A In terms of the national published Fee Schedule for physicians, after the mandated 0.5-percent MACRA increase and some of the other budget-neutrality and misvalued-code adjustments, the 2018 conversion factor went up 0.28 percent to $35.9996. Ambulatory surgical centers got a fee-schedule conversion factor increase of 1.9 percent to $45.575 if they meet quality-reporting requirements. HOPD services in eye care showed an overall +1.35-percent change.
Q In terms of payment changes, how did eye care fare for 2018?
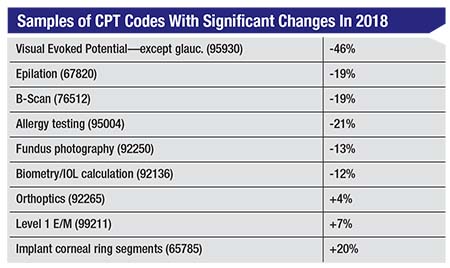
A Of the 622 possible codes that might apply to ophthalmologists and optometrists in 2018, only 42 have a reimbursement change of more than 3
 |
Q Are there any changes to Category I CPT codes for 2018?
A Oculoplastics is the area with the most changes (related to face and head flaps and nasal sinus endoscopy coding). In this area, most important, perhaps, is that CPT code 15732 (Muscle, myocutaneous or facsiocutaneous flap; head and neck [e.g., temporalis, masseter muscle, sternocleidomastoid, levator scapulae]) is deleted. This was sometimes used with SOOF lifts so other codes apply now (usually 1404x and 1406x).
Other codes with changes are:
• 15730—Midface flap (i.e., zygomaticofacial flap) with preservation of vascular pedicle;
• 15733—Muscle, myocutaneous or facsiocutaneous flap; head and neck with named vascular pedicle (e.g., buccinators, genioglossus, temporalis, masseter, sternocleidomastoid, levator scapulae); and
• 95930—Visual evoked potential (VEP) checkerboard or flash testing, central nervous system except glaucoma,
o With VEP for glaucoma (all types), code 0464T (Visual evoked potential testing for glaucoma, with interpretation and report) has applied since January 2017.
Q Are there any new CPT Category III codes?
A Category III codes are released twice a year. Coverage and payment for these codes are at the discretion of the individual Medicare Administrative Contractors. None are significant for eye care on January 1, 2018, but those that are in place and effective since July 1, 2017 are:
• 0469T—Retinal polarization scan, ocular screening with on-site automated results, bilateral;
• 0472T—Device evaluation, interrogation and initial programming of intraocular retinal electrode array (e.g., retinal prosthesis), in person, with iterative adjustment of the implantable device to test functionality, select optimal permanent programmed values with analysis, including visual training, with review and report by a qualified health care professional;
• 0473T—Device evaluation and interrogation of intraocular retinal electrode array (e.g., retinal prosthesis), in person, including reprogramming and visual training, when performed, with review and report by a qualified health care professional; and
• 0474T—Insertion of anterior segment aqueous drainage device, with creation of intraocular reservoir, internal approach, into the supraciliary space. (This is the code for the CyPass Micro-Stent.)
Q Are there HCPCS code changes to be aware of?
A For Medicare, the existing code for Omidria, C9447 (phenylephrine and ketorolac, injection) had its pass-through payment status changed. The payment indicator for this code changed from “K2” (paid separately) to “N1” (bundled). This means that on January 1, 2018, payment for C9447 is packaged in the reimbursement for the cataract procedure and is no longer separately identifiable for Part B Medicare.
An Advance Beneficiary Notice or similar financial waiver form cannot be used to shift the payment responsibility to the Medicare beneficiary.
Q Are there new things to be aware of from the Office of the Inspector General?
A The OIG no longer publishes an annual Work Plan as a separate document. It now does monthly updates on its website. Issues such as misuse of modifiers (e.g., 24, 25, and 59) continue to draw scrutiny. Oversight related to the new Quality Payment Program continues.
Q Has Medicare made changes of significance to beneficiaries?
A The 2018 Medicare Part B deductible remains the same as it was: $183. The standard monthly premium also remains unchanged at $134.
Q Are there changes to the Quality Payment Program that was new only last year?
A 2018 is the second year of QPP and there are some changes. Avoiding a Merit-based Incentive Payment reduction remains straightforward but the threshold is raised from three points in 2017 to 15 points in 2018. The maximum bonus or penalty rises to 5 percent from the current 4 percent. The Exceptional Performance threshold stays at 70 points. The exemptions for MIPS are raised to $90,000 in allowed charges or 200 Part B patients.
There were also changes to the relative weights and thresholds within the four MIPS components. In 2018, quality contributes 50 percent (down from 60 percent); advancing care information, 25 percent; clinical practice improvement activities, 15 percent; and resource use (Cost), 10 percent (up from zero). The “threshold of patient” percentage for quality in each of the six measures rises from 50 percent to 60 percent.
Q Were there changes to ICD-10?
A As with ICD-9, these go into effect on October 1 each year. There are a few subtle changes, but the biggest relate to myopic degeneration (H44.2-) and low vision/blindness coding (H54.-), each of which gained much greater specificity. REVIEW
Mr. Larson is a senior consultant at the Corcoran Consulting Group. Contact him at plarson@corcoranccg.com.




