 |
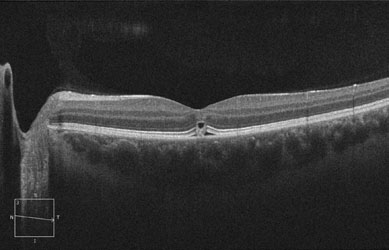
| Figure 2. Spectral-domain OCT imaging of left eye demonstrating disruption of IS/OS junction with a focal area of subfoveal edema. |
In most situations involving laser pointer eye injuries, there is little diagnostic dilemma. As in the case presented here, patients are able to identify the sentinel event of laser exposure followed by some transient afterimage, scotoma or other visual disturbance.
Appropriate workup consists of a full ophthalmologic exam, including fundus photography and optical coherence tomography of any abnormalities to document the baseline appearance and extent of the lesion. Amsler grid testing can be helpful to identify the location of the visual disturbance as well as to document its evolution. Our patient had imaging with spectral-domain OCT, which showed a discrete foveal abnormality involving all layers of the retina, but most prominently the outer retinal layers (See Figure 2). There was distinct disruption of the inner segment/outer segment (IS/OS) junction, which seemed to be replaced by a small outer retinal cyst. Also present was a small amount of sub-retinal fluid.
Treatment for retinal laser injuries is controversial and limited. Current medical therapy consists of systemic corticosteroids, which has shown mixed results.1 There are also anecdotal reports describing the use of antioxidants and other vitamins. Observation is also a reasonable option as many of these patients will experience improvement of visual acuity and visual symptoms with time. The decision was made to observe the patient presented here as opposed to instituting any type of treatment.
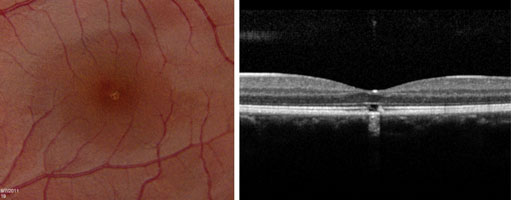 |
| Figure 3. Fundus photograph of the left eye two weeks after laser injury, left. OCT imaging of left eye two weeks after laser injury, right. |
Discussion
As the use of laser pointers becomes more popular, it is important for physicians to know which lasers have the potential for causing eye injury. Lasers are divided into four “classes” based on their strength of output. Class 1 lasers, with a maximum output that is <0.4 mW, are considered the safest lasers and are believed incapable of causing damage even if viewed for long periods of time.3 Class 2 lasers have a maximum output <1 mW. These are also felt to be extremely unlikely to result in ocular injury because of protective mechanisms conferred by the body’s natural blink response and aversion reflexes.4 Class 3A lasers have a maximum output between 1 mW and 5 mW, and although they cannot cause immediate eye injury, they can induce damage if stared directly at for sustained periods of time.3 Most laser pointers that are available in the United States are class 2 or class 3A lasers.3
Class 3B lasers are much more powerful, with a maximum output between 5 mW and 500 mW. These are believed to be capable of producing ocular damage immediately upon viewing.3 Although these lasers are illegal in some countries, they can be obtained quite easily via the Internet. Class 4 lasers are the most powerful lasers, boasting a maximal output >500 mW. These are typically used in military and occupational settings, such as laser shows. They are capable of producing extensive ocular damage.5 Given the brevity of our patient’s exposure that still resulted in retinal injury, the laser involved was most likely a class 3B laser.
Another important consideration in laser pointer injuries is the color of the laser. When laser pointers first became commercially available, they were virtually all red lasers with a wavelength of 670 nm. Recently, green laser pointers with a wavelength of 532 nm have become more popular because of several advantages they confer over red lasers. The beam of green laser pointers is much more visible in ordinary night atmospheres and is also visible in daylight. However, the retina is more sensitive to shorter wavelengths.6
To illustrate this, a study group from the Mayo Clinic performed separate studies where they exposed the healthy retina of eyes destined for enucleation due to choroidal melanoma to both a red class 3A laser pointer and a green class 3A laser pointer.6,7 When the red laser was used, they were unable to document any abnormalities in clinical appearance, fluorescein angiography or histopathologic examination. In contrast, exposure to the green laser pointer resulted in changes seen clinically, with OCT imaging and on histopathologic examination. This suggests that green laser pointers carry a higher risk of causing retinal injury than red laser pointers.
Multiple symptoms have been reported in patients with laser pointer exposures, such as eye pain, redness, irritation, corneal signs and retinal injury. It is important for physicians to know which of these symptoms could actually be caused by such exposure. Red, irritated eyes as well as eye pain are common complaints of those exposed to laser pointers; however, none of these things can be caused directly from laser pointer exposure. The laser light that hits the retina has been amplified by the refractive media of the eye to produce a retinal irradiance (watts per unit area) 104 times greater than the irradiance present at the cornea.1 The energy present at the ocular surface and the external ocular structures is not sufficient to cause any appreciable effect. It is the amplification of irradiance by the ocular media that makes the retina the most susceptible body tissue to laser pointer injury. Any redness or surface irritation in a patient with laser pointer exposure is likely due to secondary rubbing of the eye. Also, since the retina lacks pain receptors, eye pain is an unlikely symptom directly caused by laser pointer exposure.
A number of factors play a role in determining the type and severity of retinal injury from laser pointers. Three of the most important factors are: 1) the amount of energy delivered by the laser; 2) the duration of exposure to the laser; and 3) the location of retinal involvement.1
Eye-threatening laser injuries used to be almost exclusively limited to military and occupational settings where the lasers were powerful enough to induce retinal injury. However, with more powerful laser pointers becoming commercially available to the public in recent years, laser eye injuries have become more common. Even minimal exposure can result in immediate and clinically significant retinal injury, particularly in the case of green laser pointers.
Case reports in the literature illustrate some important points regarding laser pointer injuries. Most patients exposed to lasers present with a transient afterimage that usually resolves. Some patients, as in this case, present with a mild visual disturbance, such as a fixed scotoma or subtle decline in visual acuity. However, there have also been cases reported of precipitous decline in visual acuity due to subretinal hemorrhage or subinternal limiting membrane hemorrhage.5,8 There are also reports of long-term complications due to laser pointers such as choroidal neovascularization.9
Although many patients recover full visual function within several weeks following the injury, several late complications have been reported. The most common complication is chorioretinal scarring.1 Other complications include macular hole, macular cyst and epiretinal membrane formation.1 As patients are also at risk for development of CNV after retina laser injury, they should be monitored for this. Any change in vision or development of retinal hemorrhage and/or edema following initial resolution of the injury should be promptly evaluated for possible CNV. The evaluation should include clinical examination, OCT and fluorescein angiography. In addition, patients can be given an Amsler grid for self-testing and should be told to follow-up for any metamorphopsic changes.
The author would like to thank Nikolas London, MD, of the Wills Eye Institute Retina Department, for his time and assistance.
1. Barkana Y, Belkin M. Laser eye injuries. Surv Ophthalmol 2000;44:459-78.
2. Sethi CS, Grey RHB, Dean Hart C. Laser pointers revisited: Asurvey of 14 patients attending casualty at the Bristol Eye Hospital. Br J Ophthalmol 1999;83:1164-7.
3. Marshall J. The safety of laser pointers: Myths and realities. Br J Ophthalmol. 1998;82:1335-8.
4. Ajudua S, Mello MJ. Shedding some light on laser pointer eye injuries. Pediatr Emerg Care 2007;23:669-72.
5. Boosten K, Van Ginderdeuren R, Spileers W, et al. Laser-induced retinal injury following a recreational laser show: Two case reports and a clinicopathological study. Bull. Soc. Belge Ophtalmol. 2011;317:1-16.
6. Robertson DM, McLaren JW, Salomao DR, Link TP. Retinopathy from a green laser pointer: A clinicopathologic study. Arch Ophthalmol 2005;123:629-33.
7. Robertson DM, Lim TH, Salomao DR, et al. Laser pointers and the human eye: A clinicopathologic study. Arch Ophthalmol 2000;118:1686-91.
8. Wyrsch S, Baenninger PB, Schmid MK. Retinal injuries from a handheld laser pointer. N Engl J Med 2010;363:1089-91.
9. Fujinami K, Yokoi T, Hiraoka M, et al. Choroidal neovascularization in a child following laser pointer-induced macular injury. Jpn J Ophthalmol 2010;54:631-3.



