As David Huang, MD, PhD, celebrates the 30th birthday of the technological brainchild he helped create—optical coherence tomography—he’s also pleased with the progress of its 6-year-old sibling, OCT angiography, which is coming of age in retinal care and blazing a trail of baby steps in the glaucoma space. “It’s intriguing,” says Dr. Huang, a professor of ophthalmology at the Oregon Health & Sciences University in Portland. Also a professor of biomedical engineering at the OHSU School of Medicine, Dr. Huang pauses before reflecting further on the potential for helping his colleagues use this emerging erythrocyte-counting scanning modality to diagnose glaucoma and monitor progression. “We still have a fair amount of progress to make on this, but it’s already giving us meaningful new parameters to observe and measure for our glaucoma patients.”
The question in many glaucoma experts’ minds is when OCT-plus-angiography, or OCTA, will come of age.
Still not widely used, even in many academic settings, the technology is short on supporting literature and lacks the robust normative data that’s helped make the use of OCT an unofficial standard of care for both glaucoma and retinal specialists. Nonetheless, researchers working on limited OCTA studies have recently recorded two landmark findings on how the technology may someday be used in everyday practice as a tool that:
• could show that primary open angle glaucoma is not just caused by increased intraocular pressure, potentially opening a window for alternative treatments; 1 and
• may track progression in advanced primary open angle glaucoma in meaningful ways after OCT stops providing meaningful measurements of overly thinned retinal nerve fiber layer.2
In this report, researchers and glaucoma specialists talk about the promising future of OCTA, its current limitations and how much impact the technology could eventually have on the glaucoma care.
What is OCTA?
OCTA systems operate on one of two platforms: a spectral-domain system with an ~840-nm wavelength, used most often in glaucoma care;3 or a swept-source OCTA with a longer ~1,050-nm wavelength that may allow for a deeper penetration into the choroid, a benefit that’s mostly used in retinal care.4 In 1990, Dr. Huang introduced OCT under the direction of James G. Fujimoto, PhD, his professor at the Massachusetts Institute of Technology. Their efforts led to a 1991 groundbreaking paper in which Dr. Huang and co-authors described the power and potential of this “noninvasive cross-sectional imaging in biological systems.”5
Now that the use of OCT has evolved into a standard of care in the glaucoma and retina arenas, OCTA is gradually making a place for itself as as an add-on to OCT. The technology is currently available from OptoVue (through AngioVue, and on its Avanti widefield OCT platform), Zeiss (Cirrus HD-OCT with AngioPlex OCT), Heidelberg Engineering (Spectralis OCT Angiography Module) and Topcon, whose device (SS-OCT Angio powered by OCTARA) is still awaiting FDA approval.
The benefit of OCTA is that it compares sequential, cross-sectional OCT image frames at the same position, looking for signal fluctuations that indicate blood flow, according to Dr. Huang. He notes that the device uses this function to detect blood flow down to the capillary level, relying on a non-invasive scanning technique that mimics the invasive use of fluorescein angiography.
 |
How OCTA Helps in Glaucoma
OCT angiography has been commercially available since September of 2015, five years after Dr. Huang’s team began to help develop and test the technology. This has been made possible in recent years by the availability of faster OCT platforms, which allow for rapid, multiple scans of the same places in the eye, according to Dr. Huang. “It’s worked amazingly well,” he notes. “You can really get blood vessel contrast down to the capillary level. Our contribution has been to develop a very efficient method of detecting flow by comparing OCT signals, establishing a correlation that can increase signal-to-noise ratio, resulting in a flow detection capability that has made it possible to introduce OCT angiography for use by clinicians.”
Dr. Huang says his team studied a number of areas of blood circulation in the retina and optic nerve head before finalizing the design. “Basically, we’ve established OCT angiography in the same location as the structured OCT image,” he notes. “What we find in glaucoma is that the capillary density is decreased in the optic nerve head and peripapillary nerve fiber layer. We see RNFL thinning and, in the same area, reduced capillary density.”
In the macula, he continues, reduced vessel density is present in the superficial vascular complex, a combination of the nerve fiber layer plexus and the ganglion nerve fiber layer plexus. “This is the same structure that’s damaged by glaucoma,” he says.6
 |
Beyond IOP?
Robert N. Weinreb, MD, chair and distinguished professor of ophthalmology and bioengineering, and director of the Shiley Eye Institute at UC San Diego, says he and other researchers are studying where OCT fits into our current paradigm of glaucoma management.
One study, published in Ophthalmology this past January, included 139 eyes (23 healthy eyes, 36 preperimetric glaucoma eyes, and 80 POAG eyes) of 94 patients who were seen over at least three visits.1 Vessel density measured by OCTA and structural thickness measured by OCT were evaluated on the same 3-mm2 GCC scan slab. Evaluation of associations between rates of thickness and vessel density showed significant rates of GCC thinning and macular vessel density decreases in all diagnostic groups, including comparable rates in healthy eyes and preperimetric glaucoma eyes. However, in the POAG group, more than two-thirds of the eyes showed faster macular vessel density decrease than GCC thinning.
The faster macular vessel density decrease rate was associated with worse glaucoma severity. IOP during follow-up significantly affected the rate of GCC thinning in all groups (all p<0.05) but notably showed no association with the rate of macular vessel density decrease. The researchers’ conclusion was that macular vessel density is useful for evaluating glaucoma progression, particularly in more advanced disease.
What was left unsaid by the researchers, and remains open for exploration, is whether changes in macular vessel density in some individuals may reflect causes of glaucoma that are independent of IOP. “If confirmed in studies of longer duration and larger size, OCTA measurements may also be useful for evaluating glaucoma progression caused by factors other than intraocular pressure,” says Dr. Weinreb. Noting that the duration of this study, up to 2.6 years in the POAG group, was longer than earlier studies, he says it provides a good foundation for hypothesis development. “Currently, intraocular pressure is the best-studied factor in what causes glaucoma,” Dr. Weinreb notes. “There have not been accurate, reproducible, non-invasive technologies that can readily can assess vascular impairment or ischemia in the optic nerve. However, sensitive detection and monitoring of vessel density with OCTA might provide information about whether, in any individual, the IOP is the primary cause of damage, and whether loss of vessel density is merely a consequence of loss of neurovascular tissue. Alternatively, it might show whether real or observable loss of vessel density can lead to loss of neuronal tissue in some patients. Such an understanding might provide a basis for the development of new therapies, including those that protect the optic nerve independent of IOP.”
Grace Richter, MD, MPH, assistant professor of clinical ophthalmology and acting director of the glaucoma service and glaucoma fellowship program at the University of Southern California’s Roski Eye Institute, is also eager to find out to what extent vascular abnormalities may contribute to glaucoma. “Until now, we thought only intraocular pressure could cause the disease,” she says. “But OCTA may help us learn more about normal-tension glaucoma. If there is non-pressure-related therapy that could potentially improve blood flow and prevent optic nerve damage, OCTA would be helpful in understanding the utility of those therapies and the extent to which vascular abnormalities contribute to glaucomatous damage.”
 |
Late-stage Monitoring with OCTA
Another study involving Dr. Weinreb and his fellow researchers supports the use of OCTA for monitoring the late stages of glaucoma.2 The study investigated the measurement floors and dynamic ranges of OCT and OCTA when monitoring glaucoma in 509 eyes of 38 healthy participants, 63 glaucoma suspects and 193 glaucoma patients. The relative vessel density measured by OCTA was compared to the circumpapillary retinal nerve fiber thickness, measured by OCT.
“In late-stage glaucoma, particularly when visual field mean deviations are very poor, worse than 14 decibels, OCTA’s measurement of perifoveal vessel density is promising for monitoring advanced progression, because it doesn’t have what’s known as a detectable measurement floor,” says Dr. Weinreb. “With OCT structural measurements, change is observed only to a certain level in advanced disease, at this detectable measurement floor. However, the floor is lower for OCTA. Using OCTA, one often can detect change in severe disease that can’t be detected with structural OCT.”
Does this mean that OCTA will always be better than structural OCT for detecting progression in advanced disease?
 |
“Not necessarily,” says Dr. Weinreb. “One possible limitation is the number of steps for detecting change. With structural change, you have more steps within the dynamic range than with OCTA. Only with longer duration studies and studies with greater numbers of patients will we know. With our current information, however, OCTA does appear to be a promising tool for detecting disease-related change in glaucomatous eyes with advanced disease. In contrast, we believe that, with our current technology, structural OCT, rather than OCTA measurements, may be more sensitive for detecting change in early glaucoma.”
Even though most glaucoma specialists or other clinicians aren’t routinely using OCTA for glaucoma management, Dr. Weinreb is guardedly optimistic on its future. “We’re excited by the technology,” he says. “Not only does it have application to glaucoma care, we believe it also could lead to novel therapies for glaucoma.”
 |
Monitoring Moderate Glaucoma?
Dr. Huang of OHSU also sees the potential for the use of OCTA for monitoring progression in moderate disease, not just the severe cases recent research seems to support. The nerve fiber layer also thins so much in moderate cases that OCT can barely help perceive further change, he points out.
“You can find measurements getting as low as 40 to 50 percent of the original reduced thickness that was identified in the patient,” observes Dr. Huang. “The decreases become very small, and it’s very difficult to gauge progression of the disease once the patient develops even moderate disease. On the other hand, with OCTA, the capillary density seems to continue to drop in moderate and severe glaucoma. Of course, we already have visual fields to measures changes at this point, but visual fields have relatively poor test-to-test reproducibility. It can take as many as seven to nine visual field tests to really get a significant progression rate measurement.”
OCTA’s greater precision in moderate and severe disease leads to the potential benefit of being able to detect progression earlier in these moderate and severe cases, says Dr. Huang.
“If you go from having 5 percent of nerve fiber layer left down to 3 percent, that’s a huge change in your visual sensitivity, but in terms of thickness, that difference is very small and difficult to measure,” he says. “With capillary density, you can get the reproducibility down to 3 percent. The meaningful contrast of the capillaries might be very useful to rely on in these moderate to severe cases, whereas visual fields, as I mentioned, can be terrible, quite noisy, in these cases. The capillary density we measure with OCT angiography is in the layer of the plexus that we’re interested in, providing diagnostic usefulness. You get more repeatable measurements measured off of the capillary density, compared to the visual field sensitivity.”7
Monitoring Treatment
Dr. Huang says OCTA can also help determine how well a treatment has worked—and can even show that some effects of glaucomatous damage can be reversible. “We’ve found that, in fact, there can be a tremendous pressure-lowering effect from trabeculectomy,” he says. “We see visual fields that show that the treatment has proven effective. This finding tells us that that the ganglion cells were not really functioning; they were sick. They were not functioning because of that high pressure. But once that pressure was removed, they started functioning better. Of course, you would never find a neurologic fiber layer getting thicker following treatment. The structure doesn’t change once the damage has been done. But the capillary density, we found, can actually improve after the trabeculectomy. (See Figure 1.)
“OCT angiography is also different from structural OCT in this respect: You can measure improvement in function,” Dr. Huang continues. “As the function improvements occur, you can actually see the capillaries coming back. The metabolism recovers after trabeculectomy.
“Additionally, if you have a neuroprotective drug or aother drug that might improve ganglion cell function or ensure its survival, you might have a direct effect on IOP and it would be hard to measure with OCT if that drug was effective,” he says. But this is one way to measure if such a treatment is working. This is because the perfusion has been increased. We’re able to see this because this method of measuring change is very responsive to short-term changes, based on blood flow.”
 |
Not Ready for Prime Time?
Sarah H. Van Tassel, MD, co-director of the glaucoma service and director of the glaucoma fellowship at Weill Cornell Medicine in New York City, says she has not yet ventured into the OCTA domain for routine clinical care of her glaucoma patients.
“OCTA is still relatively new,” she notes. “It’s a noninvasive modality that has the advantage of offering qualitative and quantitative assessments of the vasculature within the retina and optic nerve. I think that it’s an incredibly interesting time for research related to OCTA. I wouldn’t want my lack of interest in doing OCTA clinically to be construed as a lack of interest in the OCTA research enterprise, because I think it’s rapidly evolving. OCTA might prove to be advantageous in important areas. Evidence suggests that the measurement floor is lower in OCTA than in OCT and that it may be valuable for identifying patients who are at risk for rapid progression or who are rapidly progressing before we realize it when we’re using visual fields or OCT. So I’m definitely excited about it.”
Despite Dr. Van Tassel’s enthusiasm for OCTA’s potential, she believes more development of the technology is needed to optimally enhance and support evaluation of the glaucomatous optic nerve and the glaucoma patient. “What we really need are easy-to-use, commercially available algorithms that are compared to normative data sets, enabling us to know what’s normal and abnormal and what constitutes rapid change,” she says. “To date, those kinds of clinical-support tools are not readily available when using OCTA.”
Besides the need to acquire more normative data, Dr. Van Tassel says imaging artifacts associated with OCTA present a challenge. This is more so in OCTA than in OCT, according to the literature.8,9
“We will be forced to very closely interrogate the images for artifacts in OCTA, because artifact is one of the limitations and challenges associated with OCTA images,” she says. “The retina literature has really gotten into the weeds on that topic.10 A lot of reports point to patient motility and eye motility creating image artifact with OCTA, and challenges in trying to exactly duplicate the layer of the vasculature you’re capturing each time you scan. It may be challenging to compare prior scans and future scans with normative data.”
 |
For the time being, Dr. Van Tassel relies on OCT, among other technologies, but she recommends a careful approach. When applying OCT to glaucoma care, for example, she notes that ophthalmologists in general tend to focus too much on the suggestive red and green colors included in scans. “Often, doctors aren’t attuned to the nuances of scan results and to making sure the actual data and image acquisition are of sufficiently high enough quality to support clinical decision-making,” she notes. “Remember that green means that a particular measurement is within the 90-percent range of normal compared to the eyes in the normative database. But the normative databases aren’t perfect.” She emphasizes that patients can have numeric data that fall in the normal range compared to the normative database and still have glaucoma. Conversely, patients can have numerical data outside the normal range but not have glaucoma.
Ophthalmologists are “good pattern recognizers,” she continues. “I think that, because we like patterns, the colors on the maps become, in some respects, crutches, rather than support tools, which is really what OCT and OCTA are meant to be.
“Quantifying progression is really difficult. How do you distinguish test-retest variability?” she continues. “How do you know if a patient is actually getting worse? In contrast to using visual field criteria, you really have no agreed-upon criteria for whether actual structural progression resulting from glaucoma is occurring. The guided progression analysis functionality of OCT is one tool that can be helpful.”
Full Steam Ahead
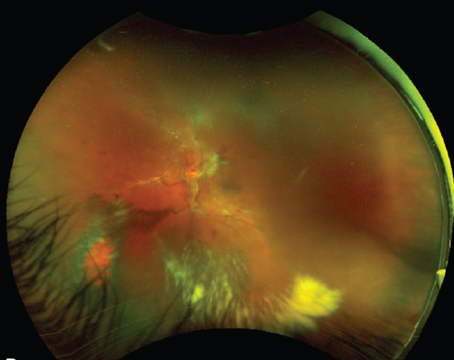
Dr. Richter of the USC Roski Eye Institute has no reservations about using OCTA at this point. She performs one of these scans on virtually all of her patients after dilating them to produce better images, one or two times a year. She prefers to use 6 x 6-mm scans, the largest available, because larger optic nerve heads may not allow visualization of the surrounding peripapillary retina, an important component of an OCTA scan. She typically encounters two main types of qualitative findings: focal wedge defects and diffuse loss in advanced disease. (Figure 2.)
“There are cases when OCT is good enough for determining if a patient has glaucoma,” she admits. “But I still try do an OCTA on every patient because I feel that, over time, it will be helpful longitudinally as I follow patients. We still don’t know if that will be true at this point. I would say for the majority of cases, OCT is fine for making a diagnosis, but I’ve had a decent number of patients in which I’ve made the diagnosis of glaucoma based on OCTA, which is one of the reasons I try to get an OCTA scan on as many patients as I can. But keep in mind that I’m in an academic setting and this is my area of research, unlike many other ophthalmologists’ settings and potential areas of research.”
Some of Dr. Richter’s successes in using OCTA for patient care have included the following:
• A 70-year-old Caucasian woman, presenting for a second opinion on possible normal-tension glaucoma, had non-specific findings on OCT, and Humphrey Visual Field findings suggestive of cecocentral defects OU. OCTA showed obvious papillomacular bundle defects suggestive of metabolic optic neuropathy, rather than glaucoma (Figure 3).
• A 68-year-old African-American woman had open angles, IOP of 17 mmHg OD and 18 mmHg OS, normal central corneal thickness, a family history of POAG and full visual fields. She presented with a superior disc hemorrhage, but OCT showed no local damage. OCTA revealed an obvious superotemporal wedge defect in the area of the disc hemorrhage (Figure 4).
• A 31-year-old male presented with POAG and baseline IOPs of 14 mmHg OD and 15 mmHg OS. OCT showed left eye inferior thinning but no signs of the superior nerve damage expected from his inferior visual field defect in that eye. OCTA showed a superotemporal defect in the left eye that correlated with the inferior nasal step on the visual field. This was completely missed on the OCT scan (Figure 5).
• A 70-year-old Caucasian male had normal visual fields, open angles, an IOP of 12 mmHg, thin corneas and a nonspecific family history of glaucoma. OCTA showed an obvious wedge defect in the right eye, leading to a diagnosis of preperimetric POAG. Only a hint of the defect, non-diagnostic, had been found on the RNFL thickness map OD (Figure 6).
Better Study Needed
Despite her success when using OCTA on select patients, Dr. Richter notes that literature supporting the use of OCTA in practice needs to go beyond existing studies that focus on diagnostic accuracy.
“A lot of the literature supporting the use of OCTA in glaucoma has been focused on vessel density,” she says. “For OCT, the literature often talks about the diagnostic accuracy of mean circumpapillary RNFL thickness. But most glaucoma specialists or general ophthalmologists who use OCT in glaucoma look beyond the summary mean of the RNFL thickness. There’s a lot more data available from OCT. For example, looking in the focal quadrants and sectors, or looking at the RNFL thickness maps, can help with following glaucoma patients over time.”
She believes that OCTA, similarly, can offer a lot more than diagnostic accuracy—more than a single summary parameter like vessel density of an OCTA image. “OCTA has actually helped me the most in the early diagnosis of glaucoma,” she notes. “It has sometimes helped me with the question of whether a patient has glaucoma or not. OCTA can really help you identify focal characteristic effects on the microvasculature, which can be convincing enough to support a diagnosis of glaucoma. These are sometimes not so easy to see on OCT or during the clinical exam.”
Broader Applications
Regarding whether general ophthalmologists should consider using OCTA, Dr. Richter says: “I think each practice has to weigh the pros and cons of acquiring OCT angiography. It provides an add-on to a lot of the current OCT devices and it’s useful for a lot of retinal diseases. So I think most comprehensive ophthalmologists could find OCTA very helpful in numerous ways, not just when caring for glaucoma. Whether the cost is worth it depends on your patient demographics and what sort of practice you operate. If you want to practice with cutting-edge technology and really provide the highest level of technology for your patients, then OCTA will allow you to find the more nuanced manifestations of early glaucoma, once you learn how to detect those changes. At the same time, we’re still learning a lot about of OCTA. So it may make sense to wait. For a more resource-limited setting, this technology might not be the priority. But it definitely does help in patient care.”
A lot of glaucoma specialists say they aren’t using OCTA at this point, but most expect that to change as more published literature supports the benefits of its use. OCT has existed for 30 years, they argue, so the literature supporting its use in detecting glaucoma and monitoring patients for progression is much more firmly established. “As we learn more about the qualitative benefits of OCTA, it will become more widely used,” says Dr. Richter. “For example, for longitudinal studies to determine if OCTA can be helpful in detecting progression, there’s very little literature because that takes time and we’re very early on in the use of this technology.”
For her part, Dr. Richter is making efforts to report on the qualitative findings of OCTA. “Hopefully it will be more practically-focused on how OCTA can be used to improve our care of patients,” she says. “There are benefits you can get from OCTA that are not available in OCT. This is not just a matter of looking at a summary parameter such as the vessel density. You can also really look at the image qualitatively. I find it very helpful in new patients. I can find focal wedge defects in the microvasculature of the RNFL, and I’ve had several instances in which I saw a wedge defect that was consistent with glaucoma but that I really couldn’t see in a clinical exam or on OCT.”
Limitations of OCTA
Dr. Richter, acknowledging the limitations of motion artifact and sensitivity to media opacity when using OCTA, follows simple rules to prevent problems. “I avoid OCTA in a patient who can’t sit comfortably enough for the length of the OCTA scan, which is approximately 10 to 20 seconds,” she says. “The patient may be in a wheelchair, be very elderly or have a movement disorder. I also avoid OCTA if the patient has media opacities, such as a very prominent floater centrally, a cornea opacity or a dense cataract, for example.”
Dr. Huang, whose decades of research and development work helped establish the giant footprint of OCT in glaucoma and retinal care, also acknowledges the shortcomings of OCTA. But he believes these shortcoming will be overcome in time.
“I think it will be a matter of the machines getting better,” he says. “The software supporting the analytics will continue to get better, enabling you to be more sure of diagnosis and management decisions. Scan time will need to be efficient, and the imaging must continue to improve. And as so many doctors note, the advantages of using OCT angiography will also obviously need to be demonstrated in clinical trials and studies.
“I think, so far, the demonstrated benefits are most compelling for retinal specialists in areas such as neovascular age-related macular degeneration and diabetic retinopathy,” Dr. Huang adds. “You can really use these technologies reliably for these patients by effectively screening them and following their disease course more easily than you could with fluorescein angiography, which is more invasive, more expensive, requires a lot of time and wears on patient tolerance. I think OCT angiography is quite compelling for the retinal specialist, who will be relying on OCT angiography a lot more than fluorescein angiography.”
In the care of glaucoma patients, he continues, both perimeters and OCT units remain the mainstream technologies. “Updating to the use of newer, faster OCT machines will support the use of OCT angiography at some point, if not immediately,” he points out. “I think that would be the time for glaucoma specialists to learn the uses of OCT angiography and, after acquiring the OCT angiography enhancement, start following their patients with this technology. In a few years, the analytics may provide an effective way to follow the patient in terms of monitoring progression and treatment response. Right now, there’s not much of a consensus on OCT angiography in glaucoma. But it’s something that’s easily available, in terms of equipping the OCT machine and providing the scanning patterns. When you do an OCTA scan, you also get a high quality, 3-D structural scan from the OCT, so you can kill two birds with one stone—both the thickness measurement and the perfusion measurement. Using the same machine, you obtain two sets of data that can be used to validate each other. So, overall, I would say this new technology will be more and more beneficial for the practitioner.” REVIEW
Dr. Huang has research grants, patent arrangements and stock ownership interests involving OptoVue. Dr. Weinreb receives research support and instruments for use in his practice and research from Optovue, Zeiss and Heidelberg Engineering. Dr. Richter still uses an OCTA unit donated to her by Zeiss in 2016 but has no relevant financial relationships with any OCTA manufacturer. Dr. Van Tassel reports no relevant financial relationships.
1. Hou H, Moghimi S, Proudfoot JA, et al. Ganglion cell complex thickness and macular vessel density loss in primary open-angle glaucoma. Ophthalmology 2020; Jan 13. [Epub ahead of print]
2. Moghimi S, Bowd C, Zangwill LM, et al. Measurement floors and dynamic ranges of OCT and OCT angiography in glaucoma. Ophthalmology 2019;126:7:980-988.
3. Liu L, Tan O, Ing E. Sectorwise visual field simulation using optical coherence tomographic angiography nerve fiber layer plexus measurements in glaucoma. Am J Ophthalmol 2019; Nov 23. [Epub ahead of print].
4. Povazay B, Hermann B, Unterhuber A, et al. Three-dimensional optical coherence tomography at 1050 nm versus 800 nm in retinal pathologies: Enhanced performance and choroidal penetration in cataract patients. J Biomed Opt 2007;12:041211.
5. Huang D, Swanson EA, Lin CP. Optical coherence tomography. Science 1991;254:5035:1178-81.
6. Takusagawa HL, Liu L, Ma KN, et al. Projection-resolved optical coherence tomography angiography of macular retinal circulation in glaucoma. Ophthalmol 2017;124:11:1589-1599.
7. Liu L, Tan O, Ing E, et al. Sectorwise visual field simulation using optical coherence tomographic angiography nerve fiber layer plexus measurements in glaucoma. Am J Ophthalmol 2020;212:57-68.
8. Francesco Pichi F, David Sarraf D, Morar M. Pearls and pitfalls of optical coherence tomography angiography in the multimodal evaluation of uveitis. J Ophthalmic Inflamm Infect 2017;7:1:20.
9. Moghimi S, Hou H, Rao H, Weinreb R. Optical coherence tomography angiography and glaucoma: A brief review. Asia Pac J Ophthalmol (Phila) 2019; April 4. [Epub ahead of print].
10. Lauermann JL, Woetzel AK, Treder M. Prevalences of segmentation errors and motion artifacts in OCT-angiography differ among retinal diseases. Graefes Arch Clin Exp Ophthalmol 2018;256:10:1807-1816.