 |
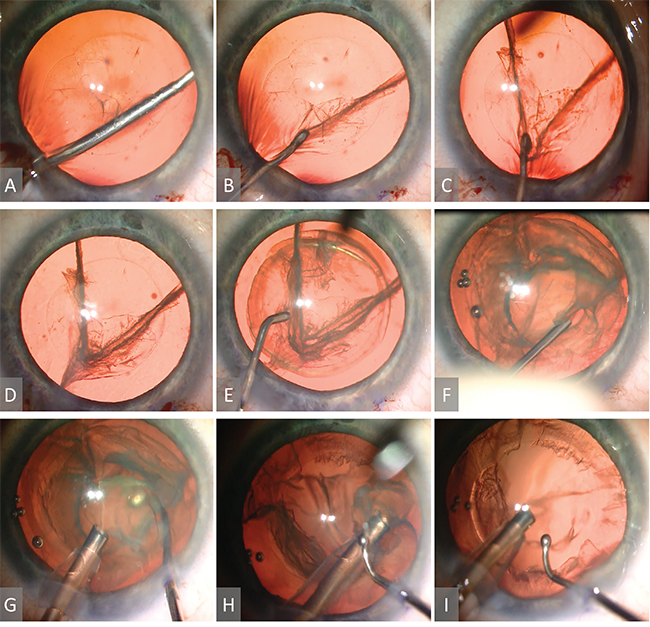
| Figure 1. After the capsulorhexis is completed, a blunt tipped instrument is slipped beneath the anterior capsule at the 7-o’clock position and around the lens equator (A). It is then gently passed through the nucleus at approximately 50-percent depth towards the 12-o’clock position (B). This procedure is then repeated, slicing from 5 to 12-o’clock, to produce a central pie-shaped portion and two lateral crescentic pieces (C,D). Gentle hydrodelineation and hydrodissection are then performed (E), and viscoelastic is injected into the grooves between the three segments (F). The phaco handpiece is inserted into the main wound and the central pie-shaped piece is removed (G), after which, the two remaining pieces are gently aspirated by turning the bevel of the phaco tip in their direction (H) until all nuclear material is removed (I). |
To be specific, at our teaching program, the residents begin with the typical tactics for phacoemulsification. These include the divide-and-conquer, stop-and-chop, and the various pure chopping methods, along with a litany of ancillary manipulations including tricks for rotating the lens.
The problem is that many of these maneuvers don’t work particularly well against soft nuclei. Their amorphous, semi-solid bodies lack rigid cleavage planes, so they don’t chop or crack. Instruments placed to spin them, instead, may pass harmlessly through without exerting any torque. And so, because our usual tactics aren’t effective, removing these cataracts can be a surprisingly frustrating and difficult ordeal.
Recently, however, we stumbled upon a new way of tackling these cases that is safe, simple, and—in our hands—successful. It relies on neither nuclear cracking nor rotation and can be performed without any specialized or expensive equipment. We call the tactic the V-slice.
The operation begins per usual: following the paracentesis, the anterior chamber is filled with preservative free lidocaine and an ophthalmic viscosurgical device. The main wound is created with a 2.2-mm keratome, through which a normal diameter (5.5- to 6-mm) capsulorhexis is fashioned. A blunt tipped chopping instrument (we prefer the Goldberg Nucleus Manipulator [Ambler Surgical, Rhein Medical]) is brought through the main wound, over the nuclear face, underneath the anterior capsule, and around the lens equator at the 7-o’clock position (See Figure 1). Then, the chopper is slowly passed through the lens at approximately one-half to two-thirds depth, aiming for the 12-o’clock position, stopping immediately if any resistance is encountered. Thereafter, the chopper is moved to the 5-o’clock position and this process is repeated. The effect is to produce a central pie-shaped segment bounded laterally by two independent crescentic pieces. Gentle hydrodelineation followed by hydrodissection is then performed. (Alternatively, one can simply hydrodissect and eliminate the hydrodelineation step.). Next, OVD is injected into the sliced grooves to further define the pieces and to push the posterior capsule back. The phaco hand- piece can then be introduced through the main wound and a second instrument through the paracentesis (we like the Connor Wand [Ambler Surgical, Rhein Medical]). Typically, the central, pie-shaped piece is the easiest to remove first, since it is usually totally separated from its surroundings and floating at the level of the capsulorhexis.
After this, the two remaining crescentic pieces can be removed in similar fashion. Thereafter the operation concludes per routine: The irrigation/aspiration handpiece is used to complete cortical cleanup, the capsular bag is filled with OVD, the lens injected, the OVD removed, and the eye brought to a physiologic pressure with the wounds checked for leaks.
At our program, the advantages of this technique are: Rotation of the nucleus is not essential; it permits easy and reliable segmentation of the lens before hydrodissection when visualization is optimized; it doesn’t rely on “cracking” to achieve this segmentation; lens division may proceed “one-handed” (which may be especially helpful for beginning surgeons, who may find a bimanual chopping procedure more challenging); it mobilizes the lens within the capsular bag without depending on nuclear rotation (or requiring hydrodissection, which may be advantageous in eyes with posterior polar cataracts); and finally, these steps can be performed without the need for specialized instruments.
Over the years, this has become our primary strategy for soft cataract removal in our resident clinics. To our knowledge, no complications stemming from this technique have occurred, which is perhaps a testament to its inherent safety, considering that many of our surgeons are only just learning the basics of cataract surgery.
The primary downside of the V-slice is that it may be useful only in very soft cataracts, since the maneuver may place undue stress on the lens zonules if a dense nucleus is encountered. Careful patient selection is therefore required. But, so far, we have been encouraged by our results with this approach and we would like to invite other interested surgeons to give it a try. REVIEW
The authors are ophthalmology residents at the University of Alabama, Birmingham, Callahan Eye Hospital, Birmingham, Ala. They acknowledge the assistance of Jeffrey Yee, MS, MD; and Jack Parker, MD.
Contact Dr. Parker at jack.parker@gmail.com.
1. Fishkind WJ. Management of the soft nucleus. In Fishkind W.J. (eds): Complications in Phacoemulsification; Avoidance, Recognition, and Management. New York, NY: Thieme, 2002. pp. 105-111.