Vmax Vision announces the addition of voice-guided instruction software to the PSF Refractor, its proprietary subjective refraction technology. The system uses Point Spread Function principles to deliver more accurate and reliable refraction results.
The voice instruction software is the first of its kind, audibly guiding the patient through each refraction test. With the addition of this unique voice instruction, refraction training time is significantly reduced, while also ensuring a consistent quality of testing.
According to Vmax Vision, the decrease in refraction training time brings direct profits to the practice. New doctors can more quickly master the refraction process and begin treating patients. Doctors can more easily delegate the refraction process to technicians in order to decrease chair time and increase interaction with their patients. In addition, because test instructions are computerized, delivery of the test is standardized for the first time, ensuring consistent results across refractions.
Introduced in April 2011, the PSF Refractor measures a patient’s subjective visual response to a point source, enabling a highly precise refraction to 0.05 D—five times more precise than the traditional phoropter. The unique PSF Refraction corrects for higher-order aberrations and helps prevent over-minusing of prescriptions. In addition, the PSF Refraction enables the first true night-vision correction, identifying and correcting nighttime-specific visual aberrations.
For more information, call (321) 972-1823 or visit
vmaxvision.com.
Moria Adds to One Line with New LASIK Instruments
After a successful launch of disposable instruments for cataract surgery and keratoplasty, Moria now extends its One line with three single-use instruments for LASIK and FemtoLASIK surgery: a Kratz wire speculum #17227; a Sinskey manipulating hook #17223; and a manipulating hook #17230.
Moria says its One line of single-use instruments are ideally suited for LASIK surgery, providing convenience and cost savings by eliminating the time and expense of re-processing soiled instruments, guaranteeing new, precise, undamaged instruments for each surgical procedure, and maximum safety during each surgical procedure.
These instruments are sterile, individually packaged in sealed, peel-apart pouches in a box of 10. Each reference can be ordered separately. For information, visit
moria-surgical.com.
 |
Ocusoft has introduced Ocusoft Baby, the first and only eyelid and eyelash cleanser for children of all ages, at Walgreens and Duane Reade Pharmacies nationwide.
Developed by the company behind Ocusoft Lid Scrub, Ocusoft Baby is a mild, tear-less formula that gently removes irritants and debris that can contribute to discomfort associated with blocked tear ducts, pink eye, allergies and other eyelid related conditions in infants and small children. Specially formulated for children’s delicate skin, Ocusoft Baby contains no parabens, fragrances, dyes or quaternium-15, ensuring the utmost comfort.
Ocusoft Baby Eyelid & Eyelash Cleanser is available in individually wrapped towelettes (20/box) and can be found in the baby care aisle at your local Walgreens and Duane Reade Pharmacies. To request professional samples for your trial evaluation, visit
ocusoftsamples.com or call
1 (800) 233-5469.
Supra Scan Photocoagulator Platform Is Customizable
Quantel Medical’s line of laser products is led by the Supra Scan photocoagulator platform, the only laser to include multi-color wavelengths, multi-spot pattern mode and micropulse mode. The Supra Scan is customizable with 532-nm, 577-nm and 810-nm wavelengths, and can include the multi-spot pattern mode with the 532-nm green wavelength.
Micropulse mode with multispot patterns is possible when using the 532-nm wavelength, and there are five possible patterns: squares for pan retinal photocoagulation; triple arcs for pan retinal photocoagulation (periphery); circles for retinal tears; macular grid for diffuse macular edema; and single spot for titrate/finishing touches. The laser, adaptable to a Haag Streit-type slit lamp, offers a continuous parfocal zoom 100 µm to 500 µm (pattern mode), and 50 µm to 500 µm (classic mode). For information, call 1 (888) 660-6726 or visit
quantel-medical.com.
FCI: A First in Nascolacrimal Intubation Stents
FCI Ophthalmics has introduced what it calls the first ever “pushed” monocanalicular nasolacrimal intubation stent, the Masterka. Designed by oculoplastic surgeon Bruno Fayet, MD, Paris, France, the Masterka offers a safer and faster intubation of tear ducts as it does not require the frequently difficult step of recovery inside the nasal cavity.
The Masterka is indicated for congenital nasolacrimal duct obstructions that are resistant to probing. Unlike the traditional “pulled” technique, in which the stent is advanced through the nasolacrimal system and retrieved through the nose by pulling on the guide probe or thread, the Masterka has no metallic probe or suture attached to it and, therefore, it is not pulled out of the nose. Instead, the Masterka is pushed into the nasolacrimal duct and anchored in place at the punctum by a plug-like fixation head similar to FCI’s signature Monoka stents.
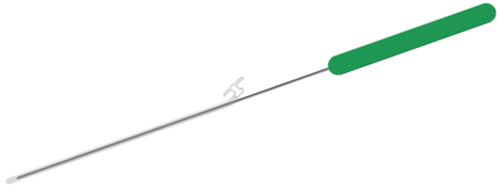 |
The Masterka device consists of a silicone tube molded to a fixation head and pre-mounted on an introducer to facilitate insertion. The introducer is easily and completely removed once the intubation of the lacrimal passages has been completed. The Masterka comes in 30, 35 or 40 mm lengths and must be selected according to each patient’s needs. Special sizing devices are sold separately.
The insertion of the Masterka device using the push technique is performed in the same manner as a nasolacrimal duct probing and the insertion of the traditional stents into the nasolacrimal duct system. A major difference is that the introducer for the Masterka is retrieved by withdrawing it upwards and back out through the canaliculus and punctum, thus avoiding the sometimes traumatic nasal recovery step of pulled intubations. After insertion, the seating of the Masterka anchoring fixation head is performed in exactly the same manner as all of the other devices in FCI’s Monoka family of intubation devices. For information call 1 (800) 932-4202 or e-mail
info@fci-ophthalmics.com.
|
Bioptigen Gains Clearance to Market Envisu Spectral Domain Imaging System
Bioptigen Inc. has received 510(k) clearance from the Food and Drug Administration to begin marketing its hand-held Envisu Spectral Domain Ophthalmic Imaging System devices for patient use. The Envisu SDOIS aids in the diagnosis of physiological and pathological conditions of the eye through non-contact optical imaging. In receiving this regulatory clearance, Bioptigen’s Envisu SDOIS become the first optical coherence tomography imaging systems commercially available in the United States for hand-held and pediatric imaging.
Envisu’s ergonomic, hand-held scanner enables imaging of patients of all ages—from premature and neonatal infants to adults—whether they are upright or supine, ambulatory or confined. And interchangeable lenses allow clinicians to image various structures of the eye, from cornea to retina.
Bioptigen already has received regulatory approval from Canadian, European and Australian authorities to commercially market its Envisu C2200 and C2300 ophthalmic imaging devices.
The National Institutes of Health recently awarded Bioptigen a grant to continue investigation of ophthalmic imaging solutions for premature and neonatal infants. For information, visit
bioptigen.com.
REVIEW



