 |
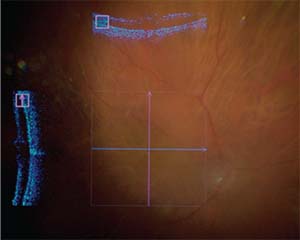
| Figure 1. 3D heads-up display with five observers watching Murtaza Adam, MD, operate. The setup consists of an ICM 5 high-dynamic-range camera connected to an operating microscope and a 4K OLED display placed approximately a meter away from the surgeon. |
The Technology Evolves
In 2008, TrueVision Systems first entered the market with a three-dimensional, heads-up ophthalmic surgical visualization system. Using a high-definition display, a camera connected to a traditional surgical microscope, and passive 3-D glasses, their principal idea was to free the ophthalmic surgeon from the constraints of the operating microscope (Figure 1). Some anterior segment surgeons immediately began using the technology, since heads-up visualization allows for a seamless overlay of preoperative and intraoperative data, such as toric overlays and phacoemulsification metrics.
Sony also entered the market in 2013 with its own version of a 3-D heads-up visualization system for neurosurgery and opththalmology, but its impact upon the vitreoretinal market has been less significant. This is likely due in part to the partnership forged by Alcon and TrueVision in 2016 to create NGENUITY, a visualization platform specifically created for digitally assisted vitreoretinal surgery.
Over the intervening years since the system’s introduction, TrueVision/Alcon have made several improvements to the system, including a fifth-generation, high-dynamic-range 3-D camera, integration of a 55-inch, 4K OLED TV, and much-improved latency (i.e., the perceived delay between when you make an action and when you see it displayed). With any medical innovation, however, all potential advantages over the current paradigm are undermined by questions of clinical utility and economics. Does performing 3-D heads-up vitreoretinal surgery result in better visual outcomes? Will there be a lower complication rate? Will surgery be more efficient, resulting in reduced operative time? Will the surgery be more ergonomically comfortable? In a medical system with limited resources, these are important questions that need to be answered.
A Dearth of Data
At this time, few scientific studies have attempted to answer the questions listed above. In 2015, Claus Eckardt, MD, and Erica Guerreiro Paulo, MD, published the first peer-reviewed study comparing the traditional microscope to the TrueVision 3D heads-up platform.1 The authors prospectively and systematically evaluated the performance of 20 volunteers carrying out various tasks (arranging small objects with forceps, tying sutures, etc.) using a standard operating scope and the TrueVision system. Although the authors found that the resolution of the traditional microscope was twice that of the digital display, they didn’t feel that this was a significant obstacle, and they reported no differences in performance. More than 90 percent of the study participants preferred the ergonomics of the heads-up technique.
In the same publication by Drs. Eckardt and Paulo, a retrospective analysis
 |
| Figure 2. Indocyanine green dye-assisted chromovitrectomy in a patient with proliferative diabetic retinopathy before (top) and after (bottom) activation of a digital filter to enhance visualization of the internal limiting membrane. |
Building upon this work, two additional publications, including one by our group at Wills, more rigorously examined the power of digitial amplification in reducing endoillumination requirements during vitreoretinal surgery.2-3 Both small case series reported safely performing a variety of vitreoretinal cases with endoillumination levels at less than 5 percent of maximum output, a task that would be extremely difficult with a traditional scope.
This limited body of work represents preliminary attempts to demonstrate the potential of 3-D heads-up surgery and identify areas in need of improvement. At Wills Eye Hospital, our investigator-initiated, prospective, randomized, controlled trial is currently under way to explore these same areas of interest. Our study aims to compare detailed intraoperative metrics and postoperative outcomes of patients with macular holes, epiretinal membranes and retinal detachments, randomized to undergo surgery with a traditional operating microscope or the NGENUITY system. Our hope is that other groups will perform similar objective and quantitative analyses to provide a realistic assessment of the system’s ability to affect patient care, and identify ways to maximize its potential.
A Dash of Subjectivity
Our experience with 3D heads-up vitreoretinal surgery over the past year has been largely positive. From a subjective standpoint, after we began using the the NGENUITY system, we’ve found that our support staff has become more engaged and attentive, because anyone wearing passive 3-D glasses in the OR shares the surgeon’s 4K, stereoscopic OLED view. This shared viewing ability has helped many on the OR staff, as well as medical students and residents, to have a better understanding of the methods and goals of surgery. When we use a standard operating microscope, the attending and
 |
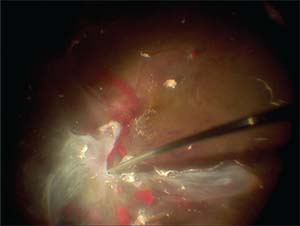
| Figure 3. Intraoperative optical coherence tomography of a small macular hole|following epiretinal membrane and internal limiting membrane peel. The entire case was performed with 5-percent endoillumination to minimize the risk of macular phototoxicity. |
The 3D heads-up platform performs well in macular cases and diabetic tractional detachments. The field of view is broad and stereopsis is excellent, even with high magnification. This allows for wide, confident peeling with excellent peripheral awareness. Additionally, real-time digital filtering can be used to highlight internal limiting staining achieved during chromovitrectomy (Figure 2) and digital gain manipulation can significantly reduce endoillumination requirements (Figure 3). Integration of intraoperative optical coherence tomography also works seamlessly with the heads-up system and provides high-resolution scans of macular anatomy (Figure 3). In diabetic tractional detachments, the movement of a peripherally detached retina when peeling posterior fibrovascular tissue is easily detected, giving the surgeon more confidence in his or her ability to avoid creating iatrogenic breaks (Figure 4).
Primary and complex retinal detachment repairs are intuitive with the 3-D heads-up platform. However, we’ve encountered occasional issues with decreased peripheral acuity and washed-out images when performing peripheral laser.
The traditional operating scope has the advantage of using the surgeon’s pupils and lens (with associated accommodation) as part of the optical system to balance image exposure and facilitate a clear peripheral examination. With 3-D heads-up surgery, however, the final pathway for light is the high-dynamic-range camera mounted on the operating microscope, which has limits to its exposure
 |
| Figure 4. High resolution maintained with a wide field of view during dissection of preretinal fibrovascular plaques in a patient with a macula-involving diabetic tractional detachment. |
The focus control with our current setup is quite sensitive and refocusing in the middle of a case can be cumbersome. We’ve found that parfocusing at the beginning of all 3-D cases and markedly decreasing the light intensity when performing peripheral laser with scleral depression can help minimize these issues.
Overall, we have found working in the vitreous cavity to feel quite natural and comparable to the standard operating microscope. Digital image latency isn’t an issue when performing vitreoretinal surgery, since movements within the posterior segment are typically slower than maneuvers performed anteriorly. However, when working on the anterior segment, the digital latency becomes more evident and the surgeon’s hands should slightly slow to compensate for this. Also, the field of view of the anterior segment is smaller with the heads-up platform compared to the standard operating microscope. These factors lead to slightly awkward corneal, conjunctival and scleral suturing, especially when working with long sutures.
Looking Ahead
Significant improvements to the latest-generation platform are already on the way, including real-time integration of vitrectomy machine parameters, a streamlined purely digital microscope, the addition of digital filters, and the ability to overlay preoperative and intraoperative data on the surgical field. As each advance in heads-up surgery arrives, however, it’s imperative that we clinicians participate in guiding its evolution to improve outcomes and maximize safety. Our patients are depending on us. REVIEW
Murtaza K. Adam, MD, is a vitreoretinal surgeon at Colorado Retina Associates in Denver. He trained at Wills Eye Hospital for his ophthalmology residency and vitreoretinal surgery fellowship. He has received funding for an investigator-initiated trial related to the NGENUITY 3D heads-up surgical platform from Alcon.
Allen C. Ho, MD, is the director of retina research at Wills Eye Hospital, a surgeon at Mid Atlantic Retina, and a professor of ophthalmology at Thomas Jefferson University, all located in Philadelphia. He has received funding for an investigator-initiated trial related to the NGENUITY 3D heads-up surgical platform from Alcon.
1. Eckardt C, Paulo EB. Heads-up surgery for vitreoretinal procedures: An experimental and clinical study. Retina 2016;36:1:137-47.
2. Adam MK, Thornton S, Regillo CD, Park C, Ho AC, Hsu J. Minimal endoillumination levels and display luminous emittance during three-dimensional heads-up vitreoretinal surgery. Retina Nov 29, 2016. (Epub ahead of print)
3. Kunikata H, Abe T, Nakazawa T. Heads-up macular surgery with a 27-gauge microincision vitrectomy system and minimal illumination. Case Rep Ophthalmol 2016;7:3:265-269.



