on limited dollars?” he asks. “I think the answer is that one surgeon can do all of the femtosecond treatments in one room, while another surgeon does all the phacos in the OR. This can be very efficient. We’ve already learned that patients can wait hours between the femtosecond part of the procedure and the phaco with no ill effects, so you don’t have to worry about rushing patients from one area to the other.
“For example,” he continues, “in my practice my son now does all the femtosecond treatments on one floor of the building. Then, we bring the patients down to the OR. If it’s my patient, I do the phaco. If it’s his patient, when he’s done doing the femtosecond treatments he comes down and does all of his phacos. The OR doesn’t go unused for much time at all.
“We are definitely not doing fewer patients because of the laser,” he adds. “I think eventually we’ll be doing more patients with the laser than we could manually.”
| |||||||||||||||||||||||||
Dr. Holladay observes that when the Intralase first became available surgeons were also concerned about the extra time required to use it. “Surgeons pointed out that it was much faster to simply get the patient under the laser, use a microkeratome and do the procedure,” he says. “They worried that having to move the patient from room to room was going to ruin their flow and reduce the number of patients they could treat in a day.
“Did that have any impact? No,” he says. “When patients really want something, you’d better adjust your flow to accommodate that, or you’ll have plenty of time because all of the patients will be going to the guy down the street.”
Guarded Optimism
“I was around when phaco was introduced, and it had some real problems,” notes Dr. Mackool. “But it was clear that when it worked well it was better than anything we could do at the time. And that statement is absolutely true in the case of femtosecond laser cataract surgery. I think this new approach will have an adoption curve like phaco’s, but faster. I predict that in about five years the majority of cataract operations in the U.S. will have at least some part done with the laser.”
Dr. Roberts believes laser cataract surgery will prevail in the long run, but does see economics slowing the changeover. “You have to perform a minimum number of cases to make purchasing a laser cataract system viable,” he points out. “Nevertheless, I believe within five years the majority of cataracts will be removed using the laser.” REVIEW
Dr. Mackool is a consultant for Alcon/LenSx. Dr. Holladay is a consultant for Alcon/LenSx and AMO. Dr. Roberts has no financial interest in any related companies or products.
1. Roberts TV, Sutton G, Lawless MA, Jindal-Bali S, Hodge C. Capsular block syndrome associated with femtosecond laser-
assisted cataract surgery. J Cataract Refract Surg 2011;37:
11:2068-70. Epub 2011 Sep 22.
2. Bali-Jindal S, Lawless MA, Hodge C, Roberts TV, Sutton G. Early experience with the femtosecond laser for cataract surgery. Ophthalmology (in press).