Diagnostic Steps
By asking the right questions, surgeons say you can catch a lot of potential problems preop during your exam:
• History. Refractive surgeons say listening to patients’ experiences with contact lenses can give a lot of clues. “We’ll ask patients if they can wear contact lenses comfortably or if they have a history of wearing them but then having to stop because of irritation,” says Edward Manche, MD, director of cornea and refractive surgery at Stanford University’s Eye Laser Center. “We also get a handle on symptoms they’re having that might be related to dryness.”
Julie Schallhorn, MD, assistant professor of clinical ophthalmology at USC’s Keck School of Medicine, says you can drill down deeper into the contact lens complaints. “A lot of contact lens wearers have irritation after wearing their lenses for a while,” she says. “However, some may say that when they wake up in the morning their eyes are really irritated; that clues me in to the possibility that they may have a nocturnal exposure problem. A lot of young people, in particular, have some nocturnal exposure in which they open their lids a little at night. If you ask them about it, they’ll say their eyeballs feel as if they’re ‘Velcroed’ to their lids in the morning. Others may say that their eyes feel terrible when they’re not wearing contact lenses, but as soon as they put in their lenses they feel great. This is a sign that there may be another ocular surface issue going on that the contact lens is masking, such as really bad meibomian gland dysfunction with a rapid tear-film breakup time. For them, the lens acts like a bandage and keeps tears on the cornea. But, when they remove it, they have a rapid TFBUT and sense the dryness.” Dr. Schallhorn also says to be sure to check about systemic diseases like secondary Sjögren’s, rheumatoid arthritis and scleroderma, all of which can be related to dry eye.
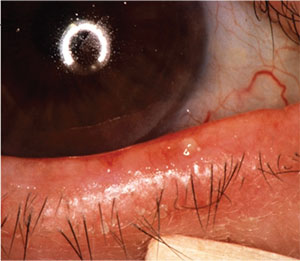 |
| Patients with meibomian gland issues and rosacea will need special attention preop. |
• Exam. Dr. Manche says a thorough anterior segment exam should turn up any issues. “We do vital dye staining with lissamine green and fluorescein,” he says. “We’ll do Schirmer’s tests to make sure we don’t have someone with Sjögren’s. We then do a good external ocular exam looking for meibomian gland dysfunction.” Surgeons will press a little on the lid margin to try to express some meibum. “See if it runs clear or if she has meibomian glands that are backed-up and not working,” says Dr. Schallhorn. “I’m also looking at the conjunctiva. Is there chalasis? If there is, it can be a sign of chronic dry-eye irritation and a cause of that irritation. I also evert all the lids of contact lens wearers to look for giant papillary conjunctivitis. On the cornea, note if they have any punctate epitheliopathy, and the exposure pattern. Is the pattern inferior or is it diffuse, as in toxic keratopathy?”
Bakersfield, Calif., surgeon Daniel Chang, MD, also says your corneal topographer can clue you in to surface issues. “Corneal topographers that do not employ a smoothing algorithm, such as the Zeiss Humphrey Atlas 900 that I use, can give a sense of the regularity of the ocular surface,” he says. “If the surface is irregular, the topography will be bumpy and granular.
“After the initial consultation, about a week or so before surgery, my patients come back for preoperative measurements,” Dr. Chang continues. “At that visit, we will have stressed the ocular surface—performed refractions, multiple diagnostic tests and dilation—and if their ocular surface can hold up to that, they’ll probably do OK with LASIK. If it doesn’t hold up, that’s a red flag.”
Treatment
Though ocular surface disease is often a mix of MGD and aqueous deficiency, physicians note that different treatments are more effective on one form or the other.
• MGD. “For meibomian gland disease, I’ll recommend lid hygiene and lid washes,” Dr. Schallhorn says. “There are many products out there that you can use. I also tend to supplement these patients with omega-3 fatty acids and flaxseed oil, at least leading up to the refractive surgery. And, depending on how bad it is, I at least get them to do some warm compresses. Then, depending on the severity of the disease, you can do oral tetracyclines. I like doxycycline or azithromycin, or a course of a steroid/antibiotic combination, depending on how bad the disease is. For most patients with MGD, however, lid hygiene, warm compresses and dietary supplementation will resolve the problem.”
• Aqueous deficiency. Dr. Manche discusses the possibility of Restasis with these patients. “A lot like to start on Restasis initially,” he says. “I give that a six- to eight-week trial and see how they respond. If they respond well and the surface looks good, then I’d consider performing refractive surgery. If they have a poor or half-way response, then I’d consider moving to punctal occlusion. If they do well with that approach, with clearing of any signs or symptoms, then they’re reasonable candidates for surgery.”
| Refractive News |
| For surgeons hoping to get more functionality from Avedro’s suite of cross-linking products, their hopes were answered in late July when the U.S. Food and Drug Administration approved the company’s Photrexa, Photrexa Viscous and KXL system for use on patients with post-refractive surgery corneal ectasia. This approval comes hot on the heels of the system’s initial approval for use in keratoconus. Avedro notes that ectasia, which can occur within a week of a corneal refractive procedure and can decrease best-corrected and uncorrected vision and induce visual aberrations, affects about 160,000 individuals in the United States. The Photrexa photoenhancers and the KXL system will be available by the end of the year, Avedro says. |
Dr. Schallhorn takes more time with aqueous-deficiency patients. “If someone is totally aqueous-deficient or has tear production problems prior to surgery, I’d take more time to observe them to see if they actually do or not, because that’s something that will get worse after surgery,” she says. “And, it’s more concerning than a tear-film insufficiency/MGD-type picture. I’d consider putting them on topical cyclosporin and monitoring them to see if they start making more tears or if on the first day they saw me they were aberrantly low and they’re actually fine after that. I’d want to see them again to look at their tear film and supply over a few visits before deciding to do refractive surgery.”
• The red flags. Despite all this attention and therapy, there will be patients who simply aren’t candidates for refractive surgery. “If they’re truly aqueous-deficient—they’re not making tears at baseline and they have the classic epitheliopathy and exposure pattern—I don’t do refractive surgery on them,” Dr. Schallhorn says. “If they have severe, unremitting MGD, with an incredibly unstable tear film that doesn’t get better with treatment, I’d also consider not operating on them.”
• Postop therapy. Though preop screening and treatment will help most patients, some will need ocular surface assistance for a short while postop. “For transient dry eyes following LASIK, my approach is primarily tear supplementation,” says Dr. Chang. “If symptoms are still significant, I’ll start Restasis, reminding them that it does take some time to have an effect. In some cases, I’ll offer punctal plugs for a more immediate improvement. Patients often improve in a few weeks. With good preoperative screening, postoperative ocular surface issues are rarely severe.” Dr. Manche says if the cornea becomes inflamed, he can extend the patient’s topical steroids for several weeks to help quiet it. “Generally, though, if the eyes are well-controlled before surgery, they tend to recover quickly,” he says. REVIEW
Dr. Chang has received consulting fees from Allergan and Zeiss. Drs. Manche and Schallhorn have no interest in the products discussed.



