Vitreous floaters are one of those perennial patient complaints that, traditionally, ophthalmologists simply had to respond to by saying, in the most sympathetic manner possible, “There’s nothing we can really do for them. Hopefully, with time, you won’t notice them as much.” In recent years, however, some surgeons have begun looking into treatments for floaters in certain patients. In this article, retina specialists weigh in on the current state of treatment for vitreous floaters.
The Vitrectomy Option
The main reason ophthalmologists had little recourse when faced with floaters was, for the longest time, the only “treatment” for them was a vitrectomy, which, in many cases, seemed like using a bazooka to kill roaches. However, for certain patients with significant floaters, it can be a worthwhile option, surgeons say.
“Vitrectomy for floaters is a field with much more data than YAG vitreolysis,” says Boston retinal specialist Chirag Shah, MD, MPH, referring to the trend of using the YAG laser to break up floaters. “We have significantly more experience with vitrectomy and are much more comfortable with it. Vitrectomy is also more effective at removing floaters than YAG vitreolysis, which vaporizes and fractionates floaters without actually removing them. The downside, though, is that there are more risks with vitrectomy. For instance, phakic patients who undergo vitrectomy will develop a cataract. Importantly, there is also a small risk of retinal detachment, which ranges from 0 to 10.9 percent in the literature; I estimate the risk to be around 2 to 3 percent based on my experience. There are other risks, too, including the risk of infection, which is around 1:1,000, and the risks associated with local anesthesia.”
In addition to these risks, there are rarer, but still possible, risks, says Jennifer Lim, MD, professor of ophthalmology and director of the retina service at the University of Illinois, Eye and Ear Infirmary in Chicago. “A more catastrophic complication of vitrectomy could be a suprachoroidal hemorrhage—it’s very rare but it could happen, especially in certain at-risk populations,” she says. “Another rare occurrence is inadvertently striking the retina with the vitrector, which could lead to subretinal bleeding or retinal tear formation. Also, although this is unlikely to occur, a patient could potentially cough or make a sudden movement, causing the surgeon to hit the retina or the wall of the eye with the instrument. Though these are rare, extreme examples of complications that could occur, we have to acknowledge them when considering a vitrectomy for floaters. You can’t just blithely schedule a vitrectomy for floaters and think that everything is going to be fine.”
Surgeons say that even though vitrectomy is obviously effective, the severity of the patient’s floaters must be commensurate with the risks involved with full-blown intraocular surgery. “For patients who come in with complaints of floaters, and they say they’re being bothered by them, my most-common response is to recommend observation for a minimum of six months,” Dr. Lim says. “It sounds kind of harsh, but a lot of time these are fresh posterior vitreous detachments, and, over time, the floaters diminish and the opacities settle down. If you’ve ever talked to a person who’s had a PVD, their symptoms are dramatic in the beginning. Then, on the follow-up visit, when we’re still checking for any retinal holes or tears—the patient usually isn’t as anxious or bothered. Then, at six months, many patients come in saying that the condition is much better and they’re fine. For many patients, in addition to observation, I also recommend that they don’t have their ambient lighting so high that it causes high contrast in their environment. Such high contrast makes it easier to notice the floaters. I also teach them how to hold their reading material at an angle so they get less glare and reflections, which can make the floaters less noticeable. It’s important to note that the risk for a retinal tear and/or detachment after an acute PVD is highest in the first six weeks following the PVD, and diminishes at six months. In many cases, if the tear or detachment is going to happen, it will happen by a year after the PVD.”
Though observation and modifying the patient’s environment can help in a lot of cases, there are more severe cases of floaters that surgeons say do need to be addressed surgically. “Most of the patients with acute PVD complain that they see a cellophane-like membrane accompanied by hundreds of black dots floating around their vision,” Dr. Lim says. “If this doesn’t clear, this would be a type of patient presentation for which I’d consider a vitrectomy. There are also the patients with whom I discuss the risks of vitrectomy—I let them know the worst—who still come back months later and say, ‘I’m really still bothered by them.’ For them, I’ll consider the surgery. However, in all cases I have to actually be able to see vitreous opacities. I have to see that the vitreous is cloudy and/or there are a lot of floaters and/or vitreous opacities drifting around.
“Other than patients with floaters and with pathologic conditions, such as a dense vitreous hemorrhage or a retinal tear, which need to be addressed with a vitrectomy, the patients on whom I’ve performed vitrectomy just for bothersome floaters were often graphic designers who worked on the computer all day and were really bothered by their condition,” Dr. Lim adds. “They told me that their floaters affected their job performance by limiting their concentration and visualization of the computer images. One patient even said he’d rather have me remove his eye than live with the floaters any longer. This patient wound up going to a psychologist about it, and got a letter from him stating that the floaters were making him depressed and negatively affecting his lifestyle.” Despite such patients meriting a vitrectomy, Dr. Lim says she still doesn’t proceed with the surgery lightly. “You must remember that a lot of these folks with floaters are also high myopes, who are at higher risk for retinal detachment,” she says. “These are long eyes and, if you do an incomplete vitrectomy like some physicians advocate, eventually that hyaloid is going to pull off. It may happen soon after the surgery and the patient may get a retinal detachment. We’ve seen such cases. On the other hand, the other argument is that if you do a complete vitrectomy, you could tear the retina in two in a very high myope. On the eyes in which I’ve done the
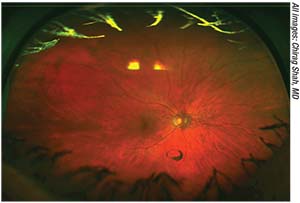 |
| Some vitreoretinal surgeons say a well-defined Weiss ring such as this indicates a good candidate for YAG laser vitreolysis. |
surgery, I do try to go for a PVD, and they’ve done well. I’ve done maybe five such surgeries over the past five years.” She says another situation where vitrectomy might be warranted is patients who see 20/20 but have a lot of contrast sensitivity problems stemming from the floaters. “I would recommend performing contrast sensitivity testing before surgery to demonstrate that it’s decreased because of the floaters,” she says.
Dr. Shah says his threshold for performing vitrectomy on visually significant floaters is lower now during the era of 27-ga. vitrectomy, compared to the days of 20-ga. vitrectomy. “I have a lower threshold because, at least in principle, with 27-ga. the wounds are small, so there’s less risk of hypotony and infection. Still, I only perform about one vitrectomy per year for significant floaters.”
A New Option: YAG
In an effort to ease the burden of patients who are complaining of floaters, but to avoid the risks of intraocular surgery, some ophthalmologists have turned to YAG laser vitreolysis. Some surgeons say this approach may be a middle ground between observation and surgery but, just like vitrectomy, it appears it’s not for every patient.
Michael Tibbetts, MD, is a medical retina specialist in Ft. Myers, Florida, who offers YAG vitreolysis for certain floater patients, and can speak about who is a good prospective patient for the procedure. “A good candidate is someone who has had symptomatic vitreous floaters for at least four months,” he says, “and who has definite evidence of a posterior vitreous detachment on exam. The floaters or vitreous opacities should be correlated with the patient’s symptoms on a thorough fundus examination. Symptomatic patients who are candidates for treatment report impairment in vision with a specific activity, for example with reading, watching television or driving, and this complaint should be documented in the medical record. There are many patients who may report intermittent floaters that aren’t affecting their quality of life, and I don’t think they’re candidates for YAG treatment.” He says the YAG patient also shouldn’t have any other retinal pathology such as retinal tears or detachments, and shouldn’t have any significant opacities in the cornea or lens that would impair the physician’s view of the vitreous. If there is a posterior capsular opacity or significant cataract, Dr. Tibbetts advises treating those problems first.
“A good presentation would be someone with a solitary Weiss ring—which is the vitreous tissue that was previously attached around the nerve head—that’s very dense and, importantly, located in the sweet spot not too close to the retina or too close to the lens,” says Dr. Lim.
Dr. Shah, who doesn’t perform YAG laser vitreolysis in his practice, but analyzed the modality in a small pilot study, says at least one particular type of floater may also not be amenable to YAG laser vitreolysis. “In some cases, there’s a Weiss ring plus a fluffy, white ‘caterpillar-like’ floater in the inferior/anterior vitreous,” he explains. “Dr. Karickhoff termed this a ‘floater duet.’ When a patient with a floater duet
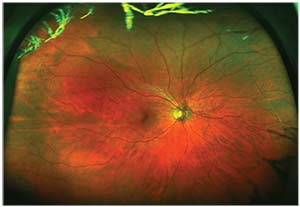 |
| The patient shown on the opposite page following YAG laser vitreolysis for the Weiss ring opacity. |
looks down, the fluffy white floater will drift superiorly and impact vision. A floater duet is very difficult to treat with YAG laser vitreolysis. I inadvertently included a floater-duet patient in our study, and realized that one can treat the Weiss ring, but the symptoms are often unchanged because of the hidden floater duet. If treated with the laser, the floater duet tends to fractionate, creating many small, mobile floaters. This particular patient’s symptoms were not improved after YAG vitreolysis.”
Though there haven’t been any large, randomized studies of YAG laser for floaters, there have been several small case series, as well as the one small, prospective study by Dr. Shah, that show the potential risks include damage to the crystalline lens or an intraocular lens, if present; an increase in intraocular pressure, retinal damage and/or retinal tear or detachment.1,2,3,4 Dr. Tibbetts says, in the 75 to 100 procedures he’s done, he’s seen rare instances of retinal tears on scleral depression postop, but that they all were effectively treated with laser photocoagulation.
“The YAG laser vitreolysis can be performed in the office, with topical anesthesia,” Dr. Tibbetts says. “It can be performed in patients who are phakic or pseudophakic, and it’s a procedure many ophthalmologists have access to by virtue of having access to a YAG laser, though lasers with coaxial illumination are better suited for the procedure.
“YAG laser vitreolysis is effective in treating well-defined vitreous opacities,” Dr. Tibbetts continues. “For more diffuse vitreous opacities, pars plana vitrectomy may be a better option.”
When approaching the procedure itself, Dr. Tibbetts says visualization is key. “The surgeon can only treat what he can see, so if you can’t see the opacity, you can’t provide an effective treatment,” he explains. “Using a YAG laser specifically designed with coaxial illumination, and the appropriate lens, is critical for illuminating the mid-vitreous. For treatment, the surgeon must use sufficient energy to definitively treat the opacity, at least 3 to 4 mJ, as well as a sufficient number of laser pulses. A treatment usually consists of 150 to 200 pulses and, to treat the opacity effectively, sometimes over 300 pulses are necessary. I’d advise starting with patients who are pseudophakic for your first 20 to 30 cases before you consider treating phakic patients.” Dr. Tibbetts performs a careful fundus exam after the treatment and checks the IOP. He then follows up with the patient a week later and performs a dilated fundus exam with scleral depression and checks the pressure again. He asks the patient to score their symptomatic improvement from 0 to 100 percent (100 percent equals complete symptom resolution) and compares this assessment with the fundus findings.
“Once patients report a 70- to 80-percent improvement in their symptoms, I advise observation and a follow-up exam in one to two months,” Dr. Tibbetts says. “If the examination demonstrates residual opacities and the patient is not satisfied with the symptomatic improvement, I may offer an additional laser treatment at the one week postop visit.”
• What the literature says. As mentioned earlier, Dr. Shah and his colleagues performed the only prospective, randomized study of YAG laser for floaters. Although it was a small study, it contains some findings that surgeons can look to for guidance, or for structuring future studies.
In the study, Dr. Shah and his colleague Jeffrey Heier, MD, randomized patients with symptomatic Weiss ring floaters following PVD to either YAG laser or sham YAG. Thirty-six patients received the treatment, and the rest got the sham.
The YAG laser group reported a 54-percent improvement in their symptoms, vs. just 9 percent of the controls (p<0.001). On a 10-point visual disturbance score, the patients in the YAG group improved by 3.2 points vs. 0.1 for the sham group (p<0.001). Nineteen patients in the YAG group (53 percent) r
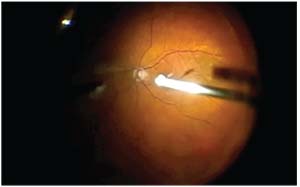 |
| The intervention with almost 100-percent success for floaters is vitrectomy, shown here removing a Weiss ring. |
eported significantly or completely improved symptoms vs. none of the controls (p=0.04). On the National Eye Institute’s Visual Functioning Questionnaire 25, the treatment group showed improved general vision, better peripheral vision, fewer “role difficulties” (i.e., difficulty performing tasks without help from others due to vision) and less dependency than the control group.4
“One striking finding from the study was the significant proportion of patients who had an excellent objective response to YAG vitreolysis, but no subjective response,” Dr. Shah says. “Specifically, eight of 32 patients reported 0-percent improvement in symptoms after YAG vitreolysis, but 7/8 had significant objective improvement based on before and after color photography as determined by a masked grader. This was interesting—and concerning—because it means that even though, objectively, a surgeon can vaporize most of a Weiss ring, there are still some residual particles that bother the patient as much as the initially large Weiss ring floater. This speaks to the importance of patient selection, not just floater selection. Many patients who are bothered by floaters have high visual demands and can be difficult to satisfy. So, it seems that for this subgroup of patients, very little can be done outside of vitrectomy to satisfy them. For the remainder of the cohort in our study, however, when there was a good objective result, there was a correlated good subjective response. That is the difficulty with this field: There’s so much subjectivity that it can be hard to select patients. This is why it’s important to select patients who are easier to satisfy, and who have floaters that are more discrete. Patients with one Weiss ring floater and realistic expectations seem to be easier to satisfy with YAG laser vitreolysis than those with hundreds of diffuse floaters and/or significant anxiety about their floaters.”
Surgeons say there are still many unanswered questions about YAG laser vitreolysis, such as: Are there different efficacies with different lasers? What personality types are best suited for the procedure? What are the long-term complications and effects? How many times should patients be treated? For all these questions, given the lack of trial data, Dr. Shah says that surgeons just aren’t certain of the answers. “It’s unknown at the moment,” he avers. “We’re doing an extension to our original pilot study in which we’re bringing patients back two or three years after their YAG laser procedure to see if there are any long-term complications and/or degredation of effect. My feeling is that some patients may lose the treatment effect over time due to progressive myopic vitreopathy. We need much more data. At the moment, I consider YAG laser vitreolysis to be experimental. We need larger, multicenter trials, with longer follow-up, to answer these questions.” REVIEW
1. Delaney YM, Oyinloye A, Benjamin L. Nd:YAG vitreolysis and pars plana vitrectomy: Surgical treatment for vitreous floaters. Eye (Lond) 2002;16:1:21-26.
2. Toczolowski J, Katski W. [Use of Nd:YAG laser in treatment of vitreous floaters.] Klin Oczna 1998;100:3:155-157.
3. Tsai WF, Chen YC, Su CY. Treatment of vitreous floaters with neodymium YAG laser. Br J Ophthalmol 1993;77:8:485-488.
4. Shah CP, Heier JS. YAG laser vitreolysis vs sham YAG vitreolysis for symptomatic vitreous floaters: A randomized clinical trial. JAMA Ophthalmol 2017;135:9:918-923.



