Optical coherence tomography is widely used by today’s ophthalmologists, and as the technology improves, new ways to take advantage of its capabilities continue to appear. One that’s gaining favor is using OCT to examine the macula before performing cataract surgery. Here, three surgeons discuss their experience and recommendations when using OCT for this purpose.
Premium Lens Precautions
Ike K. Ahmed, MD, FRCSC, assistant professor at the University of Toronto in Ontario, Canada, says he uses posterior OCT when cataract patients are receiving premium implants. “Given today’s patient expectations, any tool that helps us determine the appropriate premium lens technology and the likely postoperative outcome works to our benefit,” he says. “I find that use of macular OCT is very helpful in these cases.”
|
Steven G. Safran, MD, PA, a cornea specialist practicing in Lawrenceville, N.J., who specializes in dealing with complications arising from cataract surgery, uses posterior OCT to scan the macula before implanting premium IOLs and to examine patients referred to him for complications following cataract surgery. “To me, this is a completely indispensable piece of equipment,” he says. “I’m not sure I can evaluate a patient properly without it. I would personally never implant a multifocal without screening the patient’s retina with OCT. And if I had someone coming from out of town for a consultation—perhaps an unhappy premium IOL patient—if my OCT unit wasn’t working I’d probably cancel the appointment.
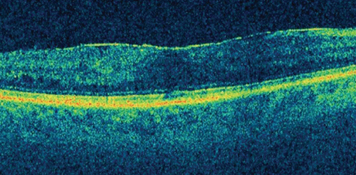
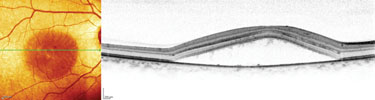
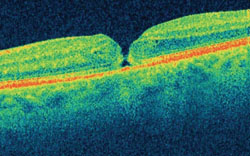
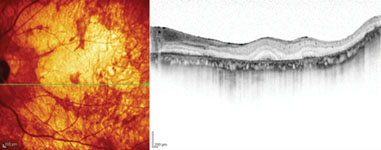
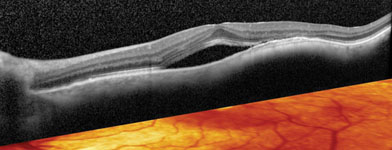
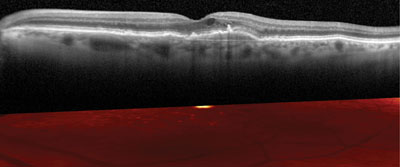
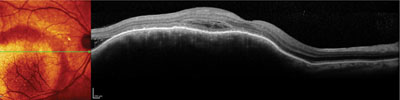
“OCT, especially spectral-domain OCT, will pick up all kinds of things that you simply can’t see with the naked eye,” he continues. “Sometimes I tell patients that looking at the retina with a 78-D lens or an indirect ophthalmoscope is like looking at a satellite photograph, whereas OCT is like having a jeep on the ground. You can see vitreomacular traction, lamellar holes and epiretinal membrane—and you’ll know if the epiretinal membrane is distorting the macular architecture.
You’ll be able to tell if there are choroidal issues such as central serous retinopathy. I’ve detected retinitis pigmentosa, macular nevi and subretinal neovascularization leakage. Given that this equipment is readily available, to my mind it’s indefensible to miss macular pathology that could have been picked up by it.”
|
Dr. Safran notes that the potential downsides of premium lenses have to be offset by the key feature that people are paying for. “A multifocal lens is like a convertible,” he says. “If you can’t put the top down, you don’t want it. A convertible comes with more wind noise, it’s less structurally sound, if you flip over while driving it you’re going to be killed and if someone wants to break into your car they can do it with a butter knife. There are a lot of disadvantages to a convertible, and the same is true with a multifocal. So you have to make sure that the big benefit the patient is paying for works as advertised. That means you have to know what’s going on with the macula before you give somebody a multifocal lens. You have to rule out macular pathology, or the likelihood that the patient will have macular pathology.”
What About Monofocals?
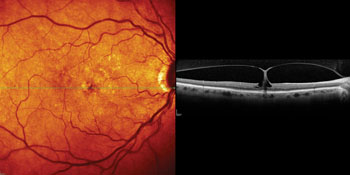
Joel S. Schuman, MD, chairman of the department of ophthalmology at the University of Pittsburgh School of Medicine, director of the UPMC Eye Center and professor of bioengineering at the University of Pittsburgh, believes that OCT can be worthwhile even if a patient is only receiving a standard monofocal IOL. “If that patient has an epiretinal membrane and ends up with macular edema, he’s not going to be happy if he expected to be 20/20 or 20/15 postop,” he says. “The same is true with preexisting macular edema. The point is that if the cataract isn’t the primary or sole cause of the visual impairment, taking the cataract out won’t result in the patient recovering excellent vision postoperatively.
“These conditions are surprisingly common—especially epiretinal membrane,” he continues. “Of course, most cataract patients will do extremely well, and being unaware of an epiretinal membrane preoperatively may not influence the outcome if the patient doesn’t develop macular edema following surgery. But the risk is certainly higher if the patient has an epiretinal membrane, and I’d rather have the patient be prepared for the possibility of imperfect vision when he recovers than have him expect better vision than I can give him. For that reason, I think retinal OCT is worth doing on all cataract patients, whether they’re receiving a monofocal or premium IOL.”
|
Advantages of Posterior OCT
The knowledge gained by using posterior OCT before cataract surgery has a number of potential benefits:
• It sets appropriate patient expectations. “Preoperatively I think it’s very important to know if there’s any macular pathology,” says Dr. Schuman. “It allows you to direct treatment appropriately, and importantly, it helps you to set appropriate patient expectations. If patients have appropriate expectations, it’s unlikely they’ll be disappointed with the outcome. But if their expectations exceed what you’re realistically able to provide, you’ll probably end up with an unhappy patient.” Dr. Schuman says he usually does the OCT right before he discusses surgery with the patient.
|
Dr. Ahmed agrees that it’s very important to give the patient an idea of what his vision will be like postop, or at least warn him if there may be a concern. “A lot of these conditions are pre-existing,” he points out. “Epiretinal membrane doesn’t happen overnight, so if ERM turns up after cataract surgery, it was probably there beforehand. But if there’s a problem postoperatively, patients have a tendency to think it was caused by your surgery. And why wouldn’t they think that? The bottom line is, if you identify the problem beforehand, it’s the patient’s problem. If the problem is diagnosed after surgery, it becomes your problem.”
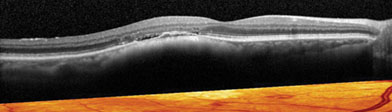
• It’s a powerful tool for patient education. “Having the OCT to show to the patient is an incredibly useful teaching tool,” says Dr. Schuman. “I always show it to the patient if there’s any pathology that I think might limit the postop visual outcome. It takes a couple of extra minutes, but patients seem to understand what they’re seeing in the scans. I say, ‘Here’s what a normal macula looks like,’ and then show them the differences in their macula. If they have an epiretinal membrane, I can show them the extra line on the surface of the retina and explain how that could limit their vision postop by pulling on the retina and causing swelling. Macular edema is usually easy to see; you can see the swelling of the retina and the loss of the normal foveal contour. I think the ability to show patients these images really helps to facilitate their understanding of why they might run into problems postop.”
|
Dr. Safran agrees that OCT scans are a big help with patient education. “If a patient comes in with an epiretinal membrane or some other macular problem, I don’t even try to explain it to the patient until I have the OCT in front of me and I can illustrate the problem,” he says. “It’s a huge time-saver.”
• It’s a great tool for resolving postop problems. “When a patient who’s unhappy with his premium lens is referred to me for a second opinion, it’s critical to have corneal topography and OCT to isolate the source of the patient’s complaint,” says Dr. Safran. “You want to know what’s going on with the cornea and retina. Those are the two pieces of information you need. And of course, OCT can help with both the anterior and posterior segments.”
Dr. Schuman also relies on OCT if a patient doesn’t achieve the postop level of vision he was expecting. “Sometimes a patient with a 20/30 visual outcome will have some macular edema that you didn’t pick up on your fundus exam,” he says. “That will show up plainly on OCT, so you can direct your therapy appropriately, as well as explain to the patient exactly what’s going on in his eye. I usually will only do OCT postop if there’s a problem, and usually insurance will cover the test because it’s being used to manage pathology.” Dr. Schuman adds that he seldom uses fluorescein anymore to test for macular edema because he can see edema so clearly with OCT.
Other Issues
Use of OCT to check the macula before cataract surgery raises a few questions and concerns:
• Is time-domain OCT acceptable for this purpose? Dr. Schuman notes that time-domain OCT can show you the pathology quite well, in the absence of spectral-domain OCT, but it does have some limitations. “The pictures are clearer with SD-OCT,” he says, “and with most SD-OCTs you’ll have more data, so you’re not as likely to miss the pathology. In time domain, if you’re not scanning right in the area of the pathology, you’re going to miss it.”
• Will OCT always work? Dr. Safran notes that it’s rare to find a cataract patient on whom posterior OCT doesn’t work. “I use the Heidelberg instrument, which has tracking technology that allows you to over-scan images,” he explains. “If necessary, you can build an image out of 100 scans through very cloudy media. It’s a pretty impressive capability. I used that feature recently on a patient who was referred to me. I couldn’t see a thing, but the OCT revealed a retinal detachment.”
|
• Is using posterior OCT the standard of care? “Not doing a posterior OCT before implanting a multifocal lens in this day and age is like driving without car insurance,” says Dr. Safran. “You won’t have a problem until you get in an accident. If a patient has a poor outcome because of macular pathology that isn’t picked up until after the surgery, and the patient is then told by a retina specialist or another ophthalmologist that a multifocal lens, or even the cataract surgery itself, might not have been the best option, it places you are in a difficult position. Saying you weren’t aware of this problem because you don’t have an OCT simply won’t cut it. From my personal perspective, posterior OCT preop is becoming the standard of care for premium IOLs today.”
Dr. Ahmed, however, notes that it may be premature to call use of posterior OCT in cataract surgery standard of care. “I think it’s helpful, and I think it should be considered when you have clinical suspicion,” he says. “I look at it as an adjunct, a valuable tool. But I don’t know if I’d go so far as to call it standard of care. If you feel it’s standard of care in your practice in your community, with your clinical skills, then it’s your standard. But if someone chooses not to use posterior OCT in a particular case, I don’t think that’s a problem.”
• Is it possible to rely on it too much? “I think if we had our way, we’d do macular OCT on every cataract patient,” says Dr. Ahmed. “But it becomes a cost and capability issue. That’s why surgeons tend to reserve it for the premium patients. Those are the patients with the highest expectations, and those that require the highest level of precision. If I have a premium patient, or a patient for whom I’m not sure about the condition of the macula, I definitely want to have an OCT. But if it’s a routine, non-premium patient and I have a good clinical exam, I get a good look at the macula, the patient has a reasonable history and visual acuity is just slightly deteriorated, then I don’t think it’s something that will give you a high yield. So I don’t do it routinely, for practical reasons.”
Dr. Ahmed sees another downside to using posterior OCT on every cataract patient. “It’s easy to get a bit too reliant on technology and use it as a crutch,” he notes. “Just because we have a tool doesn’t mean we have to use it for every patient. If we had that philosophy for every piece of technology, we’d be testing constantly and it would put a huge cost burden on the health-care system. I think it makes sense to have some guidelines for using this technology in this situation, and we’re still figuring that out.”
|
• What about reimbursement? Dr. Schuman notes that insurers may not cover OCT testing for cataract patients. “That means that you may need to determine whether the patient’s insurer is willing to pay for the OCT exam preop,” he says. “If not, you’ll have to do the exam gratis, or charge the patient for it. In some states doctors are still fighting to have OCT reimbursed when a patient has glaucoma.
“I think the utility of OCT is very clear,” he adds. “Nothing else can show you the pathology the way OCT can. But it’s a problem that some insurers will pay and some won’t, and that limits doctors’ willingness to use the technology.”
Dr. Safran doesn’t see reimbursement as a problem. “First of all, insurers will reimburse you for using OCT if there’s pathology,” he points out. “So if you see something and you think it needs to be evaluated by OCT, you can bill for it. If you’re using OCT because you’re implanting a multifocal lens, it’s part of the package that patients are paying for. Part of that fee is meant to cover testing, including OCT. Besides, if I find something with OCT that makes me decide not to implant the multifocal, I’m extremely happy that I did it. And then it’s covered by insurance anyway because the patient has pathology.
“It’s so safe and easy to do an OCT,” he continues. “It doesn’t take long and there’s no risk to the patient. If I need the information, the last thing I’m worried about is whether I’m getting paid for it. If you were going to do LASIK and you couldn’t charge the patient for topography, would you not do the topography? You have to do it. You need the information. I’m very happy that I get paid extra to implant multifocals and the Crystalens, but part of that package is knowing what’s going on with the macula so I can give the patient the right advice. Yes, we do want to get paid for using OCT over the long haul with most of our patients. But in this situation I don’t worry about it.”
Another Valuable Tool
“Posterior segment OCT has come a long way,” notes Dr. Ahmed. “We use it in undilated pupils, we use it even with moderate density cataracts, and with spectral domain the speed and reliability has been enhanced greatly—although I think time-domain OCT can do a reasonable job, too. It’s a relatively straightforward, easy-to-use technology, and I think more and more cataract surgeons are using it. Most of them have access to OCT because use of OCT has exploded over the past four or five years; it’s now found in most offices and hospitals.
“Comprehensive cataract surgeons have been using OCT to deal with retinal issues for some time now,” he adds. “I think using it for cataract surgery just adds another confidence-builder, in terms of predicting the outcome.” REVIEW
Dr. Ahmed is a consultant for Carl Zeiss Meditec; Dr. Safran has given paid talks for Heidelberg; Dr. Schuman is co-inventor of optical coherence tomography.