Dry-eye disease is estimated to affect more than 7 million Americans, and the prevalence of dry eye increases with age. Additionally, cataract surgery has been found to exacerbate pre-existing dry eye and to induce dry eye in patients with healthy corneas. This postoperative dry eye can negatively affect visual outcomes and visual recovery time.
"Because cataract surgery is incisional and because most cataract patients are older, there is almost always going to be a general worsening of dry eye after cataract surgery," says Eric Donnenfeld, MD, who is in private practice at Ophthalmic Consultants of Long Island in
Preop Steps
Often, when patients present with cataracts, surgeons are so focused on planning for the surgical procedure that they overlook dry eye symptoms. "As cataract surgeons, we may successfully remove the cataract and then be surprised when patients are not satisfied with the result. Many patients complain that their eyes are still stinging and burning. It is important to preoperatively assess patients for concurrent problems, especially dry eye. If they have moderate to severe dry eye, the dry eye needs to be addressed preoperatively," says Carlos Buznego, MD, who is in private practice at the Center for Excellence in Eye Care, in
William Trattler, MD, in practice at the same center, agrees. He typically uses Restasis (cyclosporine ophthalmic emulsion 0.05%) and punctal plugs during the preoperative period in patients with pre-existing dry eye. "It doesn't take long to see an improvement," he says. "Typically, I see a nice improvement on the ocular surface after a week or two of treatment. It is important to get significant dry eye under control before you proceed with surgery because it can potentially affect your IOL calculations."
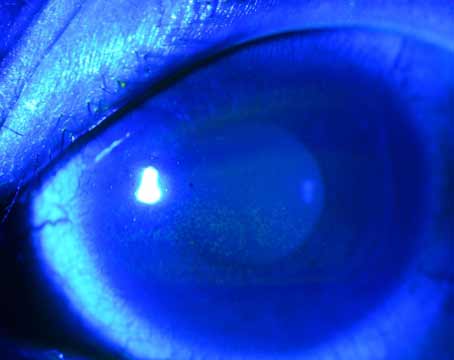
Dr. Buznego routinely assesses cataract surgery patients for dry eye during the history and slit-lamp exam. He notes that dyes such as fluorescein, lissamine green or rose bengal can be used to identify more subtle cases of ocular irritation. "If there is any doubt about the diagnosis, Schirmer testing may be helpful," he says. "We should gear therapy toward the level of dry eye. For moderate to severe dry eye, the recommended treatment is nonpreserved artificial tears, topical cyclosporine A, and, occasionally, topical steroid drops to get the corneal epithelium in the best possible shape before we proceed with cataract surgery. For mild dry eye, we may just go with lubricating drops."
Dr. Donnenfeld aims therapy at treating the underlying condition. For patients with meibomian gland dysfunction and blepharitis, he uses hot compresses, lid hygiene and oral nutritional supplements, such as flaxseed oil and fish oils. For patients with dry eye due to aqueous deficiency, he uses artificial tears in combination with loteprednol four times a day with Restasis over a two-week period. "I taper off loteprednol after two weeks and continue Restasis indefinitely until after the cataract surgery," he says. "I like to start this therapy two weeks before cataract surgery, but optimally four weeks before surgery. I then continue it postoperatively until the ocular surface is superb. These treatment options can also be expanded. Punctal plugs can play a role, and, sometimes, more aggressive therapy such as oral doxycycline is necessary."
Postop Symptoms
Even patients with no history of dry eye commonly experience dry eye after surgery. A recent study conducted by Cal Roberts, MD, and Eleanor Elie, RPN, found that a clinically significant proportion of patients report experiencing at least some dry eye symptoms after cataract surgery.1 This randomized, observer-masked study included 30 women with a mean age of 72.7 years (range: 61 to 86 years). Fifteen patients received topical cyclosporine twice daily for one month before and for one month after cataract surgery. The other 15 patients received its vehicle.
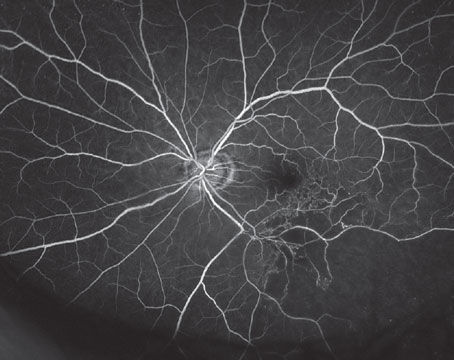
Patients were examined preoperatively and at one week and one month postoperatively. At all study visits, tear breakup time was assessed after instillation of fluorescein drops. Additionally, at all study visits, patients completed a six-item dry-eye symptom questionnaire to evaluate the impact of dry eye symptoms on their daily lives.
At one month after surgery, the most frequently reported symptoms in the vehicle-treated patients were as follows: 87 percent needed to use artificial tears at least once daily; 80 percent experienced dry eyes at least occasionally; 73 percent reported a foreign body sensation at least occasionally; 53 percent reported a burning sensation in the eye at least occasionally; 53 percent reported sticking of the eyelids in the morning at least occasionally; and 47 percent reported blurry vision at least once per day. The proportion of vehicle-treated patients reporting dry eye symptoms increased after cataract surgery.
In comparison, treatment with cyclosporine appeared to increase the proportion of patients who "never" had dry eye symptoms after cataract surgery. Fifty-three percent of the cyclosporine-treated patients reported no need for artificial tears one month after surgery. Additionally, a greater proportion of cyclosporine-treated patients reported "never" or "not usually" having dryness, burning, morning eyelid sticking, and blurry vision compared with vehicle-treated patients. Cyclosporine also appeared to reduce the incidence of severe symptoms.
Tear breakup time improved during the month after surgery in both treatment groups. According to the authors, "These results are consistent with cataract surgery either inducing dry eye or exacerbating pre-existing dry eye in certain patients."
Dry-eye symptoms after surgery can negatively affect visual recovery and outcomes. "Visual recovery is obviously going to be faster with a nice healthy smooth cornea as opposed to a dry cornea with epithelial surface irregularities and tear film issues," Dr. Buznego says. "We are always striving to improve vision and visual recovery. If we are solely concentrating on the technical aspects of surgery, and we are not really paying attention to some of the details, such as dry eye disease and corneal irregularities, we are not going to have successful outcomes."
Dr. Donnenfeld notes that many patients who have undergone cataract surgery complain of vision fluctuation throughout the day. "Visual fluctuation is one of the most important diagnostic symptoms of ocular surface disease. When a patient presents with vision fluctuation, you should evaluate his tear film rather than evaluating the cataract surgery," he says.
Presbyopia-Correcting IOLs
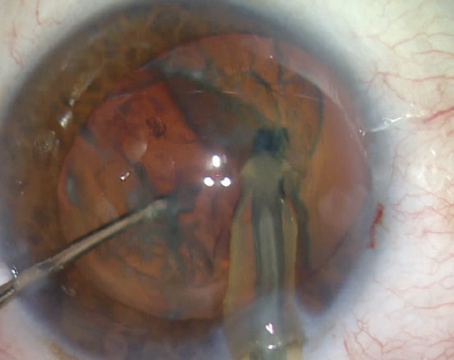
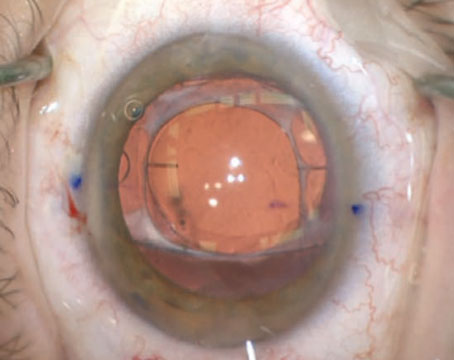
Dry-eye symptoms can be a particular problem for patients with multifocal intraocular lenses. "These patients are paying additional amounts for cataract surgery and are therefore expecting a smoother visual recovery and a better visual result," says Dr. Buznego. "When patients do not achieve the expected outcomes with these lenses, surgeons sometimes blame it on the brand of lens. My feeling is that one of the most unrecognized causes of patient dissatisfaction following presbyopic IOL surgery is dry eye syndrome."
Dr. Donnenfeld agrees. He and his colleagues recently conducted a study and found that the preoperative and postoperative use of cyclosporine A 0.05% significantly improved visual outcomes in patients implanted with the ReZoom multifocal IOL. (Donnenfeld E, et al. IOVS 2007;48:ARVO E-Abstract 1066). This multicenter, randomized, masked, prospective clinical trial evaluated the effect of cyclosporine A 0.05% compared with an artificial tear on the quality of vision in 40 eyes of 20 patients bilaterally implanted with the ReZoom IOL (AMO). Study medications were instilled twice daily for one month preoperatively and for two months postoperatively in one eye. The second eye randomly received the artificial tear. Two months postoperatively, uncorrected visual acuity, best-corrected visual acuity, mesopic and photopic contrast sensitivity under high-contrast and low-contrast illumination, and topography were assessed. The study found that the eyes that received the cyclosporine A had significantly improved mesopic and photopic contrast sensitivity compared with eyes not receiving cyclosporine A, and there was a trend toward improved uncorrected and best-corrected visual acuity in the eyes treated with cyclosporine A.
"In this study, we not only found an improvement in contrast sensitivity in patients receiving ReZoom multifocal IOLs, but we also found an improvement in Snellen visual acuity," says Dr. Donnenfeld. "The difference in quality of vision may be the difference between a happy patient and an unhappy patient. For this reason, we are recommending that Restasis be used in patients over 60 who are receiving multifocal IOLs."
1. Roberts CW, Elie ER. Dry eye symptoms following cataract surgery. Insight 2007;32(1):14-23.