Many surgeons in the United States are already looking forward to being able to offer this to patients who find themselves in similar straits. With that in mind, three surgeons with extensive experience treating these more-aberrated eyes share some of their experience, to help prevent missteps as American surgeons start to move in this direction.
Working Within Limits
Karl G. Stonecipher, MD, medical director for TLC Laser Eye Centers in Greensboro, N.C., and clinical associate professor of ophthalmology at the University of North Carolina, uses Alcon’s Contoura Vision to perform topography-guided ablation. “The FDA approval allows the use of topography-guided ablation to reduce or eliminate up to -9 D of spherical-equivalent myopia, with up to -8 D of spherical component and up to -3 D of astigmatic component at the spectacle plane,” he notes. “For comparison, standard wavefront-optimized platforms treat 0 to -14 D of myopia, 0 to -6 D of myopia with astigmatism, and 0 to +6 D of hyperopia, with or without astigmatism. Other limitations for the use of topography-guided treatment include only treating patients age 18 and over who have a stable manifest refraction—meaning a preoperative spherical equivalent shift of 0.5 D or less over a period of one year prior to surgery—and eyes without previous refractive surgery, keratoconus, forme fruste keratoconus or any other topographic abnormality.”
Dr. Stonecipher explains that the Contoura Vision system creates an ablation pattern by generating a hypothetical reference shape based on the eye’s topography and figuring out how it can ablate tissue to most closely approximate that shape. “The reference shape is calculated based on the peaks and valleys of that eye,” he says. “The maps you see show the actual height data compared to the hypothetical reference shape. Any area taller than that hypothetical surface shows up as red; anything below that level is blue. Think of the warmer colors as a volcanic mountaintop and the cooler colors as the deep blue sea. When the ablation is based on this, it normalizes the corneal shape, reducing aberrations, smoothing the topography and making your optical system better. It also incorporates the principles used in wavefront-optimized systems, aiming to reduce spherical aberration.”
Dr. Stonecipher says that for most patients who fall outside the FDA limits, he resorts to wavefront-optimized treatment with the Allegretto system. “Nevertheless, I measure every person,” he says. “If the patient is a candidate and I can get good measurements, I’ll do Contoura Vision. In my experience, Contoura vision gives me better-than-normal outcomes more frequently. In fact, Arthur Cummings and colleagues just reported that in the Journal of Refractive Surgery.1
Dr. Stonecipher points out, however, that there’s more than one level of astigmatism. “If the cornea is considered abnormal, treating it with this technology is not an on-label option,” he says. “But if I have someone with a cornea that’s normal according to the FDA criteria but has a little asymmetry, this technology will allow me to treat that cornea’s unique topographical features. So it’s important to make a distinction between an abnormal cornea with irregular astigmatism, like keratoconus, and one that’s regular with asymmetry within treatable LASIK guidelines. You can treat those topographical variations.”
Dr. Stonecipher says the results they’re achieving are exceptional. “Our topography-guided treatments are leaving patients with the sharpest uncorrected vision we’ve ever seen,” he says. “We have patients routinely report that they see better after Contoura treatments than they saw before surgery in their glasses or contact lenses. When we participated in the clinical trial with Contoura Vision, we operated on normal corneas and got a third of patients seeing 20/12 and two-thirds seeing 20/16, some of the best data ever seen in an FDA trial. In our practice, many patients are seeing 20/15 and 20/10. I’ve had two patients measure 20/8 after the procedure, which I’ve never seen before.
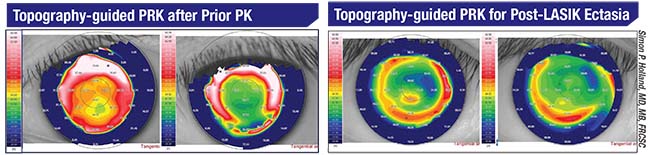 |
| Before and after scans show dramatic improvement in the central cornea following topography-guided treatment in these eyes. |
“As a result, we can tell patients that we’re likely to make their vision better, even if it was pretty good to start with,” he says. “If it was 20/25 or 20/30, we might get you to 20/20, and in 33 percent of cases patients see one line better than they did before surgery. In the FDA trial, 19 percent of participants had one line or more of improvement; 8.3 percent had two lines or more. About a third of the patients saw better by at least one line. For nine out of 10 patients, uncorrected postop acuity without enhancement was equal to their best corrected visual acuity preoperatively.2 That was unprecedented. For the first time we could say, ‘We can reduce your light sensitivity, your difficulty driving at night, your reading difficulty and your complaints about glare.’ In the trial this was all statistically significant compared to baseline at 12 months.”
Outside the U.S.
Simon P. Holland, MD, MB, FRCSC, who practices at Pacific Laser Eye Centre and is clinical professor of ophthalmology at the University of British Columbia in Vancouver, British Columbia, Canada, works with topography-guided technology pioneer David T.C. Lin, MD, FRCSC. Dr. Holland says they currently use the Schwind Amaris 1050, although they previously used the Allegretto Wavelight T-CAT laser. They used it primarily for abnormal corneas, rather than the normal ones currently approved by the FDA.
“We treated irregular astigmatism, keratoconus and ectasia—combining the laser treatment with cross-linking for those corneas—and refractive surgery complications such as decentered ablations,” he says. “We switched to the Schwind Amaris 1050 more than three years ago because of advantages such as high speed and an iris-based multidirectional tracker that includes torsion control. This technology lets us selectively treat the abnormal areas of a cornea and restore more normal topography, which has been shown to alleviate symptoms such as glare, halos and difficulty driving at night. It may also add lines of best-corrected distance visual acuity.”
Dr. Holland says they use transepithelial PRK for the vast majority of their cases. “That approach spares tissue,” he points out. “In post-LASIK cases we treat on the flap, not on the interface where the patient had the previous surgery. The flap tissue isn’t contributing much to the strength of the cornea, so we can do a relatively high degree of treatment on a patient who has, for example, post-LASIK ectasia. Then we cross-link the patient. We haven’t seen a need for going deeper into the cornea by lifting—or making—flaps and then treating the bed. With a transepithelial technique we get our best results.”
Wavefront- vs. Topography-guided
Many surgeons with access to both wavefront and topography-guided lasers resort to wavefront-guided or wavefront-optimized treatment when topography-guided treatment isn’t an option. “In most cases if you compare a topography-guided map and a wavefront map of a virgin eye, once you subtract out the sphere and cylinder from the wavefront map, they look very similar,” says Dr. Stonecipher. “However, the treatments do have some noteworthy differences. For one thing, topography-guided treatment is centered on the line of sight and the vertex of the cornea, while wavefront-optimized treatment is centered on the geometric center of the pupil. The difference between the two, called angle kappa, can be significant.
“Another difference is that with topography-guided treatments we’re just treating the topographic abnormalities on the surface where they occur,” he continues. “Because of that, these treatments are not dependent on pupil size, and the lens and vitreous don’t matter. You aren’t making changes to the cornea that may affect the optical system down the road when the individual undergoes refractive cataract surgery. Topography-guided ablation treats the source of the vast majority of the optical problems—the cornea—rather than the aberrations of the whole optical system, which can be moving targets. To put it another way, we make the lens of the camera better. In fact, our studies have found that 93 percent of patients don’t need wavefront-guided treatment.”3
“Topography-guided and wavefront-optimized systems both work well in appropriate patients,” says Raymond Stein, MD, FRCSC, Fellow of the Royal College of Surgeons in Canada, medical director of the Bochner Eye Institute and associate professor of ophthalmology at the University of Toronto. “However, for patients with irregular corneas, topography-guided is definitely the way to go. The Oculyzer and Pentacam measure more than 20,000 data points on the cornea; this information gets introduced into the laser. Most wavefront units only measure 1,000 or 1,200 data points, so there’s a significant difference in data quantity. In addition, wavefront imaging often has a difficult time with irregular corneas. So most surgeons around the world who are treating irregular corneas use top-ography-guided systems.”
Spherical Changes
One potential problem with topography-guided treatment is that smoothing the cornea can produce a refractive change. There are two main ways to deal with this possibility: Plan to perform a second procedure later to correct the altered spherical component; or estimate the likely change that your procedure will cause and compensate for it during the procedure. Each option has pros and cons.
Dr. Holland says it’s probably best to go for an improvement in best corrected visual acuity, if the patient accepts that, rather than trying to leave the patient plano at distance. “Any topographic change can cause a power change, so many surgeons still do two treatments—one to regularize the cornea and then a second refractive correction once the eye is stable,” he says.
“My partner David Lin developed and published a topographical neutralization technique designed to compensate for the potential refractive shift caused by topography-based treatment,” he continues. “Compensating for the shape change is key if you want to achieve a good outcome in a single treatment when dealing with a very aberrated cornea. It can be challenging, however, because patients with ectatic conditions may have insufficient thickness to do a complete refractive treatment, and there’s always a degree of unpredictability. On the other hand, improving the
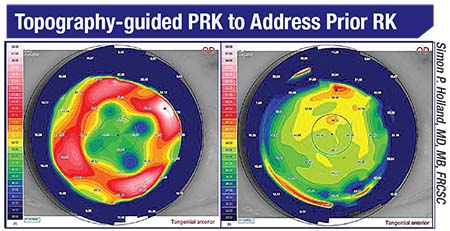 |
| Treatment normalizes a cornea that had previous radial keratotomy. |
“Of course, the patient needs to know about this ahead of time,” he adds. “On our informed consent, we explain that this procedure is not likely to leave the patient free of glasses, but will almost certainly leave the individual with much better vision when wearing glasses or contact lenses.”
Dr. Holland notes that one group of patients who may not be receptive to this tradeoff is those who’ve had refractive surgery. “They almost always want to be corrected for distance vision,” he says. “They usually say, ‘I wouldn’t have had the laser surgery if I didn’t want to be free of glasses and contacts.’ Patients with pathologies such as keratoconus or scarred corneas tend to be more tolerant.”
Dr. Stein agrees. “For these patients, just being able to wear a soft contact lens is a major improvement,” he says. “Of course, we can go back later to correct the spherical component, but we generally don’t use an excimer laser because of their thin corneas. We like to limit the laser ablation to 50 µm.”
Dr. Stein acknowledges that it’s possible to try to compensate for the spherical change during the surgery. “If the prescription is low, we can try to correct a little bit,” he says. “The question is, how much tissue can we safely remove? In patients with ectasia we want to err on the side of caution by not removing too much. On the other hand, in cases such as a decentered ablation or small optical zone, in which cross-linking isn’t necessary, we’ll do the spherical correction. Afterwards, if there’s any residual sphere we can always go back and do a little bit more. The initial treatment would be topography-guided, while the follow-up would be a standard ablation. Corneal thinness isn’t an issue in many of those patients.”
Patient Selection
As with any laser ablation, selecting appropriate patients is a key to getting outstanding results:
• Make sure your patient will be happy if there’s a trade-off. Dr. Stein points out that some patients, despite having irregular astigmatism, are not good candidates for topography-guided treatment. “I wouldn’t do a topography-guided treatment on patients with an uncorrected visual acuity of 20/30, because although these patients could benefit from an improvement in their best corrected visual acuity, the procedure could induce some nearsightedness or farsightedness,” he says. “The bottom line is that you want a satisfied patient.”
• Warn patients they may need a second procedure. “Be sure to advise patients when you start that it’s probably going to take two treatments,” says Dr. Holland, referring to the possibility that correcting the corneal surface may alter its spherical power. “They may need a touch-up.”
• Remember that some patients may benefit more than others. Dr. Holland says the patients most likely to appreciate the value of this treatment are those with the most aberrated eyes. “The best patients are those who will gain the most,” he says. “Those are the ones with severely aberrated corneas, such as post-refractive surgery complications, keratoconus, post-LASIK ectasia or central islands. These patients are highly symptomatic.”
Dr. Holland also notes that in most cases, the more central the abnormality, the better the results he gets. “That’s because there’s less tissue to remove, particularly in the ectatic patients,” he says. “For example, pellucid marginal degeneration cases can be difficult because you have to treat a wider area of thinning and elevation and use more tissue. But eyes with a more central problem, such as those needing optical zone expansion, do very well with topography-guided treatment.”
• Avoid treating corneas with steepening outside of the pupillary zone. “The fact that topography-guided ablation aims to smooth the cornea can be a problem in some cases,” notes Dr. Stein. “It flattens steep areas and steepens flat areas. If a cornea has steepening outside of the pupillary zone, the flat area would be over the pupil and the laser would work to steepen that. As a result, it could make the patient significantly more nearsighted.”
• Beware of misleading epithelial abnormalities. Although topography-guided treatment is excellent at eliminating corneal abnormalities, it’s important to correctly identify the type of abnormality you’re seeing. “You can’t just look at the topography to make a diagnosis of keratoconus,” notes Dr. Stein. “You have to do a proper slit-lamp examination to make sure there isn’t any epithelial abnormality, because there are a variety of what we call pseudokeratoconus conditions.
“These conditions include a small focal scar, punctate keratopathy and amiodarone-induced vortex keratopathy,” he notes. “Amiodarone is a lifesaving cardiac medication that can cause topography abnormalities. That’s a challenge to treat, even if we identify the correct problem, because we can’t ask the patient to stop a lifesaving medication. Another misleading condition is epithelial basement membrane dystrophy. That can cause big problems because it’s a transient condition that doesn’t need topography-guided PRK; it just needs a debridement of the epithelium.
“If you mistakenly use topography-guided laser to treat those conditions, you can induce irregular astigmatism in the stroma that may be difficult to correct,” he continues. “In those conditions the stroma was normal all along; what’s abnormal is just the very superficial layer, which can change over time.
“This is one reason you can’t just rely on the corneal measurements made by the topography-guided system,” he adds. “That information is helpful in making a diagnosis, but in addition to that, a proper slit lamp exam is important to rule out pseudokeratoconus conditions.”
Surgical tips
• Don’t try to treat complex corneas until you’re well acquainted with the technology and the way it works in your hands. Dr. Stonecipher says his best advice for surgeons just starting to explore this technology is to walk before you run. “You don’t want to begin by taking all of your highly aberrated postoperative LASIK, PRK and cataract patients and trying to fix them,” he says. “You need to understand the technology. You want to do primary, normal eyes first, get your nomograms established and build your comfort level with the technology. Spend time with a surgeon who has a lot of experience with it, and consider taking one of the excellent courses on this topic taught by John Kanellopoulos, MD, at most of the major ophthalmology meetings. And when you do start treating more complex cases, contact one of those more-experienced surgeons and share the details of any challenging case you’re working on; most of them will be happy to help you.”
• Treat every patient as a unique case. Dr. Holland notes that one factor making topography-guided treatment challenging is that every case is different. “It’s really hard to apply the lessons you learned from one eye to another eye when you’re normalizing aberrations,” he says.
• Know when cross-linking is essential. “In our practice we see a lot of patients with keratoconus and pellucid marginal
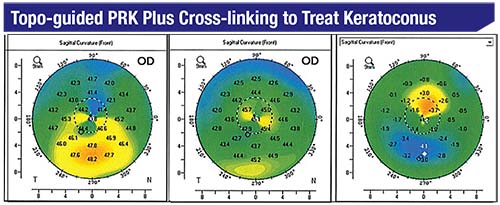 |
| Preop map (left) shows evidence of keratoconus with inferior steepening. Postop map (middle) shows significant reduction in the irregular astigmatism. The difference map (right) shows flattening of the inferior cornea and steepening of the superior cornea. This patient’s best corrected visual acuity improved from 20/100 to 20/25 by six months. |
Dr. Stein notes, however, that not all topography-guided treatments have to be combined with cross-linking. “There are a number of indications for topography-guided treatment that aren’t related to keratoconus or PMD,” he says. “It’s a great treatment for prior PRK or LASIK patients who ended up with a decentered ablation. It’s also helpful for laser vision correction patients who have a small optical zone that’s causing glare and halos. Those are cases that don’t need cross-linking. They’re irregularly shaped cor-neas, but not weakened corneas.”
• Make sure the input data is good. Dr. Stonecipher notes that you can see the system’s analysis of the data quality onscreen, but sometimes just looking at the image will reveal a problem. “There are three onscreen markers whose color—green or red—tells you whether the data is acceptable,” he says. “If all three of these are green, I know that my technician took a good picture and I can rely on this diagnostic picture for treatment. But sometimes the image on the screen will make it obvious that data is being blocked by the patient’s nose, prominent brow or long eyelashes. That’s a measurement I wouldn’t want to use for treatment.”
• Treat any problems on the ocular surface before measuring the cornea. “Treat any dry eye, allergy or ocular surface disease before you measure the topography,” says Dr. Stonecipher. “If you have a bad ocular surface, whether before or during surgery, you’ll get bad data.”
• If you use a femto laser to make the flap and get an opaque bubble layer, wait for the bubbles to clear before measuring the cornea. Dr. Stonecipher notes that it may take 10 or 15 minutes for the bubbles to clear when this occurs, but a study conducted by his daughter Megan Stonecipher and him4 found that trying to measure the cornea in the presence of an opaque bubble layer is the number- one source of requiring an enhancement when performing laser ablations.
• Always work toward creating a personal nomogram. Because altering the surface of the cornea may alter the spherical refraction, Dr. Stonecipher points out that surgeons should always be tracking their results to help create a personal nomogram that can minimize any unwanted shift. “We’re using internet-based refractive analysis, IBRA for short, and Datalink, just as we do with our wavefront-guided and wavefront-optimized outcomes,” he says. “Those will help you compensate for induced sphere, based on the characteristics of the cornea you’re treating and the treatment you’re performing.
“The nice thing about Datalink and IBRA,” he adds, “is that they’re based on data from thousands of eyes, so even if you’re just starting out you’ll have a nomogram to work with.”
Not Easy, but Worth It
Dr. Stein believes that most practices that plan to offer patients cross-linking should also offer topography-guided treatment. “If you’re a corneal specialist and you’re going to offer cross-linking and hope to have a successful, busy practice, I think you need to offer a topography-guided laser option,” he says. “On the other hand, if you’re just going to do occasional cross-linking, I wouldn’t offer topography-guided. This is not a simple technology. You have to spend time working with it and gain experience if you want to do it well.”
Dr. Stonecipher notes that he’s found topography-guided treatment to be a great practice-builder, for several reasons. “These patients are seeing as clearly as they previously saw with their glasses and contact lenses,” he notes. “My current enhancement rate is 0.5 percent. So people are coming back happy, not needing a touchup. That’s significant, because when I have to do a touch-up, patients think the procedure failed. If I can nail it first time out of the box, they’re pretty happy. If I can give them good quality of vision with no halos, starburst, etc., they’re even happier. In fact, I know some surgeons are charging a premium for performing it, so it definitely can provide added value to your practice.”
Dr. Holland agrees. “If you’re going to use topography-guided treatment off-label, you’ll find there are great rewards for both the patient and the surgeon,” he says. “However, you have to be prepared for a few bumps in the road to get there. There’s no out-of-the-box technique that will work for all of the abnormalities you’ll find in corneas.”
Nevertheless, Dr. Stonecipher says that he’d recommend that surgeons add this to their armamentarium. “Topography-guided is allowing us to attain remarkable outcomes and much lower enhancement rates, much better than we were achieving with previous technologies,” he says. “The proof is in the pudding. It’s improving our better-than-20/20 rate; it’s improving our best-corrected vs. uncorrected visual acuity; and it’s allowing us to offer patients even better optical acuity than they were born with. It’s good stuff.” REVIEW
Dr. Stonecipher is a consultant for Abbott, Alcon, Allergan, Bausch + Lomb, Ellex and Nidek. Drs. Stein and Holland have no financial ties to any product mentioned.
1. Cummings A, et al. Prospective evaluation of outcome in patients undergoing treatment for myopia using the WaveLight refractive suite. J Ref Surg 2017;33:5:322-328.
2. Stulting D, Fant B, T-Cat Study Group (Stonecipher KG). Results of topography-guide LASIK custom ablation treatment with a refractive excimer laser. J Cataract Refract Surg 2016;42:1:11-18.
3. Stonecipher KG, Kezirian GK. Wavefront-optimized versus wavefront-guided LASIK for myopic astigmatism with the ALLEGRETTO WAVE: Three-month results of a prospective FDA trial. J Refract Surg 2008;24:S424-S430.
4. Stonecipher M, Stonecipher K. Influences on enhancement rates in laser vision correction. US Opthalamic Rev 2016;9:2:2-4.



