This year's ARVO offerings in the realm of contact lenses share a better understanding of the corneal changes induced by corneal refractive therapy and further elucidate the effect of care solutions on the cornea and the lenses themselves. Study continues on comfort and compatibility of silicone hydrogels, and on the changes in tear film vis-à-vis contact lens wear. The 2004 papers offer good guidance for the contact lens practitioner, especially in difficult cases, but don't represent any dramatic breakthroughs in new products or clinical usage.
Tear Film
In healthy people, the functional behavior of the tear film should not be affected by contact lens wear, say researchers in Glasgow. Nineteen pathology-free subjects (mean age 31.5 years) wore biweekly disposable lenses in a daily-wear modality. After three months of wear, tear stability, evaporation and production rate showed no change from that seen initially. The one exception was tear composition, where significant increases in tear protein production levels were observed with adaptation to lens wear.1579
Study at the Schepens Eye Research Institute in Boston showed that neither the mucin RNA in the epithelium nor the free mucin proteins in the tears are altered by long-term contact lens wear. Researchers compared the tear fluid of 20 long-term (longer than five years), tolerant CL wearers with that of 20 non-CL wearers. No significant change was detected for any of the mucins (MUC1, 4, 5AC, and 16) when analyzing the expression of mRNA from CL and non-CL wearers. This indicates that in normal, healthy individuals without some pre-existing dry eye or other morphological change to the eye, contact lens wear appears to be fairly well-tolerated by the tear film.1567
 |
| Typical fluorescein picture of corneal staining observed with the ReNu care solution—Group II lens combination. |
A Japanese paper shows in a measurable way what contact lens practitioners have intuitively known for years: Wind has a deleterious effect on the tear film and consequently, contact lens wear. Researchers exposed the right eye of daily soft contact lens wearers (mean age 21.5 ±2) to wind artificially produced by an electric fan. Velocities of artificial wind were set at 0 m/s, 0.50 m/s, 1 m/s and 5.5 m/s under standardized conditions: air temperature 25 degrees C, relative humidity at 40 percent. Tear volume, tear interference patterns and non-invasive tear film breakup time were assessed. Subjects rated eye dryness before and during contact lens wear. For these contact lens wearers, wind over the open eye resulted in thinner lenses, more unstable vision and increased dryness. The tear film did not increase enough to compensate for the airflow. While other research shows that normal contact lens wear does not affect the tear film to any great extent, this study shows that the mechanical influences do exist.1559
Corneal Refractive Therapy
Studies presented this year on corneal refractive therapy focused again on safety and efficacy issues, but expanded as well into examination of CRT lens design and involvement of higher-order aberrations.
Even one hour of orthokeratology lens wear produces a measurable response on the cornea of young adults, say Australian researchers. Subjects wore reverse geometry lenses under open-eye conditions for one hour in one eye only. They were divided into two groups by age: Group I with a mean age of 24.3 and Group II at 43.9 years. Statistically significant changes from baseline were found in both subject groups for unaided visual acuity, corneal asphericity, apical corneal radius and central corneal and epithelial thickness. Of note, the older lens wearers (Group II) showed a reduced or delayed response to ortho-k lens wear. This research indicates that a one-hour open-eye test might be a good in-office screen for patient response to and toleration of reverse geometry lenses.1546
 |
| Research into corneal refractive therapy continues to grow. This year's ARVO papers examined the question of higher-order aberrations and CRT. Others measured the impact of varying treatment zone diameter on increased therapeutic effect. |
CRT research from Canada implies that patients should have residual acuity for up to 72 hours following cessation of lens wear. Twenty-three patients wore CRT lenses overnight for one month and did show a significant topographic shift over the wear period. The mean change in curvature measured immediately after lens removal on day 1 was -1.54 D centrally and 2.31 D at 3 mm temporal from the center. On day 28, the mean change in central curvature was -2.76 D and 4.08 D at 3 mm temporal from the center. On day 28, 14 hours after removal, little regression was noted compared to the morning measurement, with 18 percent regression centrally and 29 percent peripherally. At the 72-hour post-discontinuation visit, the cornea had not yet recovered to baseline, indicating that a change in shape can be maintained. Clinicians can share this good news with patients who may unintentionally miss an occasional night of CRT wear.1580
| HOAs and Ortho-K |
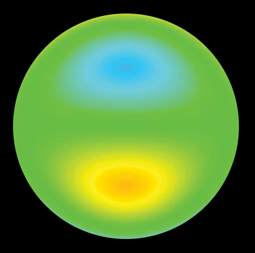 |
| Japanese researchers found that coma-like (represented above) and spherical-like aberrations increase significantly in patients undergoing overnight ortho-k.1548 |
CRT may induce or exacerbate higher-order aberrations. Sixty-four eyes of 39 Japanese patients undergoing overnight ortho-k were evaluated for induction of HOAs. Mean age of the subjects was 15.6 years. Mean spherical equivalent before treatment was -2.6 D. Researchers found that coma-like aberration and spherical-like aberration significantly increased in 3-mm, 4-mm and 6-mm pupils. These increases correlated positively with the amount of myopic correction.1548
Research out of Ohio State University supports the thesis that when trying to correct myopia Ž -2.5 D, increased aberration should be expected. In this study, 16 myopic subjects (mean: -2.72 D) wore CRT lenses for one month. While the mean sphere component of the refractive error decreased from -2.72 D to +0.55 D (an average change of +3.27 D), the total higher-order root mean square error increased from 0.1484 to 0.3173 µm (an average increase of 0.1689). Spherical-like aberrations increased from 0.0768 to 0.2277 µm. Coma-like aberrations increased from 0.1252 µm to 0.2110 µm. Clinicians would do well to advise patients that the greater the attempted increase in correction, the greater the potential for aberrations, e.g. ghosting of images, halos at night and loss of some high and low contrast sensitivity.1543
Care Systems
As in last year's abstracts, several 2004 papers weigh in on the question of cytotoxicity of contact lens multipurpose solutions containing polyhexamethylene biguanide (PHMB). The research has become more specific, looking at both levels of PHMB and at the other components of the MPS that contain it. The clinician might keep MPS in mind for a patient who is not comfortable after a period of adaptation with silicone hydrogels.
In an Alcon-sponsored clinical trial, adapted lens wearers wore conventional hydrogel (Group II or Group IV) or silicone hydrogel lenses that had been presoaked in one of four commercially available multipurpose solutions. Results showed that patients wearing Group II conventional hydrogel or Group I silicone hydrogel lenses could have corneal staining within even a few hours after insertion with a PHMB-based system. It is important to note, however, that while levels of staining were clinically significant, few associated subjective symptoms were reported by study subjects. For patients who do complain of contact lens sensitivity, a substitution of care solution might be a simple first step before swapping of lenses is considered.1538
A paper by Houston researchers attempts to get beyond corneal staining and look at actual epithelial cells to determine any toxicity from MPS. Eight healthy subjects were selected to receive one drop t.i.d. of one of two multipurpose solutions (labeled MPS-A and MPS-B). MPS-A contained polydronium hydrochloride. MPS-B contained poloxamine. Using a ConfoScan3 confocal microscope, neither MPS-A or MPS-B showed evidence of acute increase in corneal exfoliation or damage when compared to the saline control.1533
A study from CIBA Vision examined the dehydration rate of hydrogel contact lenses in order to determine the effect of care solutions on this rate. Lens dehydration is connected both to patient comfort and stability of vision. In this study, the dehydration rate was more dependent on the type of lens material than it was on the contact lens solution used. Researchers tested five commercially available contact lenses from Groups I and IV with three commercially available MPS, one investigational solution (CIBA's AQuify) and saline as a control. AQuify had steady state equilibrium water content levels that were 50-percent higher than the other lens care products, indicating that new solutions may be on the horizon that may be of help to the dry-eye contact lens patient.1545
Another CIBA Vision study suggests that cytotoxicity may be relative to the absolute concentration of PHMB in an MPS. Investigators used colorimetric assays to determine the quantitative factor-induced cytotoxicity within a 24- to 72-hour period of cell culture. They tested soft contact lens products with PHMB, the corresponding excipient solutions, and PHMB diluted by phosphate-buffered saline (PBS). Results revealed that only PHMB at 10 ppm was cytotoxic. Since PHMB of marketed contact lens solutions is approximately 1 ppm, this study suggests that other components of the solutions and/or the way PHMB reacts with these other parts may be responsible for cell damage.1534
Silicone Hydrogel Lenses
The availability of a choice of silicone hydrogel lens material becomes important to the clinician who tries to satisfy a preservative-sensitive patient. A CIBA Vision-sponsored study actually looked at the uptake of PHMB by two types of commercial silicone hydrogel soft contact lenses. Focus Night & Day (CIBA Vision) and PureVision (Bausch & Lomb) lenses were soaked in PHMB-preserved solutions for one or seven days, followed by measurement of the lenses' PHMB uptake. Regardless of soak time or type of solution, PureVision lenses took up more PHMB than the CIBA Vision lens. Also of note, this research showed that, while all of the tested care solutions contained
1 ppm PHMB, uptake of the preservative by the lenses was not equal. Just as not all silicone hydrogel lenses are alike, neither are the care solutions.1573
 |
| CIBA Vision's Focus Night & Day lens continues to be the subject of ARVO research. Investigators have advanced their study beyond that of silicone hydrogel lenses themselves to their interaction with care solutions, lubricants and the tear film. |
The more viscous contact lens lubricants (those containing cellulose acetate butyrate) best reduce symptoms of dryness in silicone hydrogel lens wearers, say Australian investigators. On four different days 15 subjects randomly instilled two drops of one of two commercially available viscous solutions, saline solution or used no solution at all. They rated comfort at pre-lens insertion, immediately after lens insertion and post-six hours lens wear. At six hours, silicone hydrogel wearers rated their lenses as less dry with the use of the more viscous lubricants compared to saline use. Similar results have been found in tests of viscous lubricants on conventional hydrogel lenses, but in those lenses even saline had a lubricating effect. Presumably the saline restores the water content of the conventional lenses (increasing comfort), whereas rehydration is not a factor in silicone hydrogels.1551
Dr. Key is in private practice in Houston, and serves as clinical professor of ophthalmology at Baylor College of Medicine.




