Every cataract surgeon recognizes that, like death and taxes, the occurrence of a retained nuclear chip is an unwelcome but essentially inevitable outcome at some point in time. Although this complication is not new, its incidence may be on the rise, according to some who speculate that the increase may be related to newer phacoemulsification settings that cause more turbulence within the anterior chamber. Thomas M. Harvey, MD, of Chippewa Valley Eye Clinic in Eau Claire, Wis., points out that, “The advent of newer phacoemulsification machines with settings that use a different trajectory of the phaco needle, such as a torsional or transitional movement, may be related to an increased incidence of retained nuclear chips.” He is quick to add that the literature does not support this association, and stresses that while there may be more anecdotal discourse on the topic, the incidence is still generally reported at one to two instances per 1,000 cases.
A retained nuclear chip typically presents asymptomatically one day postoperatively or at some point during the first month, possibly with signs such as corneal edema and elevated intraocular pressure, according to Dr. Harvey. “Therein lies the clinician’s dilemma,” says Dr. Harvey, “Should I observe this and perhaps treat it with topical steroidal eye drops—which has its own set of problems; should I blast it with a laser so that it can break it into smaller pieces that can be absorbed quickly through the eye’s natural digestive properties—an uncommon and unpopular choice; or should I schedule a second trip to the operating room to remove the fragment—which is something we all want to avoid at all cost?”
Prevalence
Not everyone supports the theory that newer phaco settings equate to a greater potential for retained nuclear fragments. Sherman W. Reeves, MD, MPH, of Minnesota Eye Consultants in Minneapolis, says he doesn’t think there is any connection. “Torsional phaco motions are basically microscopic. I don’t think this movement can be blamed for slinging lens fragments in different directions,” he says. Simply put, he points out, “Sometimes you miss a little chip, and it stays in the eye. It’s usually a nuclear fragment as opposed to a cortical fragment because cortical fragments have a tendency to dissolve much more quickly, whereas a nuclear fragment will stay around much longer and can cause inflammation in the eye if it is left behind.”
On the other hand, David A. Goldman, MD, of Bascom Palmer Eye Institute, in Miami, believes there is a direct connection. “I have heard plenty of anecdotal observations from fellow surgeons supporting this, and we are in agreement that when you get retained nuclear material specifically under the incision it is related to the newer phaco settings,” says Dr. Goldman. “When we only had the traditional longitudinal phacoemulsification, I never saw sub-incisional retained fragments.” He points out that, “Even now, although I only have a small number of patients with retained lens fragments, when I perform the maneuver where I inject saline on the incision, there are definitely a handful of cases every couple weeks where there’s a little chip that comes flying out. I’m pretty convinced that it’s related to the phacoemulsification settings.”
The risk of increased frequency makes this complication more significant than ever according to Dr. Goldman. “I think it is more important than it used to be, because we’re seeing it more frequently,” he says. This, he suggests, is actually due to a combination of factors. “One factor is the new phacoemulsification settings we’re using, whether it’s torsional or transverse or the other phacodynamic changes that we are relying on, that cause a little more turbulence within the anterior chamber,” he says. “The pieces are being broken up so quickly, oftentimes a little piece gets sling-shoted around the eye, and typically because of the way fluid is coming out of the port, the fragment will get trapped right under the phaco tip; and because of some wound edema at the time of surgery, it is missed until postoperative day one when the patient is sitting upright and the chip has floated down into the inferior angle.”
Another reason that more retained nuclear chips are being seen, according to Dr. Goldman: the increase in intra-operative floppy iris syndrome due to the aging of the patient population and their use of Flomax (tamsulosin hydrochloride) and its derivatives. “Although we have effective ways to treat it, every once in a while when we’re caught off-guard with a case of IFIS, the surgery can get a little more tricky and in trying to avoid grabbing the iris, we may miss a little piece of nuclear material,” he says. “Now that we know more about the nature of IFIS we are better prepared for it, but I think there are still times when we get caught by surprise.” This is especially true with female patients, he points out, because the use of Flomax is typically associated with males, but it is now increasingly being prescribed across the sexes to treat kidney stones because it dilates the ureter muscles. “It doesn’t necessarily take a high dose of this medication for an effect on the iris tissues to be seen,” Dr. Goldman points out.
Risk
Regardless of the cause, Dr. Harvey points out that prevention and management of retained nuclear chips start with being aware of the confirmed risk factors for this complication. The four most common risk factors for a retained chip are use of a highly retentive viscoelastic; a patient-centered problem such as arcus senilis; iris color; and use of an iris hook. “Using highly retentive and space-forming viscoelastic is among the leading cause of experiencing retained nuclear chips because the fragment will stick to it and can remain lodged,” says Dr. Harvey. Other less-viscous viscoelastics can also be high risk, he points out, if they are not removed entirely from the eye at the end of the case. Peripheral cholesterol accumulation, as seen in arcus senilis, is a risk factor for retained nuclear chips, he explains, because chunks of nuclear material can go into the angle and become “essentially invisible to the surgeon because of the opacification from the arcus.” Iris color is a risk factor because in some patients the iris color is almost the same—if not identical—to that of the cataract. “So a piece of nuclear material can sit in the angle and be invisible to the surgeon,” he explains. Finally, iris hooks pose a slight increase in risk, according to Dr. Harvey. “When we use an iris hook it is not infrequent to have the iris bent forward a bit where the hook is holding the pupil, and that will introduce a potential space which widens the ciliary sulcus and makes space available for a chip to fall behind,” he says.
Prevention
Dr. Harvey’s strategy to prevent retention of nuclear fragments begins with being on the watch for errant lenticular material and continues with thorough irrigation of every incision to make sure that no piece has found its way into the lumen of the side port.
“During phaco, when there is an instrument in the side port, it is not uncommon for a chip to migrate to where the second instrument is,” he says. “If it’s not identified, it’s a prime candidate for a residual chip that may require intervention or management changes down the road.”
|
Another way to avoid this troublesome complication, he says, is to keep in mind that highly retentive OVDs are not necessary in cases where the cataract is not very firm and the corneal endothelium is not challenged. “In cases like this, it’s better to use a less retentive viscoelastic so that any pieces that are small and hidden can actually be easily removed and are less prone to sticking in the residual visco that is inside the eye,” he explains.
Dr. Goldman likes to inject either Miochol (acetylcholine) or balanced saline solution in the direction of the keratome incision and follow up with hydration of the paracentesis wound to avoid the possibility of a retained nuclear chip. “If there is a chip, that’s usually where the chip has become lodged, and just by irrigating a bit I usually see the chip become released,” he explains.
Dr. Reeves, too, relies on thorough irrigation to minimize the likelihood of a retained nuclear chip, but also notes the importance of examining the iris for lumps. “In the flakier lenses that I think may be at higher risk for these fragments, I use BSS on a cannula at the end to irrigate under the iris to try to flush out any retained fragments that may be hiding under the iris,” he says. “I also look at the iris carefully to make sure that I don’t see any lumps, because a lumpy section of the iris suggests that there may be a retained fragment there.”
Management
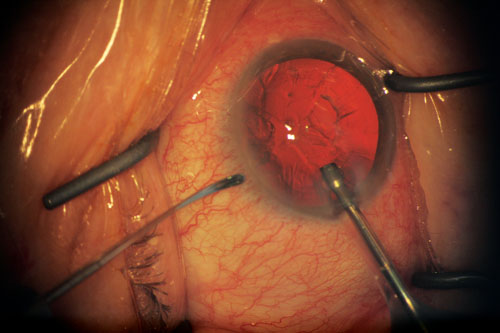
Dr. Reeves points out that while retained nuclear fragments occur infrequently, they are common enough that surgeons should be on high alert for them in each case. “Appropriate management of a retained fragment typically leads to a great surgical outcome,” says Dr. Reeves. The indication to do something, says Dr. Harvey, is if the chip is of a size that would make it likely to create a problem, if there is any swelling of the cornea in the angle or if the IOP is elevated. “Often times, the chip that’s left behind will start to have a delayed immunologic response that will make the trabecular meshwork less efficient, so the eye pressure goes up. It’s not uncommon for those that have been in place or hidden in the angle for several weeks to lead to significant corneal edema, which is a direct immunologic result of the fragment being in that position against the endothelium.”
Dr. Harvey suggests that if the fragment is large and against the endothelium or the cornea it is likely to eventually cause a problem and should be removed; if it is small and not too dense and looks more epinuclear as opposed to nuclear, then observation might be a viable management option. “It is probably much easier for a chip in the angle to be removed in the OR with either irrigation/aspiration and a second instrument to mash it into the port or to use a microincision phaco needle to capture the chunk with no chafing,” he says. “Sometimes when you smash these pieces into the I/A port they break off another smaller piece. This can be avoided with use of a microincision phaco handpiece.”
In the case of retained nuclear material in a very myopic eye that has a deep anterior chamber, Dr. Goldman points out that sometimes it’s rather far from the endothelium, and it can be watched to see if it dissolves on its own with steroid therapy. However, in a shallow hyperopic eye where the chip is in close proximity to the endothelium, and in any other case where it is causing significant edema, he thinks the best option is to take the patient back to the OR and remove it.
The only exception, he says, is if nuclear material is trapped behind the optic, which he points out happens quite rarely. “If it is a small chip, I would consider using a Nd:YAG laser on the entire posterior capsule to move the nuclear material into the posterior chamber. If it is a small piece of nuclear material in the posterior chamber it can be observed and will probably dissolve on its own.”
Dr. Harvey says there are instances when a retained nuclear chip can be observed, with an effective outcome. “Occasionally, if it is not very hard and the patient is doing well on eye drops, it can be observed with a prolonged eye drop regimen and anti-inflammatories,” he says. REVIEW