Diagnosis, Workup and Treatment
|
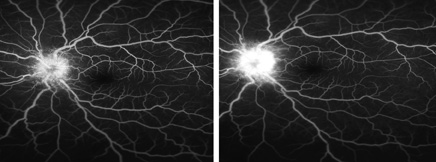
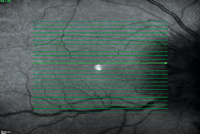
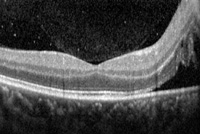
In the interim the patient underwent an intravenous fluorescein angiography, which confirmed optic disc edema; however, it did not reveal significant vasculitis (See Figure 2). An optical coherence tomography of both optic nerves was obtained, which showed edema localized to both optic discs and nasal macula, sparing the fovea (See Figure 3).
| ||||
Discussion
Syphilis is a bacterial infection caused by the spirochete, Treponema pallidum, which is primarily sexually transmitted, but may be vertically transmitted, leading to congenital syphilis. The incidence of syphilis in the United States has been on the rise for the past decade. An August 2011 report, funded by the Centers for Disease Control and Prevention, identified young black men who have sex with men as the demographic group disproportionately affected by the rising incidence of syphilis. Mirroring this trend is the rising incidence of HIV infection over the past 10 years in the same demographic, as the two infections are often seen in tandem.
Syphilis is typically characterized as presenting in one of four different stages: primary; secondary; latent; or tertiary. This conventional staging system contributes very little towards the understanding and classification of ocular syphilis. Ocular syphilis is by definition neurosyphilis, and it can occur in any of the four stages. Neurosyphilis seen in the tertiary phase refers to the general paresis, tabes dorsalis, and meningitis or meningiovascular complications that can be seen with prolonged untreated infection. Ocular syphilis is considered to be the most common form of neurosyphilis encountered. Syphilis, often referred to as the “great imitator,” can have innumerable manifestations throughout the body. The more common presentations of ocular syphilis include interstitial keratitis; anterior, intermediate and posterior uveitis; chorioretinitis; retinitis; retinal vasculitis; and cranial neuritis, including optic neuritis. This wide variability warrants a consideration of syphilis for many ophthalmic pathologies, particularly in the demographic groups most at risk.
A diagnosis of syphilis is confirmed by serology or dark field microscopy of tissue; however, in clinical practice the latter is rarely used. The initial screening tests with high sensitivity are the nontreponemal serologies that include VDRL and RPR tests. The more specific confirmatory test uses treponemal serologies, including FTA-Abs and Treponemal pallidum particle agglutination (TPHA) tests. Given the high co-infection rate with HIV, standard of care should include HIV serologies when considering a new diagnosis of syphilis. In a 2011 systematic review of the literature, Joseph D. Tucker, MD, and colleagues found that in 101 cases of ocular syphilis and HIV, ocular syphilis led to the diagnosis of HIV in 62 percent of the cases.
Lumbar puncture is not routine in the diagnostic workup for all stages of syphilis; however, it is indicated in the setting of neurosyphilis, patients with concerning neurologic findings in the setting of positive serologies, co-infection with HIV, and any patient with serological evidence of treatment failure despite standard-of-care treatment. Posterior segment manifestations of ocular syphilis often warrant further diagnostic testing including OCT and IVFA to further classify posterior syphilitic involvement as well as to evaluate response to treatment.
Treatment of ocular syphilis is the same as the treatment for neurosyphilis. The CDC recommends two regimens dictated by patient reliability. The standard regimen is IV penicillin G given for 10 to 14 days. A highly compliant patient may also be treated with daily intramuscular procaine penicillin and oral probenecid four times a day for 10 to 14 days.
The rising incidence of ocular syphilis and co-infection with HIV exists in contrast to the declining incidence of other HIV-related infections in the post-HAART era, particularly CMV-retinitis. This has prompted recent studies and literature reviews to investigate differences in presentation, clinical course and overall outcome in these patients. Dr. Tucker’s group found that posterior segment manifestations were the most common initial presentation in the HIV-positive group with ocular syphilis, particularly posterior uveitis and optic neuritis. The group also found a statistically significant association between the increased incidence of posterior uveitis and a CD4 count of less than 200. Both Dr. Tucker’s group and David J. Browning MD, PhD, and colleagues did not find that HIV negatively affected response to treatment for neurosyphilis; however, there have been reports of delay in resolution of symptoms for up to a year in HIV-positive cohorts.
CSF analysis may show pleocytosis as well as higher VDRL reactivity in the HIV-infected patient versus the non-HIV-infected patient. Post-treatment surveillance lumbar punctures are indicated when highly abnormal parameters are initially present in the CSF. HIV infection can slow the resolution of these parameters. Current CDC recommendations in the HIV-positive population dictate a consideration of retreatment if the CSF cell count has not decreased six months after initiating treatment, or if the CSF continues to show abnormalities two years after initiation of treatment.
The author would like to thank James Vander, MD, of the Wills Eye Retina Service for his assistance with this case.
1. Browning, DJ. Posterior segment manifestations of active ocular syphilis, their response to a neurosyphilis regimen of penicillin therapy and the incidence of human immunodeficiency virus status on response. Ophthalmol 2000;107:2015-2023.
2. Centers for Disease Control and Prevention. “Sexually Transmitted Diseases Treatment Guideline, 2010.” Centers for Disease Control and Prevention Sexually Transmitted Diseases. Centers for Disease Control and Prevention. Web. 28 January 2011< http://www.cdc.gov/std/treatment/2010/genital-ulcers.htm#neuro.>
3. Danesh-Meyer H, Kubis KC, Sergott RC. Not so slowly progressive visual loss. Surv Ophthalmol 1999;44:247-252.
4. Ghanem KG, Moore RD, Rompalo AM. Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS 2008;22:1145-51.
5. Gonzalez-Lopez JJ, Fernandez Guerrero ML, Lujan R, et al. Factors determining serologic response to treatment in patients with syphilis. Clin Infec Dis 2009;49:1505-1511.
6. Katz DA, Berger JR, Duncan RC. Neurosyphilis: A comparative study of the effect of infection with human immunodeficiency virus. Arch Neurol 1993;50:243-9.
7. Kiss S, Damico FM,Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol 2005;20:161-7.
8. Lukehart SA, Hook EW 3rd, Baker-Zander SA, et al. Invasion of the central nervous system by treponema pallidum: Implications for diagnosis and treatment. Ann Intern Med 1988;109:855-62.
9. Musher DM, Hamill RJ, Baughn RE. Effect of human immunodeficiency virus (HIV) infection on the course of syphilis and on the response to treatment. Ann Intern Med 1990:113:872-81.
10. Su JR, Beltrami JF, Zaidi AA, et al. Primary and secondary syphilis among black and Hispanic men who have sex with men: Case report data from 27 states. Ann Intern Med 2011;155:145-51.
11. Tucker JD, Li JZ, Robbins GK et al. Ocular syphilis among HIV-infected patients: A systematic analysis of the literature. Sex Transm Infect 2011;87:4-8.