Flap thicknesses and LASIK volume are two of the topics covered in this month’s refractive surgery survey. The survey e-mail was opened by 1,733 of 11,600 subscribers to Review’s electronic mail service (14.9-percent open rate), and 70 surgeons responded. See how their approaches to refractive surgery align with yours.
The Shrinking Flap
As mentioned earlier, surgeons are extolling the virtues of thin flaps, with 73 percent of them saying they prefer to make flaps that are between 100 and 119 µm thick, an increase from last year’s 59 percent. Sixteen percent prefer flaps to be 120 to 130 µm. Six percent employ flaps thicker than 150 µm, 4 percent use flaps less than 100 µm and 2 percent prefer flaps between 131 and 149 µm thick.
Sixty-eight percent of the surgeons use a femtosecond laser to create their flaps, with the rest preferring a blade.
As for why surgeons like the relatively thin flap size of 100 to 119 µm, many think it’s a good compromise between the extremes of thickness. Paul Kuck, MD, of LaCrosse, Wis., says this kind of flap works best for him. “A flap of 110 µm is safe enough to prevent tears and avoid too thin a flap if there is a variable cut,” he says. “I still may go thinner, though: I just upgraded to an Alcon FS200 femtosecond laser.”
 |
Preferred Procedures
Though it will take another a year or two more to declare it a trend, the percentage of surgeons who say they prefer to use wavefront-optimized LASIK for most of their cases increased to 33 percent from 13 percent on last year’s survey. A third say they prefer to use custom LASIK. Thirteen percent like PRK and 12 percent prefer conventional LASIK for most of their cases. Four percent do epi-LASIK on most patients, and 2 percent each say they mostly do CK, LASEK or Staar Visian implantation.
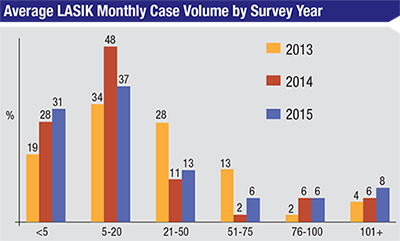
Monthly LASIK volumes reported on the survey remain somewhat flat, and hover around their 2014 levels (a comparison graph of the past three years appears below). Sixty-eight percent of surgeons say they perform 20 or fewer cases per month. Eight percent, however, say they do more than 100 cases per month, which is up slightly from last year’s 6 percent. The average price surgeons charge for LASIK increased compared to last year, climbing to $3,395 from $2,452. For PRK, surgeons charge an average of $3,389 this year, versus $2,404 last year.
Feelings on Phakics
Thirty-six percent of the surgeons say that phakic IOLs are an option they reach for in select patients, but this doesn’t mean these lenses don’t have shortcomings.
William Trattler, MD, of Miami gets good results with the Visian ICL. “I love the ICL,” he says. “But I wish it had a fenestration so we could eliminate the need to create a peripheral iridotomy.” A surgeon from Philadelphia agrees, and voices a gripe many phakic lens surgeons have, namely that toric phakic lenses have yet to be approved in the United States. “I use the ICL,” he says. “The benefits are that it uses a small incision and the eye is quick-healing. The drawbacks are difficult sizing, no astigmatism option and the need for YAG PIs.”
A surgeon from Oklahoma also bemoans the approval process that is keeping a toric option out of his reach. “I don’t like the slow approvals from the FDA,” he says. “We should have gotten approval for a toric phakic lens in the United States. We should also have gotten approval for a fenestrated lens to stop having to perform PIs. Also, these lenses should be preloaded.”
However, not everyone is a fan of phakic lenses, and some foresee problems down the road. A surgeon from Utah dislikes them as an option, saying, “The rate of debilitating glare and cataract formation are way under-reported. They all eventually have to be removed if the patient lives long enough and forms cataracts.”
Tough Cases
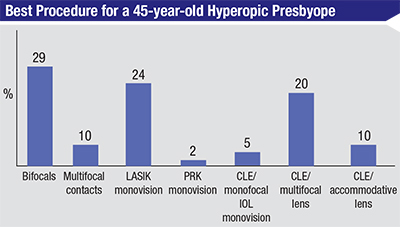
Surgeons say they alter their approach to certain patients, depending on the level of correction that’s needed and, sometimes, patient age.
For a high (-11 D) myope, most of the surgeons, 75 percent, say they think a phakic IOL is best. Kurt Andreason, MD, director of the Wright Patterson Air Force Base’s Warfighter Refractive Eye Surgery Center in Ohio, says a phakic intraocular lens is usually a good method because other ones fall short in such patients. “The residual stromal bed is usually insufficient for this refraction,” he says. “PRK with mitomycin-C is a consideration, but there is plenty of room for a phakic IOL in this situation, without much corneal effect.” A physician from Oklahoma says he’ll consider the patient’s age. “If the patient age is under 45, I’ll use an ICL,” he says. “If it’s over 45, I’ll use CLE/IOL implantation. I choose these options for quality of vision and ease of healing without regression.”
 |
Future Plans
Surgeons have also been keeping an eye on the refractive surgery pipeline, and have opinions about which burgeoning technology piques their interest the most. The most popular new technologies are corneal inlays/onlays (38 percent) and corneal cross-linking (22 percent). The other popular options were small-incision lenticule extraction (18 percent) and a new accommodative lens (18 percent).
Dr. Andreason is in the group that’s most looking forward to onlays. “This technology and its results seem promising,” he says. “LASIK surgeons can do it safely, it is reversible and many patients will be motivated to try it if long-term results continue to be successful.” George Walters, MD, of Port Arthur, Texas, feels similarly, saying, “This technology would benefit more patients and increase LASIK volume.”
Wisconsin’s Dr. Kuck is one of the 22 percent looking forward to the approval of corneal cross-linking. “It benefits keratoconus patients and decreases the risk of ectasia in patients with thin but ‘Pentacam-normal’ corneas,” he says. An ophthalmologist from California agrees, and says that she is eagerly awaiting cross-linking because of its versatility, saying, “Cross-linking has lots of applications.” REVIEW




