As the complexity of managing dry eye has grown, so too has clinicians’ need for help in navigating the sea of diagnostic and treatment options. This year, that focus has culminated in the appearance of three new algorithms intended to make dry-eye management easier for the clinician. Here, three surgeons who helped to develop these algorithms explain how the algoriths were created, the intended thrust of each algorithm and how they differ from one another.
TFOS DEWS II
One of this year’s three new dry-eye treatment algorithms is part of the Tear Film and Ocular Surface Society Dry Eye Workshop II report, better known as TFOS DEWS II. TFOS DEWS II was recently published as a series of focused reports in the July 2017 issue of The Ocular Surface; the series includes a Management and Therapy Report that discusses the new treatment algorithm. (TFOS DEWS II also offers updates of the definition, classification and diagnosis of dry-eye disease, as well as an assessment of its etiology, mechanism, distribution and impact.)
The intention of the authors was to make the TFOS DEWS II report evidence-based. Accordingly, the members of the management and therapy subcommittee reviewed the literature concerning current treatment options of all types, including treatments for tear insufficiency and lid abnormalities, anti-inflammatory medications, surgical approaches, dietary and environmental modifications and complementary therapies, to determine what concrete evidence currently exists to support each option.
“In this report we discuss almost every treatment that’s ever been described, even options such as using honey in the eye,” notes J. Daniel Nelson, MD, FACS, FARVO, professor of ophthalmology at the University of Minnesota and an ophthalmologist in the HealthPartners Medical Group in Bloomington, Minn. (Dr. Nelson was chair of the TFOS DEWS II report project.) “However, the focus is on the literature: Which treatments can be recommended based on the evidence? What’s the pathophysiological justification for a given approach? Of
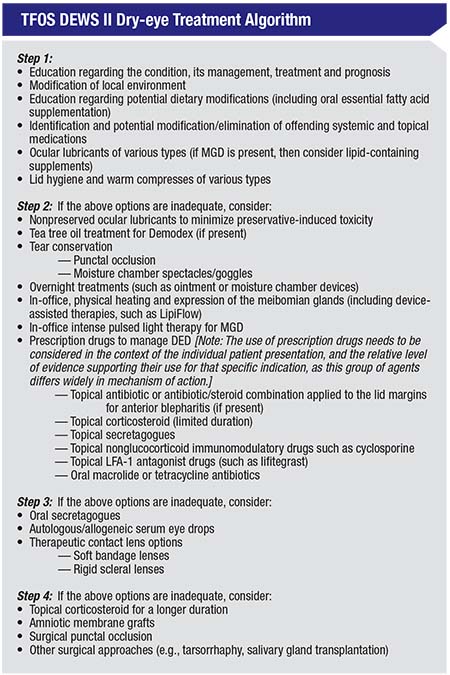 |
| The authors of the TFOS DEWS II treatment algorithm note that when patients do not respond to a given level of management or exhibit more severe dry-eye disease, the next level of management is recommended; in some cases, the previous therapy may be continued. Options within a category are not ranked according to importance and may be equally valid. Management options chosen should be dictated by the severity and etiology of the DED state. (For more information, see Jones, Downie, Korb et al, 2017.1) |
Dr. Nelson says a big part of choosing an appropriate treatment still comes down to determining whether the problem is primarily evaporative or aqueous-deficient, or a combination of both. “One of the big challenges of the report was how to define the subtypes of dry eye,” he says. “We opted to define it in terms of aqueous-deficient and evaporative disease. These classifications have been used for many years; everybody understands them, and in general they are probably the closest you’re going to get to the right terms. However, it’s clear that there’s a huge overlap between evaporative and aqueous-deficient dry eye. In fact, the report emphasizes that the lipid layer is not solely responsible for preventing evaporation; the entire tear film is involved. So even in an aqueous-deficient eye, you’re going to end up having an evaporative component.”
Severity-based Treatment
The recommendations in the TFOS DEWS II treatment algorithm are based on four levels of disease severity. Dr. Nelson explains the four stages and how they’ve been modified since the first TFOS DEWS report. “The new algorithm can be thought of as taking things from the least interventional—and in some cases the least expensive and least risky—up to more significant interventions with greater cost and perhaps more risk,” he says. “Stage one is largely focused on education, topical lubricants and physical therapy—meaning lid hygiene and warm compresses. At this stage you’re identifying whether the patient has any systemic conditions such as Sjögren’s; you might need to treat the patient systemically for that disease. The options at this level are mostly the traditional treatment options, although we’ve added dietary modifications such as the addition of omega-3 fatty acid supplements.
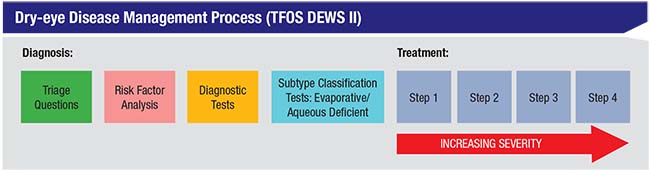 |
| The TFOS DEWS II report proposes following a process like the one pictured above when initiating dry-eye treatment. The authors note that this is not a rigid, stepwise approach, but an organizational tool. They also note that when diagnosing and deciding on a treatment there is a broad spectrum of disease that may encompass both evaporative and aqueous-deficient dry eye. |
“Stage two is partly concerned with the presence of inflammation,” he continues. “It adds in new treatment alternatives designed to counteract inflammation, including prescription drugs such as topical antibiotics, corticosteroids, secretagogues, cyclosporine A, lifitegrast, nonglucocorticoid immunomodulatory drugs and oral macrolides like azithromycin. It also includes tea tree oil to treat Demodex, and intense pulsed light therapy.
“If those treatments are not adequate, stage three is more interventional, both with nonprescription medications and interventions such as punctal occlusion,” he says. “This stage involves more aggressive approaches, including oral medications such as secretagogues, as well as autologous serum and therapeutic contact lenses. Finally, stage four includes options such as using topical corticosteroids for a longer duration, and amniotic membranes. Also, if you’re at this level and punctal plugs aren’t staying in place, you might want to resort to surgical punctal occlusion and/or tarsorrhaphy.”
In the management report, the authors state that their treatment algorithm should not be seen as a rigid, stepwise approach, but as an organizational tool to aid treatment decisions. They believe the heterogeneity of this patient population precludes an overly formulaic approach, so treatment should be individualized based on each patient’s signs, symptoms and situation. “As all clinicians treating dry eye know, you often have to customize your treatment to the patient,” Dr. Nelson says. “You may start with steps one and two; or you might jump to step three. If a patient comes in with Sjögren’s and severe dry-eye symptoms, I’ll be using treatments from stages one, two and three all at the same time. Based on experience, I know that this patient will require more than just the topical interventions; the patient will need topical anti-inflammatories, and I may have to treat with systemic medications. So dry-eye treatment is not really linear. Our algorithm can be seen as a list of options that we suggest you try.”
Dr. Nelson notes that the choice of which treatment options to pursue may be partly risk-based. “If a patient’s dry-eye problem is clearly not an immediate threat to her cornea or vision, you know you’ve got more time to try alternatives than when somebody comes in with a lot of corneal staining, perhaps a big epithelial defect, filaments, and so forth,” he says. “In the latter situation you know you’ll have to be more aggressive or you might put the eye at risk.”
Dr. Nelson says he believes that new alternatives that appear in coming years will still fit into one of these four treatment stages. “If the world’s greatest artificial tear comes along and solves everybody’s problems, that would still probably be a stage-one treatment,” he says. “On the other hand, if we came up with a great surgical treatment, that would still likely be stage four because it wouldn’t be the first thing you’d jump to.”
The CEDARS Algorithm
Another dry-eye treatment algorithm was published earlier this year by the Cornea External Disease and Refractive Society, or CEDARS.2 It takes a different approach to dry-eye disease treatment than the TFOS DEWS II report.
A driving force behind the CEDARS algorithm was Mark S. Milner, MD, FACS, associate clinical professor at Yale University School of Medicine and co-founder and co-medical director of the Precision LASIK Group in New Haven, Conn. “I’ve had a niche dry-eye practice for 15 or 20 years now,” he explains. “I give many lectures every year on dry-eye disease and related clinical studies, and I’ve noted that most dry-eye treatment algorithms are based on severity,” he says. “They suggest treating mild dry eye differently than moderate or severe dry eye.
“Although this approach is commonly accepted and considered to be standard-of-care, I thought the focus of such an algorithm should be on the diagnosis rather than the severity,” he continues. “I’ve always felt that it didn’t make sense to treat mild aqueous deficiency the same as you’d treat mild blepharitis. So for the past 15 years or so I’ve been teaching a different way of approaching dry-eye disease, and that approach culminated in the CEDARS treatment algorithm that we recently published.”
Dr. Milner notes that most doctors treating dry eye separate patients into two categories: aqueous deficiency and evaporative disease. “The problem is, evaporative disease is a very big category,” he says. “I realized that if you separate your dry-eye patients into four categories instead of two, you could have a much more directed treatment. Aqueous deficiency is one category, but you can break up evaporative dry eye into three separate categories. The first is evaporative based on goblet cell or mucin deficiency. The second category is blepharitis, although it is possible to have blepharitis without necessarily having an evaporative problem. The third evaporative category is exposure-related dry eye. These patients have an evaporative problem because their eyes are not closing all the way.”
Eventually, Dr. Milner took this line of reasoning one step further. “In 2009, after giving a lecture at the New England Ophthalmic Society, I realized that we needed a fifth category, which is what I call the co-conspirators,” he says. “The co-conspirators are those diseases that masquerade as dry eye or exacerbate it. Masqueraders include Thygeson’s superficial punctate keratopathy; superior limbic keratoconjunctivitis; medication toxicity or medicamentosa; mucous fishing syndrome; conjunctivochalasis; allergic/atopic keratoconjunctivits; and chemical toxicity. A lot of these are often misdiagnosed as dry eye. If a patient has one of these problems, you may be spinning your wheels trying to treat the patient for dry eye, and not have much success.
“We look at the CEDARS algorithm as a better approach to treating dry eye,” he continues. “Now, when patients walk in with keratitis signs and symptoms, we can separate them into the four categories: aqueous deficiency; evaporative based on goblet cell and mucin deficiency; blepharitis; and exposure. Then our algorithm provides a first-, second- and third-line treatment you can use in each situation, based on the diagnosis—not necessarily based on severity. If none of these diagnoses makes sense, then we look for the co-conspirators.”
Maximizing Options
In addition to the CEDARS algorithm’s focus on multiple diagnostic categories rather than severity, it also includes a broad range of treatment suggestions. The published report2 discusses each treatment in detail and provides references with clinical evidence supporting its use—if any exists. “I use a lot of esoteric treatments for dry eye, things that many clinicians don’t commonly use,” explains Dr. Milner. “In addition to options such as topical hormones and autologous serum, I sometimes treat with albumin or medroxyprogesterone or DHEA drops. Many of these options are off-label and compounded, so they’re not commercially available.
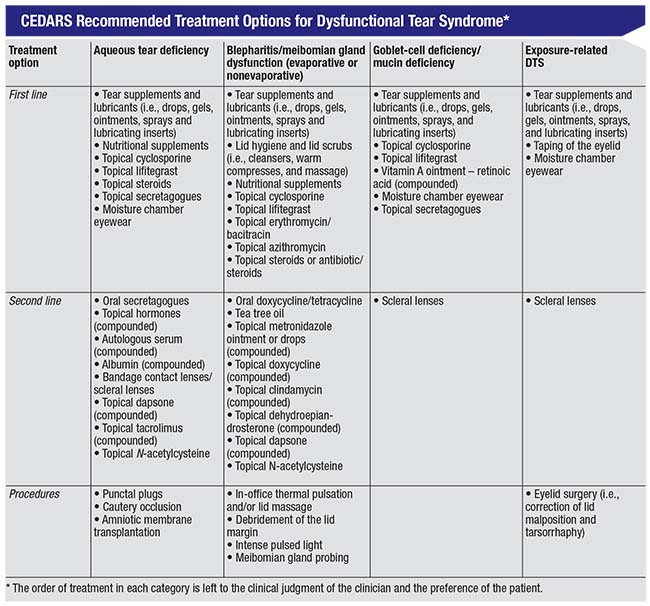 |
| The CEDARS treatment algorithm is arranged by diagnostic category rather than disease severity. It was intended to cover a comprehensive list of treatments, including many that are off-label and compounded, as well as many that are not widely known in the ophthalmic community. It provides first-, second- and third-line treatments that can be used in each situation—though not necessarily based on the severity of the patient’s disease. (For more information, see the complete published report. |
“For example,” he continues, “I often use topical metronidazole ointment to treat blepharitis. It’s a very efficacious treatment that most doctors are aware of as a treatment for rosacea dermatitis, but few are using for blepharitis. Metrogel is a commercially available treatment for rosacea dermatitis on the face, but some compounding pharmacies will make it into an ophthalmic preparation that’s great for posterior blepharitis secondary to rosacea. I’ve used it for 20 years. It’s safe and easy to use and works well.
“Several of my colleagues in the Cornea Society were discussing dry-eye algorithms, and we decided that this particular approach was worth publishing,” he recalls. “This was what initially led to the idea of creating an algorithm refined by a CEDARS panel. So about two years ago with the help of Ken Beckman, MD, and Jodi Luchs, MD, co-authors on the paper, we started the process of forming a CEDARS dry-eye panel, and earlier this year we published the algorithm.”
Dr. Milner points out that the report also returns to the use of the briefly popular term “dysfunctional tear syndrome.” “I believe it makes sense to go back to this because the term ‘dry-eye disease’ seems to imply to the patient and doctor that the problem is just a lack of tear production,” he explains. “Calling it dysfunctional tear syndrome does a better job of conveying that it’s not just about tear quantity—it’s about tear quality as well. The reality is, we need to treat both the abnormal quality and quantity of the tear film.”
But Will They Use It?
A key issue with any algorithm is whether clinicians will actually find it useful. “For the past 10 years, I’ve taught this diagnosis-based approach,” Dr. Milner says. “The feedback from doctors has been very positive. Dry eye is a very complex disease, for many reasons, and for years we’ve had very few good treatments. Now we have two commercially available drugs, and although this has helped, doctors are still frustrated. Doctors say that they love Restasis and Xiidra, but ask what else they can do when they need to add additional treatments. The CEDARS algorithm lists a lot of esoteric treatments, as well as a nice road map on how to add them to a treatment regimen, based on what they find and what the patients are saying. I think it’s a more directed approach to solving a lot of our dry-eye treatment problems.”
Dr. Milner notes that many doctors don’t think of dry eye as a multi-treatment disease. “In my experience, that’s a mistake,” he says. “Dry eye, like glaucoma, is often a multitreatment disease, especially if the disease is more severe. Patients may need cyclosporine and lifitegrast and plugs and maybe a topical antibiotic. Our algorithm helps provide numerous treatment alternatives to try in those situations.”
The ASCRS Algorithm
A third dry-eye management algorithm is being developed by the American Society of Cataract and Refractive Surgery’s corneal committee. (The ASCRS algorithm should be published before the end of 2017.) Francis Mah, MD, who specializes in cornea, external disease and refractive surgery at Scripps Health System in San Diego, is a member of that committee; he explains the thrust of their approach and how it differs from the other two algorithms already published.
“Christopher E. Starr, MD, FACS, a cornea specialist at Weill Cornell Medicine in New York, has been leading the charge in this endeavor,” notes Dr. Mah. “At this point, the algorithm has been approved by all of the committee members. In fact, we’ve already put it into use in the clinic, and we’re preparing to publish a second paper talking about how the algorithm works in real clinical practice.”
Dr. Mah notes several differences between the ASCRS algorithm and the others. “The CEDARS algorithm is extremely inclusive,” he says. “It incorporates a lot of different tests and therapies, many of which are not FDA-approved. I see it less as an algorithm than an encyclopedic list of everything relating to treating the ocular surface.
“The TFOS DEWS II algorithm is very scientific; they reference the medical literature extensively,” he continues. “However, it’s a very simple algorithm that leaves a lot up to the clinician. I think it’s more a source of suggestions and guidelines than a specific description of how to proceed. For example, in each stage they list some treatment options, but they don’t go into great detail as far as the specific order in which to use them. The same thing is true of their diagnostic recommendations.
“Ours is a much more specific type of algorithm,” he notes. “We go into detail about what to do, and what order to do it in: If you find this, then do that. It’s almost like a recipe. We also go into great detail about conditions besides dry eye and blepharitis, such as allergic conjunctivitis, infectious, viral or bacterial conjunctivitis, and anterior basement membrane dystrophy, many of which can masquerade as dry eye or blepharitis. In general, our algorithm is a lot more specific, provides a lot more direction, and is a lot more inclusive in terms of diagnoses and some of the masqueraders.”
Dr. Mah says that the ASCRS committee has been very conscious of the other groups’ efforts. “We started this process a couple of years ago, about the same time as the DEWS II group,” he explains. “We have members who are part of the same committees and groups as DEWS II and CEDARS. So of course we wanted to make sure we were not duplicating or taking information from the other groups. We wanted to make sure ours would be a unique algorithm. In fact, we delayed our algorithm so that we could ensure that we weren’t duplicating what the Tear Film and Ocular Surface group was doing.”
Laying It Out, Step by Step
Dr. Mah notes that it’s common practice to divide treatment algorithms by levels of severity. “I’m co-chair of the committee working on AAO’s revised Preferred Practice Pattern for cornea, and we do divide our recommendations into mild, moderate and severe disease,” he says. “However, the ASCRS algorithm for dry-eye management is divided by diagnosis first. Omitting this from the treatment algorithm assumes the clinician is making the correct diagnosis, which may not be the case, given all of the diagnostic challenges involved in managing dry eye.
“As in our treatment algorithm,” he continues, “our recommendations for diagnosis are laid out in a step-by-step manner. If this test is positive and that test is negative, that means that the diagnosis is in this direction; and with this diagnosis, the next step is testing for X, Y or Z. In fact, we’ve designed the diagnostic algorithm so that it can be hung up in an eye specialist’s exam lane.”
Dr. Mah says the committee has worked to incorporate all of the tests that are currently available into their diagnostic algorithm. “We want to help clinicians make sense of all of the different point-of-care tests that are out there, and provide guidance on how to incorporate them logically and inclusively,” he says. “For example, the algorithm includes using a questionnaire; testing for osmolarity and/or inflammation—specifically MMP-9—and looking at tear-film interferometry. So it’s not a question of ‘Should I buy this or that test?’ It’s, ‘If I have access to two or three tests, how do I incorporate them to make sense of the information I’m getting to try to come up with a cogent thought process as far as the diagnosis?’
“Ultimately, we hope this will become an online algorithm that will allow you to input whatever testing information you have, whether you’re using one test, multiple tests or no tests,” he says. “The online algorithm will then provide a tentative list of diagnoses. Such an online system could be similar to the current ASCRS refractive surgery website, where you put in the information that you have and whatever calculations you’ve completed, and it comes up with some options for you. Obviously this would grow and develop to incorporate new tests as they appear, and to reflect the latest medical literature.
“Once you have a diagnosis, then our treatment algorithm takes over,” he adds. “Depending on the diagnosis, we describe various treatments that can be used to manage, for example, meibomian gland dysfunction or aqueous deficiency, or a combination of the two, or bacterial conjunctivitis, or adenoviral conjunctivitis or allergic conjunctivitis.”
Keeping Things in Perspective
Dr. Mah stresses that the committee’s goal was to make its algorithm(s) clinically useful. “All the dry-eye management algorithms have benefits,” he says. “I think this is currently a very confusing area, because we have a lot of information, but there’s still a lot of information that’s lacking. Ocular surface disease is a huge, diverse area, yet we’re trying to narrow everything down to one diagnosis.
“I believe that as we get more information things will be better elucidated, but in the meantime, anything we can do to make things better for clinicians and their patients is a step in the right direction,” he continues. “Our focus was on making sure that our algorithm is clinically useful in the everyday interaction between clinicians and patients. However, I think there’s merit and value to all three algorithms. I don’t think there’s supposed to be a winner or loser, or one that gets discarded. They should all be helpful to clinicians.”
Looking at dry-eye management from a historical perspective, Dr. Mah says we’re still early on in the grand scheme of things. “The traditional ways of approaching dry eye still have value,” he says. “It’s still important to look at conjunctival and corneal staining with fluorescein and lissamine green; it’s still very important to do tear-film breakup time; it’s still important to look at the meniscus and the meibum that’s being expressed from the meibomian glands. None of the new tests or treatment approaches are so groundbreaking that we should discard what we’ve been doing all along.
“I hope that this year’s focus on dry-eye management algorithms will help to increase clinicians’ awareness and stimulate discussion,” he concludes. “Dry eyes and ocular surface disease impact the majority of our patients. If these algorithms increase awareness and help clinicians understand dry-eye disease better, that will translate into better patient care. Even with all of the information about dry eye that’s been disseminated over the past couple of years, there are still many doctors who aren’t really thinking about it. If we can get everybody to look at it and not dismiss it as something just for the cornea specialist or dry-eye specialist, that will be a big step forward.” REVIEW
Dr. Milner has financial interests with Allergan, Shire, Bausch + Lomb, TearScience, Aldeyra Therapeutics, Eleven Biotherapeutics, Kala Pharmaceuticals, and Refocus Group. He’s a speaker and consultant for Allergan, Shire, TearScience and Sun Pharmaceuticals and owns stock in RPS (Rapid Pathogen Screening). Dr. Mah is a consultant for TearLab, Allergan and Shire. Dr. Nelson is conducting research for Santen Pharmaceuticals and is on the medical advisory board for TearSolutions.
1. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. The Ocular Surface 2017;15;3;575-628.
2. Milner MS, Beckman KA, Luchs JI, et al. Dysfunctional tear syndrome: Dry eye disease and associated tear film disorders - new strategies for diagnosis and treatment. Curr Opin Ophthalmol 2017;27:Suppl 1:3-47.



