The part of the bleb most likely to leak is the thinnest, most avascular area. Many of these blebs are cystic and have thinner and thicker areas; if that’s the case they may leak at the apex of a cyst or the interface between the thick and thin areas. Another vulnerable area is where the bleb is most elevated, because it will be prone to repeated trauma from the eyelid during blinking. This part of the bleb is also more likely to dry out, because the tear film doesn’t coat the elevated area as well as it would if it were flat.
Discovering a Leak
Any time your patient has a thin bleb that you know is at risk for leaking, listen carefully when you ask the patient how the eye is doing. If a leak has developed, the patient may report increased tearing. If it’s leaking enough that the eye has become hypotonous, the patient could report blurred vision. Or, the patient may simply report discomfort.
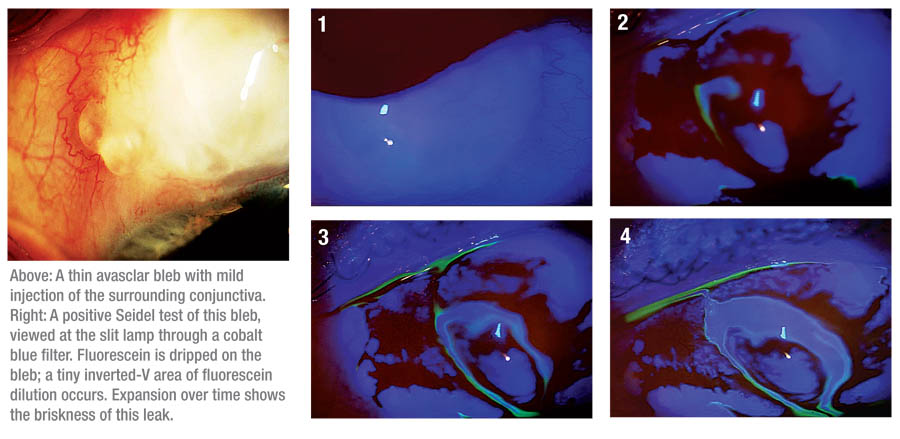 However, it’s possible for the patient to be asymptomatic and still have a leak. For that reason, when I examine any patient with a thin, cystic bleb, I routinely check for a leak by conducting a Seidel test. I wet a fluorescein strip, drip the resulting dye over the bleb and study the bleb with the cobalt blue light at the slit lamp; if there is a leak, aqueous will dilute the dye and you’ll see a clear stream within the fluorescein. (For example, see facing page.)
However, it’s possible for the patient to be asymptomatic and still have a leak. For that reason, when I examine any patient with a thin, cystic bleb, I routinely check for a leak by conducting a Seidel test. I wet a fluorescein strip, drip the resulting dye over the bleb and study the bleb with the cobalt blue light at the slit lamp; if there is a leak, aqueous will dilute the dye and you’ll see a clear stream within the fluorescein. (For example, see facing page.)
In most cases, a bleb leak is not an emergency. So, if I find a leak during a routine exam, I evaluate the signs and symptoms. If the eye isn’t painful, there are no signs of inflammation and the anterior chamber is formed, I’ll start with conservative measures (described below). Of course, if the leak is so brisk that the pressure is low, the eye is uncomfortable and the anterior chamber is shallow or flat, I proceed to surgery.
How you respond to a bleb leak depends, in part, on when the leak occurs. Thus far, I’ve been talking about late-onset bleb leaks—blebs that leak months or years after surgery. These are less problematic because the internal bleb structure is already established. In contrast, when the bleb leaks right after surgery it’s very important to seal it as fast as possible. These leaks usually occur along the suture track, at the limbus or through an inadvertent conjunctival buttonhole. If aqueous does not occupy the subconjunctival space, the requisite separation between the conjunctiva and sclera is absent. Scar tissue will form between these two layers and the bleb will fail within a very short period of time.
 With an acute postoperative bleb leak, I first assess its briskness. If it’s tiny, it may heal spontaneously by withholding or decreasing the dose of topical steroid. Once the leak has sealed, I resume my standard six-times-a-day steroid regimen to minimize inflammation and scarring within the bleb. If the conjunctiva is gaping at the surgical site or a suture has broken, I use an 8-0 Vicryl suture on a taper needle to close it at the slit lamp, since the leak won’t heal on its own. With a leak too brisk to self-seal but not brisk enough to need a suture, I insert a bandage contact lens, confirm that it covers the leak, and then reevaluate the patient in three to five days. If it’s unchanged, I suture it. If it’s leaking less, I reinsert the contact lens for another three days. If the leak persists at the next visit, I place a stitch.
With an acute postoperative bleb leak, I first assess its briskness. If it’s tiny, it may heal spontaneously by withholding or decreasing the dose of topical steroid. Once the leak has sealed, I resume my standard six-times-a-day steroid regimen to minimize inflammation and scarring within the bleb. If the conjunctiva is gaping at the surgical site or a suture has broken, I use an 8-0 Vicryl suture on a taper needle to close it at the slit lamp, since the leak won’t heal on its own. With a leak too brisk to self-seal but not brisk enough to need a suture, I insert a bandage contact lens, confirm that it covers the leak, and then reevaluate the patient in three to five days. If it’s unchanged, I suture it. If it’s leaking less, I reinsert the contact lens for another three days. If the leak persists at the next visit, I place a stitch.
The Conservative Approach
To treat conservatively, I do four things:
1. Suppress aqueous production. Decreasing aqueous production should help to relieve some of the pressure inside the bleb and reduce aqueous flow through the leak, giving it a better chance to heal. This can be accomplished with an aqueous suppressant such as a beta blocker or a carbonic anhydrase inhibitor.
2. Apply an antibiotic. It’s important to use prophylactic antibiotics in this situation to prevent blebitis or endophthalmitis. However, there are different schools of thought about choice of antibiotics. Some prefer a non-epithelial toxic antibiotic (such as a fluoroquinolone), to optimize the chances of the epithelium sealing the leak. Others believe in using a mild irritant, to provoke healing. I usually treat with an antibiotic such as gentamicin ophthalmic solution, which serves two purposes. First, it helps to prevent infection, which is always a concern when a bleb is leaking. Second, gentamicin irritates the surface of the bleb, which may stimulate epithelial cells to proliferate and thus help to seal the leak.
3. Make sure the eye has adequate moisture. Dryness can make the delicate bleb more friable. In addition, the patient is more prone to rub a dry, itchy eye, which is not good whether the bleb is leaking or not. Using artificial tears at least four times a day lubricates the ocular surface; this relieves the itch, makes the bleb more supple and minimizes the trauma to the bleb from blinking.
4. Make sure the eye is protected from trauma and patient eye-rubbing. A bandage contact lens protects the bleb from trauma from the normal eyelid blink. In addition, I may treat these patients as if they have just had surgery and have them sleep with a protective shield over the eye to prevent then from unconsciously rubbing the eye during sleep. LASIK goggles may be a more comfortable alternative for some patients.
When I use conservative management, I’ll typically see the patient five to seven days after my initial in-tervention. At that point, if the leak looks slower but still hasn’t healed, I’ll continue the same strategies or advance the treatment and have him return in a week. For example, if I started with aqueous suppression, gentamicin and artificial tears, I would add a bandage contact lens. If it’s almost healed at the second week, I’ll have the patient come in again a week later.
 |
Many patients respond well to this conservative regimen. I estimate that this is sufficient to heal about one-third of my bleb leaks. Typically, if the leak hasn’t resolved within three or four weeks of this regimen, I repair it surgically. However, even in this situation, it’s not usually necessary to rush. I have a patient right now who is still leaking after a month of conservative management, but he’s not showing any signs of infection or inflammation. So, we won’t do the surgery for another few weeks, because he needs time to manage other concerns in his life first.
On the other hand, if I see any sign of inflammation, or I’m concerned that an early infection is brewing, I’ll start intensive topical antibiotics—-not just gentamicin, but also a fluoroquinolone—every hour. It’s important to treat the infection first, to sterilize the tissue before performing any surgery. Once the eye has quieted down, I’ll perform the repair. (On occasion, the leakage will stop when the infection is controlled.)
Other Nonsurgical Interventions
Aside from medications and bandage contact lenses, there are a few other approaches short of surgery that can sometimes help to restore a bleb to working condition.
One technique that can be effective is needling the bleb to relieve what Peng Khaw, MD, calls a “ring of steel.”2 This is a thick ring of scar tissue that forms at the interface between the cystic bleb tissue and normal conjunctiva. It’s more likely to be seen when a bleb is small and localized. This ring of scar tissue can prevent the aqueous from diffusing underneath the surrounding conjunctiva, building up pressure within the bleb, causing it to thin out and ultimately rupture.
A needle can be used to mechanically break the ring of scar tissue. Before I start, I inject 0.2 cc of a 50:50 mixture of lidocaine 1% and mitomycin 0.3 mg/ml beneath the conjunctiva in the superior fornix. I allow 20 minutes for the mitomycin to diffuse in the tissue and then start the procedure. For this purpose, I use a 25-ga. needle on a tuberculin syringe containing only lidocaine 1%.
The needle is inserted in the subconjunctival space lateral to the bleb and a small amount of lidocaine is injected to provide local anesthesia. For example, if the bleb is located between the 11 and 1 o’clock positions, I pass the needle through the conjunctiva at the 2 o’clock position and move the tip forward 5 or 6 mm while injecting lidocaine until it reaches the scar tissue ring. Then I use the tip of the needle to puncture numerous holes through the ring, all the way around it—enough holes that I can then take the needle and mechanically break the scar tissue by sweeping it up and down. Breaking the ring allows the fluid to diffuse out into the adjacent subconjunctival space and relieve the internal pressure on the cystic portion of the bleb. In most cases, I also slide the needle under the scleral flap to lift it a little and allow more aqueous to seep out.
Once the needle is removed, I use forceps to pinch the tissue where I made the needle track and use cautery to seal the hole to prevent any leakage. At the end of the procedure, a diffuse bleb is present. The leak through the cystic portion often heals within days. I do this entire procedure in the office at the slit lamp, although it can also be done in the operating room. I’ve had very good success in healing leaks in small, localized blebs.
Other, less-frequently used non-surgical techniques include autologous blood injection and compression sutures. The former technique in- volves drawing the patient’s blood and injecting a little into the subconjunctival space adjacent to the bleb and within the bleb itself (see picture, above). The theory is that blood causes inflammation and the release of trophic factors that attract fibroblasts to the area to seal the leak. However, in order for this to work, the leak should be close to the edge of the bleb, near healthy conjunctiva that has viable fibroblasts. In a large, diffuse avascular bleb with a central leak, fibroblasts are unlikely to migrate far enough or in sufficient number to repair the leak.
Another technique is compression sutures, first described by Paul Palmberg, MD, at the Bascom Palmer Eye Institute in Miami. (Palmberg PF, et al. IOVS 1996;37:ARVO Ab-stract S444) The idea is to create a narrow rectangle or an “X” made of 8-0 or 9-0 nylon sutures. The anterior suture is passed through 50-percent depth of the limbal cornea, and the posterior aspect is fixated to the fornix episclera. The suture compresses the problematic bleb, flattening the tissue adjacent to the leak. By displacing some of the aqueous away from the hole in the conjunctiva, the leak will have less internal fluid pressure, thus allowing the tissue to heal. (This technique can be used in conjunction with autologous blood.) A small series reported 57-percent success with this procedure.3 I’ve used this technique with some success, but I prefer the more predictable results of a standard bleb revision.
Surgical Repair
The goal of surgical bleb repair is to cover or reinforce the weak con-junctiva with stronger tissue to halt the leak, restore ocular integrity and preserve bleb function. The first two goals are imperative, the latter is desirable. (Unfortunately, the bleb may not function as well after the repair.)
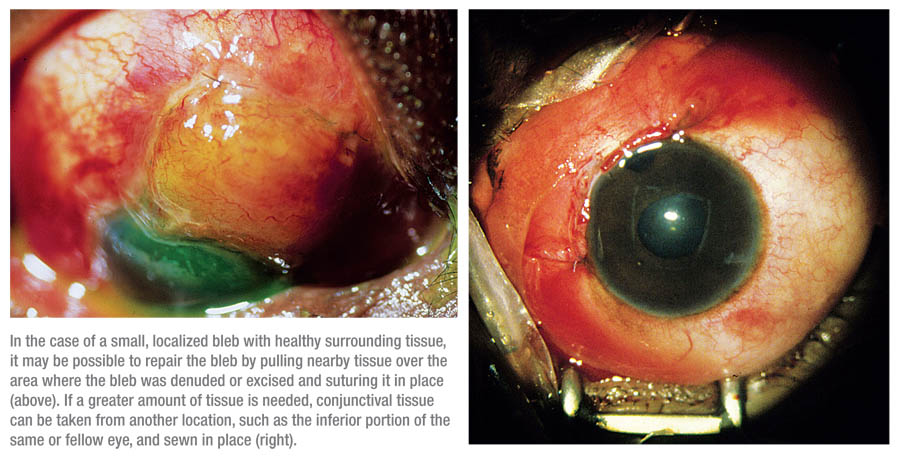
A common element of surgical interventions is covering the bleb, or the area where the bleb was denuded or excised, with intact conjunctiva and then suturing it into place. If the underlying scleral flap has melted or is friable, reinforcement with a patch graft may be necessary. This patch can be made of a variety of tissues, such as sclera, cornea, pericardium or amniotic membrane. The technique used to repair the leak depends on the surface area of the bleb and the health of the surrounding tissue.
For a small localized bleb, a pedicle flap of conjunctiva can be fashioned by making a horizontal incision in the fornix just through conjunctiva, dissecting the conjunctiva from the underlying Tenon’s layer, then pulling it anterior to cover the bleb. With a medium-sized bleb, conjunctival advancement or a rotational conjunctival flap may be necessary. With a large bleb, or a bleb sur-rounded by scar tissue, there may not be sufficient healthy adjacent conjunctiva to cover the bleb. Thus, a free conjunctival graft from the same or fellow eye may be needed. Amniotic membrane grafts have also been used, with limited success, to cover the bleb when adequate conjunctiva is not available, or glued on the surface of the bleb using a tissue adhesive to allow the underlying friable tissue to heal. Buccal mucosa from inside the lower lip can also be used as a graft if there is no suitable conjunctiva.
When repairing a bleb, the first thing I do is dissect around the edges of the bleb to preserve as much of the normal conjunctiva as possible. Next, I denude the surface of the bleb and remove the epithelium so that whatever I put on top of it will adhere. If the sclera under the bleb is very friable and degenerated, I may also sew a patch graft over the scleral flap.
Once the leaking bleb has been partly or completely removed, the conjunctival tissue defect must be closed. Depending on the amount of tissue needed, I either use a relaxing incision to free nearby con-junctival tissue so it can be rotated or slid toward the limbus, or I use conjunctiva taken from another location, such as the inferior portion of the same eye or fellow eye; I graft it over the area where the leaking bleb was located. I sew it in place with 8-0 Vicryl on a taper needle to minimize tissue trauma.
Following the Patient Postop
After surgery, I see the patient the next day and check for leaks along all of the suture tracks. If everything looks good, I prescribe a topical fluoroquinolone and a topical steroid q.i.d. Then I see the patient every week to 10 days for about three visits. If the leak has not recurred by then, I feel comfortable that the operation was successful.
The appearance of the new bleb will depend on which type of repair you performed. If adjacent conjunctiva was mobilized to cover the flap, it should have started to heal down after a week; if the leak has not recurred by then, you’re probably fine. On the other hand, if you do the free conjunctival graft, when the patient comes back on the first day all the tissue in the graft will look very pale—even a little scary—because it’s been disconnected from its blood supply. However, the graft should start to vascularize at the edges within a week.
When you see the patient at one week, the graft may still be pale in the center, but it should be more vascularized around the edges where the sutures are; this indicates that the blood vessels have grown across the host-graft interface into the graft. After that, each time the patient re-turns the pale section in the center should be smaller until it’s been completely revascularized. If the graft doesn’t vascularize, the tissue be-comes necrotic and sloughs off; the graft is gone.
To help ensure the healing of the repair, I put the patient on the same precautions as after a trabeculectomy: don’t lift anything weighing more than 10 pounds; keep head above heart to prevent pressure around the eye; and keep the eye protected by wearing a shield at night and glasses during the day. I have the patient take those precautions for about two weeks.
Other Postop Concerns
One problem you may encounter following a bleb repair is that once the leak heals, intraocular pressure can rise. A repaired bleb is usually thicker than the original, and that can affect how well it functions. So, a patient might come in with a bleb that’s small, cystic and leaking with a pressure of 2 mmHg; but once you’ve repaired the bleb, the pressure may rise to 10 or 15 mmHg or higher.
Because of this, it’s possible that the patient may need more medication to control his glaucoma after the repair than before. I tell patients, “Your pressure is low now, but after I fix this, it will likely be higher and you may have to go back on your eyedrops.”
Hoping for Something Better
Leaking blebs certainly contribute to the feeling that ophthalmologists need a better alternative than trabeculectomy to lower the IOP and treat glaucoma. But so far, despite new surgical and nonsurgical alter-natives, trabeculectomy remains the gold standard. Even some of our patients are aware of the potential downsides of trabeculectomy. I have a patient who has waited for 10 years for something better to come along.
For now, we’re likely to continue creating blebs and occasionally managing bleb leaks. It’s an imperfect solution—but it’s helped to preserve vision in many, many eyes. Fortunately, that’s the bottom line.
Dr. Miller-Ellis is a professor of clinical ophthalmology and director of the Glaucoma Service at the Scheie Eye Institute of the University of Pennsylvania Health System in Philadelphia.
1. DeBry PW, Perkins TN, Heatley G, Kaufman P, Brumbeck LC. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol 2002;120:297-300.
2. Ressiniotis T, Khaw PT. Procedural treatments: Trabeculectomy. In: Giaconi JA, Law SK, Coleman AL, Caprioli J, eds. Pearls of Glaucoma Management. Berlin: Springer-Verlag, Heidelberg, 2010:271-278.
3. Biswas S, Zaheer I, Monsalve B, Diamond JP. Compression sutures with autologous blood injection for leaking trabeculectomy blebs. Br J Ophthalmol 2009;93:549-550.
Further reading:
1. Al-Shahwan S, Al-Torbak AA, Al-Jadaan I, Omran M, Edward DP. Long-term follow up of surgical repair of late bleb leaks after glaucoma filtering surgery. J Glaucoma 2006;15:432-436.
2. Ares C, Kasner OP. Bleb needle redirection for the treatment of early postoperative trabeculectomy leaks: A novel approach. Can J Ophthalmol 2008;43:225-228.
3. Dinah C, Bhachech B, Ghosh G. Long-term success with autologous blood injection for leaking trabeculectomy blebs. Br J Ophthalmol 2010;392-393.
4. Au L, Wechsler D, Spencer F, Fenerty C. Outcome of bleb revision using scleral patch graft and conjunctival advancement. J Glaucoma 2009;18:331-335.
5. Budenz DL, Barton K, Tseng SCG. Amniotic membrane transplantation for repair of leaking glaucoma filtering blebs. Am J Ophthalmol 2000;130:580-588.
6. Burnstein AL, WuDunn D, Knotts SL, Catoira Y, Cantor LB. Conjunctival advancement versus nonincisional treatment for late-onset glaucoma filtering bleb leaks. Ophthalmology 2002;109:71-75.
7. Catoira Y, WuDunn D, Cantor LB. Revision of dysfunctional filtering blebs by conjunctival advancement with bleb preservation. Am J Ophthalmol 2000;130:574-579.
8. Harizman N, Ben-Cnaan R, Goldenfield M, Levkovitch-Verbin H, Melamed S. Donor scleral patch for treating hypotony due to leaking and/or overfiltering blebs. J Glaucoma 2005;14:492-496.
9. Kee C, Hwang J. Amniotic membrane graft for late-onset glaucoma filtering leaks. Am J Ophthalmol 2002;834-835.
10. Kitagawa K, Yanagisawa S, Wantanabe K, Yunoki T, et al. A hyperdry amniotic membrane patch using a tissue adhesive for corneal perforations and bleb leaks. Am J Ophthalmol 2009;148:383-389.
11. Radhakrishnan S, Quigley HA, Jampel HD, Friedman DS, et al. Outcomes of surgical bleb revision for complications of trabeculectomy. Ophthalmology 2009;116:1713-1718.
12. Rauscher FM, Barton K, Budenz D, Feuer WJ, Tsenj SCG. Long-term outcomes of amniotic membrane transplantation for repair of leaking glaucoma filtering blebs. Am J Ophthalmol 2007;143:1052-1054.
13. Rootman DB, Kumar NL, Rootman DS, Trope GE. Buccal mucous membrane for the reconstruction of complicated leaking trabeculectomy blebs. J Glaucoma 2010;19:270-4.
14. Schnyder CC, Shaarawy T, Ravinet E, Achache F, et al. Free conjunctival autologous graft for bleb repair and bleb reduction after trabeculectomy and nonpenetrating filtering surgery. J Glaucoma 2002;11:10-16.
15. Seligsohn A, Moster MR, Steinmann W, Fontanarosa J. Use of Tisseel fibrin sealant to manage bleb leaks and hypotony. J Glaucoma 2004;13:227.
16. Spencer NA, Lee C, Diamond J. Combined conjunctival relieving incisions and advancement for the repair of late-onset leaking trabeculectomy blebs. J Glaucoma 2007;16:384-387.
17. Tannenbaum DP, Hoffman D, Greaney MJ, Caprioli J. Outcomes of bleb excision and conjunctival advancement for leaking or hypotonous eyes after glaucoma filtering surgery. Br J Ophthalmol 2004;88:99-103.
18. Wadhwani RA, Bellows AR, Hutchinson BT. Surgical repair of leaking filtering blebs. Ophthalmology 2000;107:1681-1687.




