Given the patient’s clinical findings, she was diagnosed with ocular melanocytosis and recommended to have twice-yearly dilated fundoscopic examinations to monitor for the occurrence of melanoma. Over the next three years, examination findings remained stable. By 6 years of age, the IPE cysts had enlarged with iridocorneal touch and shallowing of the anterior chamber. Ultrasound biomicroscopy revealed numerous IPE cysts involving the pupillary margin, mid-zonal region and iridociliary sulcus junction as well as thickening of the ciliary body along the 6 and 9 o’clock meridians. The two largest cysts touching the endothelium were reduced using fine needle aspiration. Cytopathologic examination revealed cyst contents and no malignancy.
At this time, systemic evaluation revealed a normal echocardiogram to rule out aortic dissection that can be associated with pupillary margin IPE cysts, and normal brain and orbits MRI scan to rule out intracranial or meningeal involvement of the melanocytosis. The MRI did show a slightly smaller right globe with asymmetrical slight thickening and enhancement involving the ciliary body region OD, suspected to represent melanocytosis and consistent with the UBM findings. Observation was advised.
Two years later, the patient noted swelling and a mass-like lesion in the right temporal fossa. MRI revealed a soft-tissue mass in the right temporal fossa involving the temporalis muscle and measuring 3.5 x 1.4 x 2.7 cm. A suspicion for neoplasm was raised. Biopsy and histopathologic examination of this lesion revealed a diagnosis of malignant melanoma in the setting of a blue nevus. In addition, a mass was noted in the right eye by MRI.
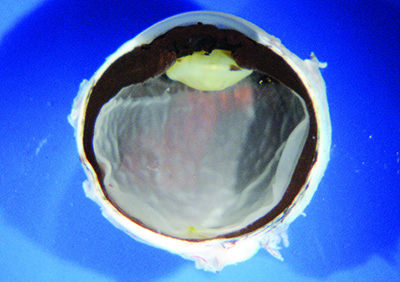
Ocular examination at this time showed large coalescent IPE cysts OD, precluding a view of the fundus. In-office B-scan ultrasonography disclosed a large choroidal mass, measuring 15 x 13 x 9.6 mm, and the entire uvea appeared thickened. Emergent MRI confirmed lack of orbital mass, but a clear-cut enhancing mass within the right globe, suggestive of a uveal malignant melanoma.
|
Discussion
Oculodermal melanocytosis is defined as a congenital pigmentation of the periocular skin, episclera, uveal tract, and sometimes the orbit, meninges and hard palate.1 Melanocytosis affects <1 percent of the Caucasian population, and it can be bilateral in 10 percent of cases.1 Clinically, this condition appears as a flat, gray dermal pigmentation along the distribution of the 1st and 2nd divisions of the trigeminal nerve, although hard palate and temporal skin involvement can occur. The sclera assumes a blue-gray discoloration and the iris and choroid appear dark brown, often with iris mamillations and occasionally with elevated intraocular pressure from angle pigmentation.2 Histopathologically, melanocytosis represents an excess of dendritic melanocytes in affected tissues, which can give rise to malignant melanoma, typically in the uvea, orbit or brain.3
The cutaneous component of oculodermal melanocytosis is a form of flat blue nevus. Blue nevus is generally categorized into congenital or acquired types and appears as a blue to black nodule within the dermis. There are two varieties of blue nevus: common and cellular. The common blue nevus has no potential for evolution into melanoma, while the cellular blue nevus carries low potential to undergo malignant transformation.4 Most cutaneous blue nevi appear thicker and more irregular than oculodermal melanocytosis.1
Management of patients with oculodermal melanocytosis entails periodic examination for early detection of malignant melanoma. Dilated fundoscopic examination should be performed every six months. Surgical removal of patches of cutaneous or scleral melanocytosis is generally not advised.1
The overall lifetime risk for development of uveal melanoma in an eye with ocular melanocytosis has been calculated at one in 400 for Caucasians.5 A study on sectoral melanocytosis by Carol Shields, MD, and colleagues revealed that male gender; related cutaneous or palatal melanocytosis, particularly in the temple region; scleral melanocytosis in the superior, nasal or temporal quadrants; sector or diffuse choroidal melanocytosis; and diffuse iris melanocytosis were associated with a clinically significant higher odds ratio for the presence or development of melanoma.6
Further analysis of this relationship disclosed that patients who develop melanoma in association with oculodermal melanocytosis carry a worse prognosis than those without melanocytosis. Melanoma in the setting of melanocytosis has approximately double the risk for metastasis.7 Increasing tumor thickness was found to be predictive of both metastasis and death.7 This was confirmed in a matched study that compared melanoma patients with oculodermal melanocytosis to those without this association. Even when cases were matched for patient age, tumor location, basal diameter and thickness, those with oculodermal melanocytosis still carried double the risk for metastasis.8 While the etiology of this difference is unknown, it could be due to a subtle cytologic or genetic difference between the tumors.
In conclusion, oculodermal melanocytosis is congenital pigmentation that predisposes the patient to a low risk for uveal melanoma. When realizing the relatively aggressive nature melanoma and understanding the importance of detection when the malignancy is small, we suggest that screening of all patients with melanocytosis twice yearly and imaging of the eye annually is the mainstay of management. REVIEW
1. Shields JA, Shields CL, eds. Eyelid, Conjunctival, and Orbital Tumors: An Atlas and Textbook. 2nd ed. Philadelphia: Lippincott Williams and Wilkins, 2008:100-8.
2. Teekhasaenee C, Ritch R, Rutnin U, et al. Glaucoma in oculodermal melanocytosis. Ophthalmology 1990;97:562-70.
3. Shields JA, Shields CL, eds. Intraocular Tumors: An Atlas and Textbook. 2nd ed. Philadelphia,: Lippincott Williams and Wilkins, 2008:6-7.
4. Eagle, RC. Eye Pathology: An Atlas and Text. 2nd ed. Philadelphia: Lippincott Williams and Wilkins, 2011:251.
5. Singh AD, De Potter P, Fijal B, et al. Lifetime prevalence of uveal melanoma in white patients with oculo(dermal) melanocytosis. Ophthalmology 1998;107:195-98.
6. Shields CL, Qureshi A, Mashayekhi A, et al. Sector (partial) oculo(dermal) melanocytosis in 89 eyes. Ophthalmology 2011;118:2474-2479.
7. Shields CL, Kaliki S, Livesey M, et al. Association of ocular and oculodermal melanocytosis with the rate of uveal melanoma metastasis: Analysis of 7,872 consecutive eyes. JAMA Ophthalmology 2013;131:993-1003.
8. Mashayekhi A, Kaliki S, Walker B, et al. Metastasis from uveal melanoma associated with congenital ocular melanocytosis: A matched study. Ophthalmology 2013;120:1465-1468.