Two conditions we deal with frequently are allergic conjunctivitis and dry eye. Each presents with a spectrum of symptomatology and, although treatments are available for both, there is also room for therapeutic improvement. A key area of unmet need is the intersection of these two conditions, with the growing awareness that as the prevalence of each condition rises, many patients experience both ocular allergy and dry eye.
Although population demographics suggest that there is likely to be a high degree of comorbidity between allergy and dry eye, there are few direct studies that address this issue. Two large-cohort, longitudinal studies do provide evidence that these are not simply two separate, independent conditions.1,2 Data from both of these studies indicates that patients who suffer from allergic conjunctivitis are significantly more likely to experience signs and symptoms of dry-eye disease, especially as they reach middle age. Despite their distinct underlying etiologies, both conditions can lead to a chronic state of ocular surface inflammation and discomfort, which can ultimately result in significant visual dysfunction.
|
While atopy continues its relentless march, the increased lifespan and the aging of populations worldwide are contributing to increased dry-eye prevalence. Like ocular allergy, dry eye is a disorder that ranges from a minor inconvenience to a pervasive, life-altering affliction. It is a condition more common in women, and more common in patients over 50.5 Dry eye differs from ocular allergies, however, in that it has an extremely heterogeneous etiology that includes Sjögren’s syndrome, meibomian gland disorders and neural loop disorders that interfere with reflex tearing. Other causes include various dyslipidemias, mucin disorders (including cystic fibrosis), Stevens-Johnson syndrome and the keratitis that can sometimes occur following refractive surgery.5 Environmental factors play a key role in disease presentation, and many such factors (humidity, air flow and visual tasking) can lead to a significant exacerbation of dry-eye symptoms.
Both ocular allergy and dry eye are aggravated by atmospheric pollutants such as ozone, automobile emissions and other byproducts of fossil fuel combustion. Ozone exposure can lead to elevated free radical damage to proteins and other cell constituents on the ocular surface. Other emission compounds can act as antigens, stimulate immune responses to other airborne allergens, or act as direct irritants to the ocular mucus membranes they contact, eliciting both lacrimation and immune responses. This is just one example of the close association between these two ocular disorders; the report of the International Dry-eye Workshop listed allergic conjunctivitis as a key “extrinsic factor” in dry-eye etiology.5 Despite this, there has been little focus on the causal relationships and the potential for overlapping, synergistic therapies for the two conditions, to date.
One aspect of the comorbidity that does seem to be emerging is the reduced seasonality of the combined disorders. Dry-eye patients typically experience more severe symptoms in winter months when humidity is lower and people spend more time indoors.5 The majority of patients with allergies are symptomatic in spring or fall, depending upon the specific allergens to which they respond.3 In contrast, those with both dry eye and allergies are more likely to experience year-round ocular symptoms. This may reflect a greater proportion of patients with perennial allergies, or may simply be due to the combined assault of both conditions on the ocular surface.
Treating the Comorbid Patient
The starting point for therapy of both conditions is likely to include the use of tear substitutes, which can flush allergens from the ocular surface while at the same time replenish a shortage of tear volume. Over-the-counter oral antihistamines might be an option for treating ocular allergies, but some of these come with a particularly troublesome side effect: The relief they provide from allergies is offset by their tendency to exacerbate symptoms of dry eye. A number of studies have shown that oral antihistamines such as loratadine or cetirizine can reduce aqueous tear production and worsen the ocular burning, grittiness and corneal staining in patients who suffer from dry eye.6,7 Another recent study examined tear composition in patients with allergic conjunctivitis, and found that changes resulting from allergies could contribute to tear-film instability.8 Thus it appears that allergies may predispose patients to developing dry-eye disease in a number of ways.
|
Topical corticosteroids such as loteprednol are the last resort for both allergy and dry eye, and when used judiciously these agents can safely break the inflammatory momentum that can result from either of these conditions, whether the condition is in isolation or exists in combination with the other. As long as the duration of steroid therapy is kept within a one- to two-week window the risks of increased intraocular pressure or ocular infection should not become significant. The other therapy used for dry eye, cyclosporine, is a drug with multiple actions that relieves dry eye by enhancing aqueous tear production in approximately 12 to 15 percent of patients.13 Despite this, neither cyclosporine nor any related drug (such as tacrolimus) appears to hold promise as a universal therapy for other ocular inflammatory conditions, including allergy or allergy plus dry eye.
Addressing Unmet Needs
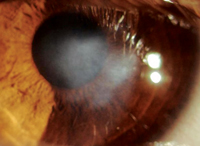
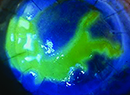
While patients with ocular allergies experience an increased risk for dry eye, the converse is also true: Dry eye can exacerbate allergic signs and symptoms. In a recent paper we described a study that tested effects of exposure to an adverse environment designed to evoke dry eye (using the Ora Controlled Adverse Environment model) on the allergic responses of patients who report suffering from both allergic conjunctivitis and dry eye.14 The adverse environment model caused a significant increase in all measures of acute allergic conjunctivitis. Using confocal microscopy of the patients’ conjunctival surface, we were able to show that these increases in allergic response coincided with increases in the number of inflammatory cells infiltrating the conjunctival vasculature.
Two additional recent studies document damage to the conjunctival and corneal epithelium associated with prolonged allergen exposure10,15 and describe an ocular surface disease that is remarkably similar to that seen in dry eye. Future efforts in therapeutic development may well be designed to treat both conditions by addressing this underlying inflammatory nature.
Historically, the stumbling block for dry-eye drug development has been the apparent disconnect between signs and symptoms of dry-eye disease—dry-eye patients may be asymptomatic with significant corneal pathology, or may suffer from severe burning and ocular discomfort with little or no corneal staining in the clinic. The search for reliable biomarkers for ocular surface pathology is aimed at providing a reliable metric for drug discovery.16 Potential targets for this quest include tear components such as cytokines, mucins, lipids or metalloproteinases. Others include quantifying conjunctival cell types or parameters derived from impression cytology.17 Based on the underlying inflammatory etiology, reliable dry-eye markers should also be valuable in developing treatments for late-phase allergy and for the combination of allergy and dry eye.
As we learn more about the pathology of the ocular surface, the commonalities between tear-film dysfunction and allergic disease become more apparent. While the pathological processes underlying disease in each patient represent a complex amalgam of genetic, molecular and environmental factors, the end result seems to include a robust complement of signs and symptoms common to many patients with dry eye, allergy or both. The shared changes in the ocular surface include structural modifications in the epithelial cells, inflammatory cell infiltration and inflammatory mediator release, as well as alterations in tear constituents. Each of these variations from the normal ocular surface homeostasis contributes to expression of the disease phenotype, and each represents a potential target for therapeutic intervention.
As with all new treatments, the key to addressing the needs of this growing population of patients is establishing viable metrics and efficacy standards for therapeutic development. Ideally, new treatments will provide relief to sufferers of both dry eye and allergy, so symptoms of either disease need not be overlooked. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at the Schepens Eye Research Institute. Dr. McLaughlin is a medical writer at Ora Inc.
1. Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among U.S. women. Am J Ophthalmol 2003;136:318-326.
2. Moss SE, Klein R, Klein BE. Incidence of dry eye in an older population. Arch Ophthalmol 2004;122:369-373.
3. Friedlaender MH. Ocular allergy. Curr Opin Allergy Clin Immunol 2011;11:477-482.
4. Wayne P, Foster S, Connolly J, Bazzaz F, Epstein P. Production of allergenic pollen by ragweed (Ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Annals Allergy Asthma Immunol 2002;88:279-282.
5. Report of the International Dry Eye Workshop (DEWS) Ocul Surf 2007;5:69-204.
6. Ousler GW, Wilcox KA, Gupta G, Abelson MB. An evaluation of the ocular drying effects of two systemic antihistamines: Loratadine and cetirizine hydrochloride. Ann Allergy Asthma Immunol 2004;93:460-4.
7. Wong J, Lan W, Ong LM, Tong L. Non-hormonal systemic medications and dry eye.http://www.ncbi.nlm.nih.gov.ezp-prod1.hul.harvard.edu/pubmed/22023816 Ocul Surf 2011;9:212-26.
8. Li K, Liu X, Chen Z, Huang Q, Wu K. Quantification of tear proteins and sPLA2-IIa alteration in patients with allergic conjunctivitis. Molecular Vision 2010;16:2084-2091.
9. Murota H, El-latif MA, Tamura T, Amano T, Katayama I. Olopatadine hydrochloride improves dermatitis score and inhibits scratch behavior in NC/Nga mice. Int Arch Allergy Immunol 2010;153:2:121-32.
10. Ono SJ, Lane K. Comparison of effects of alcaftadine and olopatadine on conjunctival epithelium and eosinophil recruitment in a murine model of allergic conjunctivitis. Drug Des Devel Ther 2011;5:77-84.
11. Bohets H, McGowan C, Mannens G, Schroeder N, Edwards-Swanson K, Shapiro A. Clinical pharmacology of alcaftadine, a novel antihistamine for the prevention of allergic conjunctivitis. J Ocul Pharmacol Ther 2011;27:2:187-95.
12. Shiraishi Y, Jia Y, Domenico J, Joetham A, Karasuyama H, Takeda K, Gelfand EW. Sequential Engagement of FcεRI on Mast Cells and Basophil Histamine H4 Receptor and FcεRI in Allergic Rhinitis. J Immunol 2013;190:2:539-48.
13. Wilson SE, Perry HD. Long-term resolution of chronic dry eye symptoms and signs after topical cyclosporine treatment. Ophthalmology 2007;114:1:76-9.
14. Gomes PJ, Ousler GW, Welch DL, Smith LM, Coderre J, Abelson MB. Exacerbation of signs and symptoms of allergic conjunctivitis by a controlled adverse environment challenge in subjects with a history of dry eye and ocular allergy. Clin Ophthal 2013;2013:157-165.
15. Contreras-Ruiz L, Schulze U, García-Posadas L, et al. Structural and functional alteration of corneal epithelial barrier under inflammatory conditions. Current Eye Research 2012;37:11:971-81.
16. Enríquez-de-Salamanca A, Bonini S, Calonge M. Molecular and cellular biomarkers in dry eye disease and ocular allergy. Curr Opin Allergy Clin Immunol 2012;12:5:523-33.
17. Barabino S, Montaldo E, Solignani F, Valente C, Mingari MC, Rolando M. Immune response in the conjunctival epithelium of patients with dry eye. Exp Eye Res 2010;91:4:524-9.