| ||||||||||
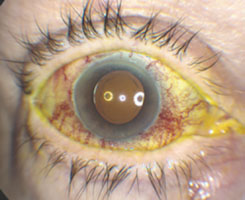
The combination of proptosis, central retinal vein occlusion, corkscrew episcleral vessels and elevated intraocular pressure raised concern for obstruction or arterialization of the orbital venous system, with carotid-cavernous sinus fistula being high on the differential diagnosis.
The patient’s records were obtained and reviewed. An MRI and MRA were performed during her recent hospitalization, which showed an apparent left enophthalmos with atrophy of the extraocular muscles, and was read as negative for mass, cavernous sinus thrombosis and arteriovenous malformation (AVM). The patient was subsequently referred to the Neuro-Ophthalmology Service at Wills Eye, where orbital Doppler imaging was performed. This showed non-arterialized reversal of flow in the right superior ophthalmic vein (SOV) and absence of flow in the right central retinal vein. Although she lacked the arterialized reversal of flow in the SOV reported in dural AVM, it was felt that she had entered the resolution phase, now at five months after her initial symptoms began.
She was seen by the Retina Service twice prior to her neuro-ophthalmology appointment, given intravitreal bevacizumab at each visit, and had notable improvement of the episcleral engorgement (See Figure 2a), retinal hemorrhages (See Figure 2b) and macular edema (See Figure 2c). Intraocular pressure declined to 12 mmHg in the right eye and vision improved to 20/60. Given her clinical improvement and following extensive discussion with the patient regarding the risks and benefits of conventional angiography, close observation with deferral of further imaging was elected.
Discussion
| |||||||||
CCF are classified as either direct (high flow) or indirect (low flow), with the latter arising from dural branches of the internal and external carotid arteries.8 High-flow CCF are most often caused by trauma and exhibit the classic pulsating exophthalmos with an orbital bruit. Conversely, low-flow CCF, also called dural arteriovenous malformations (DAVM), are postulated to occur via localized thrombotic events, with less dramatic presentation.8 Doppler ultrasound in DAVM classically shows arterialized reversal of flow in the SOV.9,10
DAVM most commonly present in females over 50 years old with hypertension, exhibiting exam findings of limbal vascular loops in 25 percent, venous stasis retinopathy via central retinal vein thrombosis in 15 percent and occasionally an orbital bruit.8 Magnetic resonance or CT angiography may be negative, with definitive diagnosis confirmed by super-selective conventional angiography. Angiography with endovascular treatment however, entails a 2 to 4 percent risk of stroke, vision loss, or other permanent neurologic morbidity.11,12 Many DAVM will spontaneously resolve, and the decision to pursue conventional angiography must weigh the risks and benefits of the procedure.
DAVM can cause significant ocular morbidity. The most serious complications are from intracerebral hemorrhage with resulting stroke, occurring in 3 percent of patients.13 These complications occur with deeper venous drainage of the fistula, and attempts have been made to clinically predict the patients who have such drainage patterns. Exam findings predictive of cortical venous drainage include bilateral orbital congestion, post-auricular bruit and CNS dysfunction.14
Indications for intervention in DAVM include progressive visual decline, ocular pain, glaucoma, ophthalmoplegia, proptosis and intracranial bleeding.8 Our patient did not have an indication for intervention, and was showing clinical improvement. After extensive discussion, a plan of close observation was agreed upon. Should she fail to improve further or develop an indication for intervention, treatment options include surgery, trans-arterial or trans-venous embolization and radiosurgery, with the latter two having reported success rates of 90 percent and significantly less morbidity than surgery.12,15 REVIEW
The author would like to thank John Pitcher, MD, of the Retina Service and Jennifer Hall, MD, and Mark Moster, MD, of the Neuro-Ophthalmology Service at Wills Eye Institute.
1. Sainz de la Maza M, Molina N, Gonzalez-Gonzalez LA, et al. Clinical characteristics of a large cohort of patients with scleritis and episcleritis. Ophthalmology 2012;119:43-50.
2. Hayreh SS, Zimmerman B, McCarthy MJ, Podhajsky P. Systemic diseases associated with various types of retinal vein occlusion. Am J Ophthalmol 2001;131:61-77.
3. Wang M, Khurana RN, Sadda SR. Central retinal vein occlusion in Wegener’s granulomatosis without retinal vasculitis. Br. J. Ophthalmol 2006;90(11):1435-6.
4. Rosenthal G, Schneck M, Lifshitz T. Branch retinal vein occlusion in Churg-Strauss syndrome. Clin Exp Ophthalmol 2002;30:381-2.
5. Chen SD, Lochhead J, Satchi K, et al. Bilateral retinal venous occlusion and unilateral cystoid macular edema in Churg-Strauss syndrome treated with intravitreal triamcinolone. Retina 2005;25:655-7.
7. Dave PV, Mathai A, Gupta A. Combined anterior and posterior scleritis associated with central retinal vein occlusion: A case report. J Ophthal Inflamm Infect 2012;2:165-8.
8. Feiner L, Bennett J, Volpe NJ. Cavernous sinus fistulas: Carotid cavernous fistulas and dural arteriovenous malformations. Current Neurol and Neurosci Reports 2003;3:415-20.
9. Kawaguchi S, Sakaki T, Uranishi R. Color doppler flow imaging of the superior ophthalmic vein in dural arteriovenous fistulas. Stroke 2002;33:2009-13.
10. Flaharty PM, Lieb WE, Sergott RC, Bosley TM, Savino PJ. Color Doppler imaging. A new noninvasive technique to diagnose and monitor carotid cavernous sinus fistulas. Arch Ophthalmol 1991;109:522-6.
11. Liu HM, Wang YH, Chen YF, et al. Long-term clinical outcome of spontaneous carotid cavernous sinus fistulae supplied by dural branches of the internal carotid artery. Neuroradiology 2001;43:1007-14.
12. Meyers PM, Halbach VV, Dowd CF, et al. Dural carotid cavernous fistula: Definitive endovascular management and long-term follow-up. Am J Ophthalmol 2002;134:85-92.
13. Stiebel-Kalish H, Setton A, Nimii Y, et al. Cavernous sinus dural arteriovenous malformations. Patterns of venous drainage are related to clinical signs and symptoms. Ophthalmology 2002;109:1685-91
14. Stiebel-Kalish H, Setton A, Berenstein A, et al. Bilateral orbital signs predict cortical venous drainage in cavernous sinus dural AVMs. Neurology 2002;58:1521-4.
15. Barcia-Salorio J, Soler F, Barcia J, Hernandez G. Sterotactic radiosurgery for the treatment of low-flow carotid-cavernous fistulae: Results in a series of 25 cases. Stereotactic Functional Neurosurg 1994;63:266-70.