In the 1990s, limbal relaxing incisions by and large replaced astigmatic keratotomy on the cornea for astigmatism correction. “The cornea has circumferential fiber rings around the limbus that extend within 1.5 D of the blood vessels of the limbus, so when you cut within that zone right next to the limbus and along, rather than across, the annulus of fibers, the cornea isn’t weakened as much and you don’t end up with wacky overcorrections,” explains Steven G. Safran, MD, PA, a staff surgeon at Robert Wood Johnson University Hospital in Hamilton, New Jersey. “We made the switch to limbal relaxing incisions from corneal incisions because they’re safer.”
Often done in conjunction with cataract surgery—most cataract surgery candidates have at least 1.25 D of astigmatism1—incisional keratotomy methods such as manual LRIs enjoy a long history of published studies supporting their safety and efficacy for astigmatism correction,2-5 in addition to well-developed nomograms, some of which have been in use for over 20 years. Performing manual incisions is relatively inexpensive, since there’s no need to purchase an expensive femtosecond laser. All you need to perform incisional keratotomy is a toric axis marker and a diamond knife, which can last forever with the proper care, experts say.
More recently, femtosecond lasers have been on the rise for managing astigmatism in conjunction with cataract surgery,6-7 making it very simple and convenient for the ophthalmic surgeon to create LRIs with the laser at the time of laser-assisted cataract surgery. Proponents of laser-assisted cataract and LRI procedures say that the femtosecond laser can ensure and increase incisional precision and uniformity. Additionally, technologies like pachymetry, real-time OCT and topography can be paired with the laser for added safety and improved anatomical visualization.
In this article, we’ll hear from proponents of both methods, and discuss the current pros and cons of lasers and knives.
Pro Laser
Preeya K. Gupta, MD, a corneal specialist at the Duke Eye Center, says that the femtosecond laser provides an easy way to integrate astigmatism correction into your clinical practice, especially if you’re already using the laser to do cataract surgery. “Adding astigmatism correction takes only seconds of additional time. We should all be correcting even low levels of astigmatism, because it leads to better visual outcomes,” says Dr. Gupta. “The femtosecond laser provides a precise and automated way to do this.”
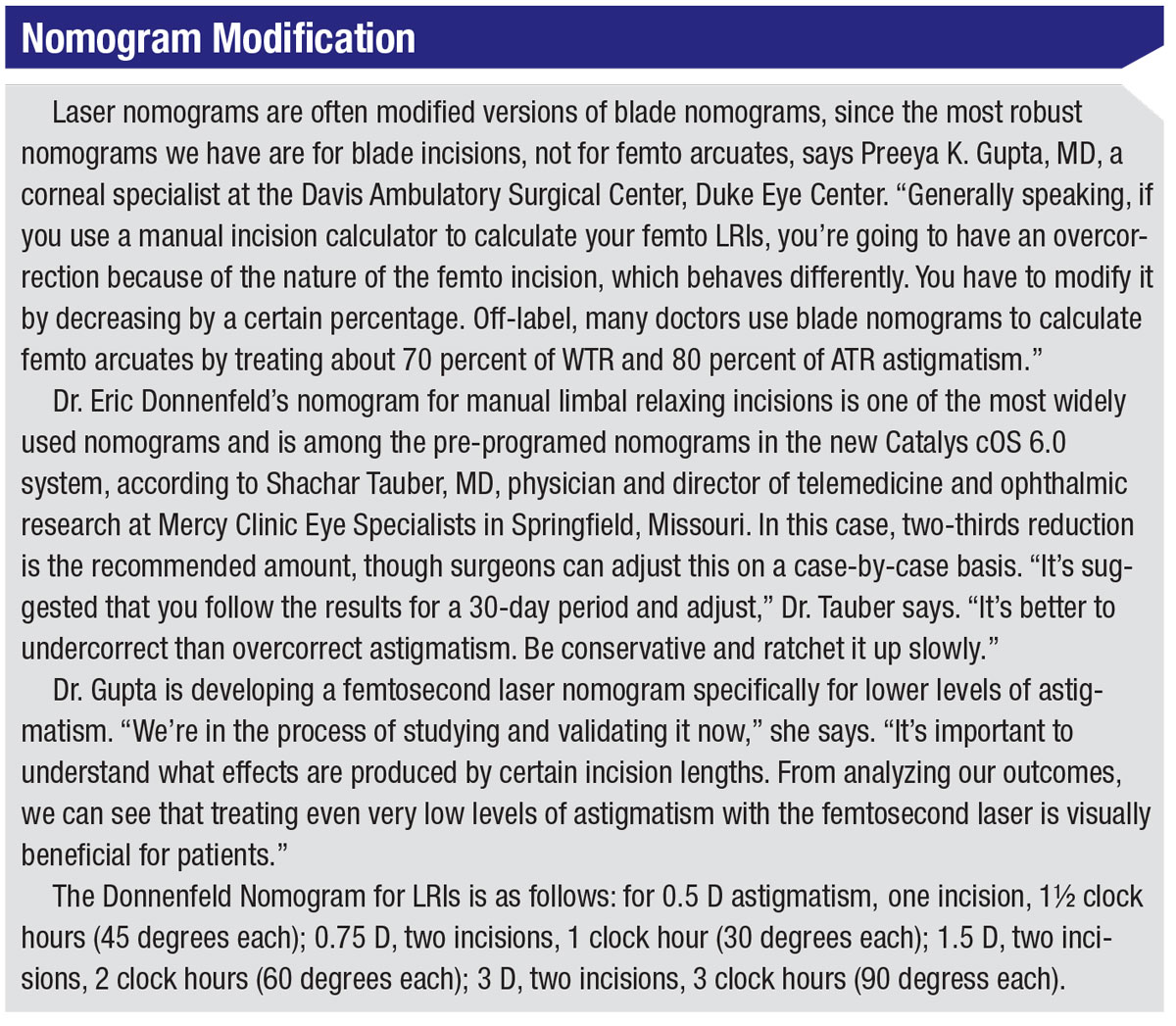 |
Dr. Gupta, who uses the LenSx laser from Alcon, prefers the laser to manual methods for a couple of reasons. “Before I started using the femtosecond laser, I did manual LRIs, but I didn’t do them on every patient,” she says. “I’d reserve them for patients who had 1 D or more of astigmatism. With the laser, on the other hand, I consider treating even low levels of astigmatism. I treat astigmatism for every laser cataract surgery patient.”
It’s partly a matter of convenience, she explains. “If I’m already sitting at the laser for cataract surgery, it’s not a lot of extra effort to treat astigmatism at the same time,” she says. “The patient is already docked to the laser, whereas if I were to switch to manual incisions, it’d require several extra steps: You need to make a plan, have other instruments and have the patient sit up for marking. Using the laser for both cataract surgery and astigmatism correction makes sense from a practical standpoint.”
Shachar Tauber, MD, lead physician on the specialty council and director of telemedicine and ophthalmic research at Mercy Clinic Eye Specialists in Springfield, Missouri, who began his medical journey in the radial keratotomy and astigmatic keratotomy school of refractive surgery, says he was very grateful when excimer and femtosecond lasers arrived on the scene. “I’ve gotten completely away from manual keratotomy, even for transplants,” says Dr. Tauber, who uses the Catalys laser from Johnson & Johnson Vision. “I can have cyclotorsion set up for better accuracy with my marking, and I can pair my laser to the topographer. Incorporating topographic imaging allows for proper orientation of the steep axis and better planning of arcuates. With a laser, I feel confident that the quality, placement and accuracy of the incisions are excellent.”
Here are some reasons surgeons love their lasers:
• Improved precision. Dr. Gupta and Dr. Tauber both agree that, though surgeons are very skilled in creating manual incisions, achieving a level of precision comparable to that of a laser is difficult. “There’s more variability with manual incisions,” Dr. Tauber says. “With a laser I can input the exact number of degrees I want and set variables, like the optical zone diameter based on the pupil or the limbus, and be equal on both sides. The length and depth of the incision are also set up by the laser, so it doesn’t depend on my hand. If we look at the precision of a laser for astigmatic incisions—whether intrastromal or anterior penetrating—it’s quite precise, and the error is very small and very consistent. Arcuate incisions for the Catalys were clinically validated within 0.83 ±0.66 percent of intended optical zone, 0.22 ±0.2 degrees of intended axis and 0.22 ±0.29 degrees of intended length.”8
“The curvature of the incision is also very precise with a laser,” Dr. Gupta adds. “You can standardize its placement on the optical zone a little more precisely than with manual methods.”
• Intrastromal incisions. “What attracted me initially to the laser was the ability to do intrastromal arcuate incisions,” says Dr. Tauber. “The laser leaves the top and bottom 20 percent [of the cornea] intact; this makes for a more pristine ocular surface. You can’t correct as much astigmatism with intrastromal incisions, and your incisions will need to be longer, but that’s the extent of its limitations. You can’t do intrastromal incisions manually.”
Intrastromal incisions began with nomograms created by Dr. Julian
Stevens in London, explains Dr. Tauber. “That’s the nomogram we use,” he says. “We’re working with Dr. Doug Koch at the Baylor College of Medicine to continue perfecting intrastromals. In Europe, others have demonstrated the stability of intrastromal incisions as well as their faster healing rate. So far, there doesn’t seem to be any progression [to corneal melt], which is sometimes seen with anterior penetrating incisions.”
One other benefit of an intrastromal incision is peace of mind—though the possibility of infection is already rare with anterior penetrating incisions, there’s almost no risk of infection with intrastromals. “In theory, there shouldn’t be an infection when an incision doesn’t break the surface,” Dr. Tauber explains.
• Cyclorotation detection. The LensAR, LenSx (Alcon), Victus (Bausch + Lomb) and now the Catalys (Johnson & Johnson Vision) are some of the lasers that include a system for detecting and compensating for cyclorotation. “To me,” says Dr. Tauber, “the dividing line between manual and femto comes down to two things: the laser’s ability to do intrastromal incisions, which is better in my mind for the ocular surface, and the laser’s cyclorotation detection and correction. For the first time in the history of astigmatic correction we’re no longer using ink pen-style marking, which has a significant number of inaccuracies built into it for both astigmatic incisions and toric IOLs. With the advent of cyclorotation detection and correction, the femtosecond laser has become a solid tool.
“Traditionally, we marked the cornea with ink at the slit lamp or as the patient entered the operating room,” Dr. Tauber continues. “However, a paper in 2011 showed that manual marking error can amount to more than nine degrees, with a range up to 10 degrees.9 That’s quite a margin of error. Femtosecond lasers reduce that error, so we’re thrilled.”
• Real-time OCT. Manual LRIs may be dislocated or penetrate the cornea too deeply. Using OCT in conjunction with the femtosecond laser enhances precision and allows surgeons to see how deeply they’re cutting, Dr. Gupta points out. With OCT, surgeons can obtain in seconds images of the anterior and posterior cornea, in addition to pachymetry, corneal diameter, anterior chamber depth and iris boundaries. “OCT allows us to plan and program the laser to treat at a specific depth, say 80 percent,” she says. “When doing manual incisions, we’re not able to precisely image the cornea, so there’ll be some variability not only in depth of placement but also in the incision itself. Depending on the force of pressure, it’s also possible to perforate the cornea.”
“You have several safety margins when OCT gives you the anatomy,” adds Dr. Tauber. “Real-time OCT will change if your patient moves, which allows you to either stop before you start or to abort an incision, whether it be for cataract removal, a paracentesis or an arcuate. If your patient moves enough, the OCT will show you that the incision may not be where you want it. This rarely happens, but it’s a beautiful safety factor.”
Pro Manual
 |
“A surgeon must interact with the eye—a laser can’t do that,” says Dr. Safran, who finds lasers to be overkill at best and dangerous at worst. He says that while many studies show it’s possible to use a femtosecond laser for keratotomy and cataract surgery, their findings point to higher complication rates and no clinically-meaningful improvements over conventional means.10-11
David F. Chang, MD, a clinical professor at the University of California, San Francisco, and in private practice in Los Altos, California, says his use of astigmatic keratotomy has declined substantially now that presbyopia-correcting IOLs all come in toric versions and the light adjustable IOL (RxLAL; RxSight) is available. When he does perform astigmatism keratotomy, however, he prefers a blade. “One indication for astigmatic keratotomy is for eyes with low astigmatism (i.e., estimated 0.5 to 0.75 D) because we don’t have lower-power toric IOLs,” he says. “Astigmatic keratotomy is also a less expensive alternative for patients who can’t afford a toric IOL.”
Here are some reasons surgeons prefer to stick with a blade:
• In-clinic convenience. With manual incisions, doctors have the convenience of correcting astigmatism at the slit lamp during a regular postop exam, rather than taking the patient back to the operating room or laser suite. Additionally, some surgeons believe that correcting astigmatism in the postop phase at a follow-up visit may result in better outcomes because the eye is more stable.
Postop astigmatic correction can be very beneficial. For example, Dr. Chang’s preferred way of managing complex astigmatism is the light-adjustable IOL from RxSight. “We can effectively create a ‘customized’ toric IOL several weeks after surgery,” he says. “It’s based on the postop refraction rather than our preop predictions of surgically induced astigmatism, posterior corneal astigmatism, and cylindrical power and axis.”
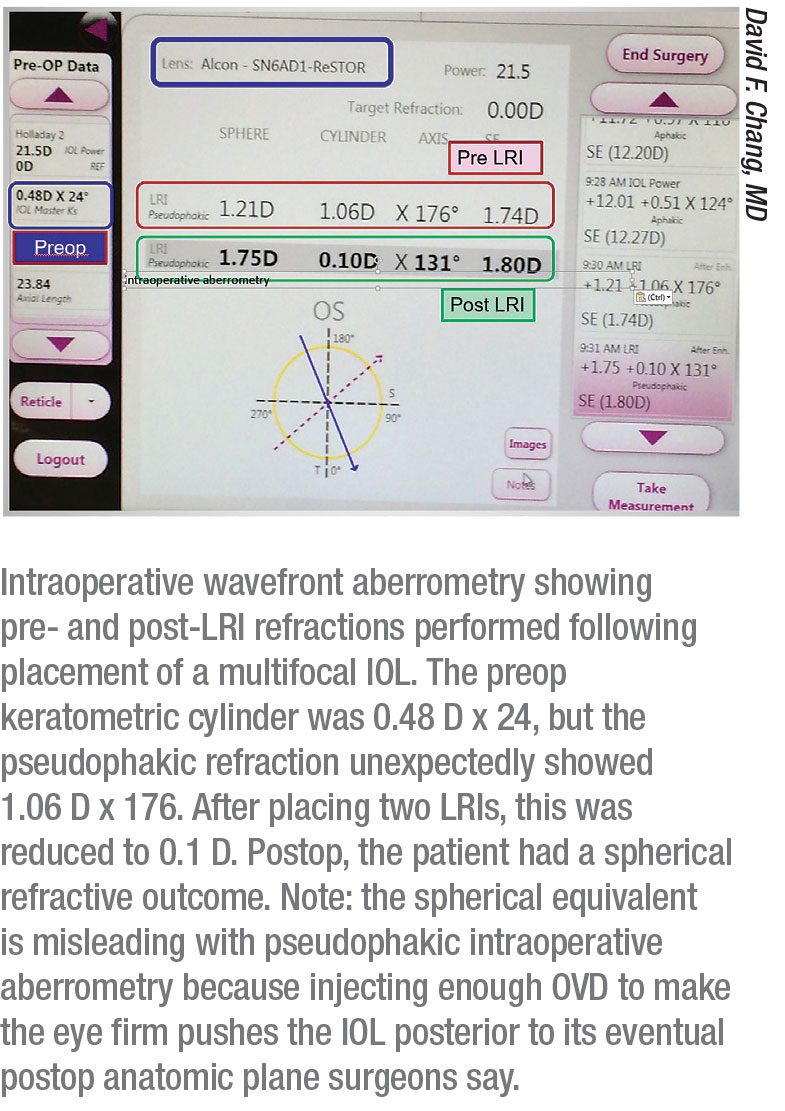
• Intraoperative aberrometry. Dr. Chang says that the best way to improve your LRI results is not by using a femtosecond laser, but by using intraoperative wavefront aberrometry. “Intraoperative wavefront aberrometry has significantly improved my AK results more than relying on preoperative nomogram planning,” he says. “This is because after you place one LRI, you can immediately re-measure the actual refractive astigmatism. Based on this, you could lengthen the first LRI, or add a second LRI opposite to the first. So the best way to improve your LRI results is not by using a femtosecond laser, but rather titrating what you do with pseudophakic intraoperative aberrometry.
“For diffractive multifocal and EDOF IOLs, I always perform intraoperative aberrometry after the IOL implantation,” he continues. “This lets me refine the axis for any toric IOL. If my preop calculations called for a spherical lens, pseudophakic intraoperative aberrometry often indicates some residual astigmatism. Because residual astigmatism reduces multifocal and EDOF performance, I will then add one or two LRIs to reduce the astigmatism to 0.5 D or less, based on titration with intraoperative aberrometry measurements of the live refraction. Femto AK can’t provide me with the important benefit of adding or titrating LRIs based on the pseudophakic intraoperative aberrometry during surgery.”
• Manual is sufficient. One common argument in favor of laser over manual methods is that lasers are more precise. “I think this is misleading,” says Dr. Chang. “There are no long-term studies that have shown superiority of femto AK to either toric IOLs or manual AK. You must have at least six months follow-up to evaluate the regression of effect with incisional keratotomy. There are even conflicting results from studies looking at consistency of femto LRI depth. The greatest variable for astigmatic keratotomy outcomes isn’t the depth of the incision, but corneal hysteresis and patient age.”
Dr. Safran adds that while precision is good, laser-like precision just isn’t necessary. “Besides the fact that laser LRIs are inaccurate by nature, you’re only trying to treat half a diopter or a diopter of astigmatism with an LRI,” he explains. “You’re not trying to treat 3 D. My manual LRI nomograms are small, medium and large, based on the patient’s age and how the tissue responds as I cut it. Let’s say you have a patient with 1.5 D of astigmatism. If I knock it down by 0.75 D or by 1.5 D and correct it all, the patient will be happy. If I overcorrect to 2 D, the patient will be down the other way, but it’s still only by half a diopter. Any correction between 0.75 and 2 D will work. LRIs don’t need to be super precise.”
• Lasers aren’t an improvement. “For years, we had no real peer-reviewed data on femto corneal relaxing incisions until a 2016 paper on intrastromal astigmatic keratotomy,” says Dr. Safran. “But this study reported safety with only one month of follow-up data, and they achieved less than half a diopter of correction.12 Another study of 51 eyes concluded that laser CRIs were effective, but the data show that over the three-month follow-up period, the mean effect of astigmatism correction was decreasing while the range of outcomes was increasing,” he says. “It was getting more unpredictable.13
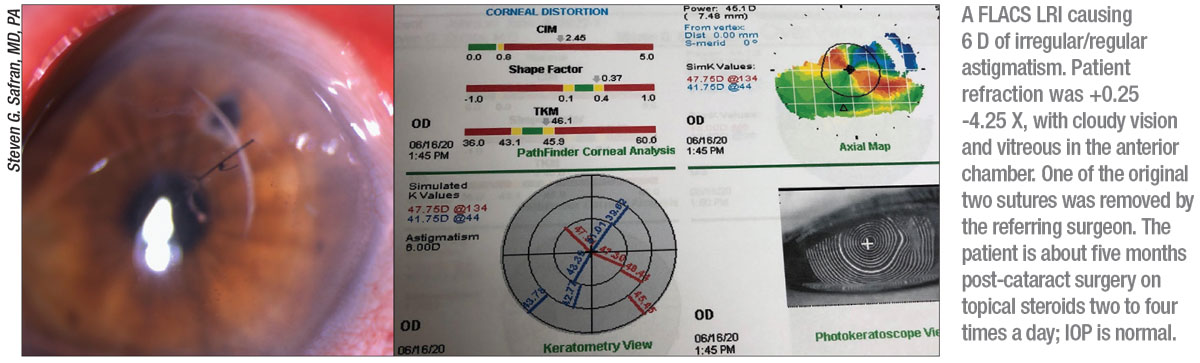
“If you look at the laser studies, there’s very little effect—maybe a quarter of a diopter of correction, and that’s nothing—a homeopathic effect,” he continues. “But when laser goes wrong, it’s not fixable. We stopped cutting the cornea, because you end up with irreparable damage. Femtosecond laser corneal incisions don’t work until they do work, and when they do work, they create problems.”
Dr. Safran points to several studies showing troubling laser side effects in FLACS, which usually precedes laser LRIs, including acidic shifts in aqueous humor pH,14 increased levels of prostaglandins,15,18,11 miosis,16 increased inflammatory mediators and fibroblast growth factor,17-18 and higher rates of posterior capsular tears.11
“There’s no evidence that FLACS is better than phaco, but plenty of studies showing it may increase complications,” Dr. Safran says. “Cutting the cornea with a laser to correct astigmatism is a bit like warming your hands with a burning coal. Nothing happens until you get burnt. Studies show lasers cause more astigmatism and don’t heal as well as manual incisions.”
The European Society of Cataract and Refractive Surgery conducted a multicenter case-control study across nine European countries and Australia that compared the visual, refractive and adverse outcomes of 2,814 FLACS cases and 4,987 conventional phacoemulsification cases.8 Seventy-two percent of FLACS and 74.3 percent of manual phaco eyes were within 0.5 D of target. One percent of FLACS and 0.4 percent of manual phaco eyes had worse postop CDVA of five letters or more at follow-up.
The study data suggest that laser use might be more proinflammatory than conventional phaco, and contribute to higher rates of corneal edema, uveitis requiring treatment and early PCO, reducing visual acuity. Though femto patients had less postop astigmatism and less surgically induced astigmatism in the study, femto didn’t yield better visual or refractive outcomes than conventional phaco. In fact, the femto group had worse postop visual acuity, more postop complications (3.2 percent versus 1.8 percent for phaco) and more patients with worse postop visual acuity than their preop visual acuity.
“Some say that lasers can help less-experienced surgeons achieve better outcomes, but that’s not the case,” Dr. Safran says. He points to a study of Wills Eye residents in which FLACS and manual phaco achieved similar complication rates and visual and refractive outcomes.9 At one month and one year follow-up, visual acuity in the manual phaco group was better (0.11 logMAR [Snellen: 20/26] at one month; 0.08 logMAR [20/24] at one year) than in the femto group (0.13 logMAR [20/27] at one month; 0.13 logMAR at one year), though these between-group differences weren’t statistically significant at either time point. Persistent postop inflammation occurred in significantly more cases in the femto group. The researchers add that rates of macular edema and elevated IOP were similar between the groups.
 |
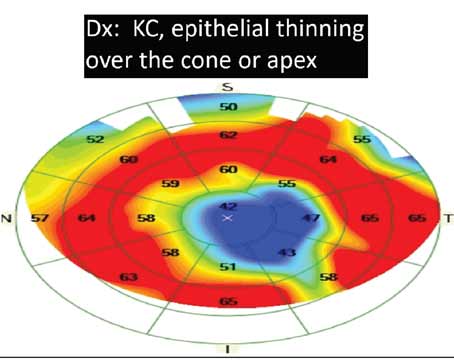
• Cut where you want. “LRIs are much more predictable, heal faster and are safer than laser corneal incisions because you’re cutting along the circumferential corneal annulus of fibers, which contains blood vessels and stem cells,” Dr. Safran says. “If the manual LRI doesn’t work the way I want it to, it doesn’t cause a problem, because it’ll heal. It won’t cause that ectasia pattern that occurs when you cut the cornea.”
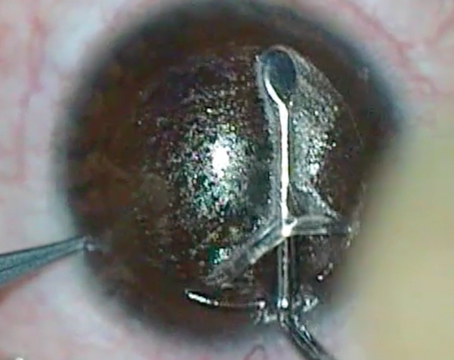
Dr. Safran says he can place manual incisions exactly where he wants them in the limbus, but that’s not possible with a laser. “Because of the laser’s design, you can’t make cuts close enough to the limbus for true LRIs,” he explains. “The cuts don’t end up where they’re supposed to be, and are instead on the peripheral cornea.”20
Intrastromal incisions also suffer from inherent laser inaccuracies, says Dr. Safran. He points to a 2017 study of 77 eyes of 77 patients that used anterior segment OCT to visualize intrastromal corneal incisions and anterior penetrating arcuates to analyze structural changes and location of incisions.21 The researchers found that the intrastromal incisions were frequently placed more anteriorly than planned and that incision midpoint depth varied among patients. They concluded that further improvements are needed to ensure precise incision location. REVIEW
Dr. Gupta is a consultant for Alcon. Dr. Tauber is a consultant for J&J Vision. Dr. Safran has been a speaker for J&J Vision and Optos. Dr. Chang is a consultant for Carl Zeiss, RxSight and J & J Vision.
1. Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, et al. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg 2009;35:1:70-75.
2. Budak K, Friedman NJ, Koch DD. Limbal relaxing incisions with cataract surgery. J Cataract Refract Surg 1998;24:4:503-8.
3. Bayramlar H, Daglioglu MC, Borazan M. Limbal relaxing incisions for primary mixed astigmatism and mixed astigmatism after cataract surgery. J Cataract Refract Surg 2003;29:4:723-8.
4. Monaco G, Scialdone A. Long-term outcomes of limbal relaxing incisions during cataract surgery: Aberrometric analysis. Clin Ophthalmol 2015;9:1581-7.
5. Kim DH, Wee WR, Lee JH, et al. The short term effects of a single limbal relaxing incision combined with clear corneal incision. Korean J Ophthalmol 2010;24:2:78-82.
6.Visco DM, Bedi R, Packer M, et al. Femtosecond laser-assisted arcuate keratotomy at the time of cataract surgery for the management of preexisting astigmatism. J Cataract Refract Surg 2019;45:12:1762-9.
7. Venter J, Blumenfeld R, Schallhorn S, et al. Non-penetrating femtosecond laser intrastromal astigmatic keratotomy in patients with mixed astigmatism after previous refractive surgery. J Refract Surg 2013;29:3:180-6.
8. Culbertson D. Why use a femtosecond laser for incisions? Presented at ESCRS, September 2012. Milan, Italy.
9. Visser N, Berendschot T, Bauer N, et al. Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg 2011;37:8:1394-1402.
10. Ewe S, Abell R, Oakley CL, et al. A comparative cohort study of visual outcomes in femtosecond laser-assisted versus phacoemulsification cataract surgery. Ophthalmol 2016;123:1:178-82.
11. Popovic M, Campos-Möller X, Schlenker MB, et al. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: A meta-analysis of 14,567 eyes. Ophthalmol 2016;123:10:2113-26.
12. Day A, Lau N, Stevens J, et al. Nonpenetrating femtosecond laser intrastromal astigmatic keratotomy in eyes having cataract surgery. J Cataract Refract Surg 2016;42:102-9.
13. Wang L, Zhang S, Zhang Z, et al. Femtosecond laser penetrating corneal relaxing incisions combined with cataract surgery. J Cataract Refract Surg 2016;42:995-1002.
14. Rossi M, Di Censo F, Di Censo M, et al. Changes in aqueous humor pH after femtosecond laser-assisted cataract surgery. J Refract Surg 2015;31:7:462-5.
15. Schultz T, Joachim SC, Kuehn M, et al. Changes in prostaglandin levels in patients undergoing femtosecond laser-assisted cataract surgery. J Refract Surg 2013;29:11:742-7.
16. Jun JH, Hwang KY, Chang SD. Pupil-size alterations induced by photodisruption during femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2015;41:2:278-85.
17. Chen H, Lin H, Zheng D, et al. Expressions of cytokines, chemokines and growth factors in patients undergoing cataract surgery with femtosecond laser pretreatment. PLoS One 2015 Sept 2;10:9:e0137227.
18. Liu YC, Setiawan M, Ang M, et al. Changes in aqueous oxidative stress, prostaglandins, and cytokines: Comparisons of low-energy femtosecond laser-assisted cataract surgery versus conventional phacoemulsification. J Cataract Refract Surg 2019;45:2:196-203.
19. Manning S, Barry P, Henry Y, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: Study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery. J Cataract Refract Surg 2016;42:12:1779-1790.
20. Gavris M, Belicioiu R, Olteanu I, et al. The advantages of femtosecond laser-assisted cataract surgery. Romanian J of Ophthalmol 2015;59:1:38-42.
21. Wang L, Jiang L, Hallahan K, et al. Evaluation of femtosecond laser intrastromal incision location using optical coherence tomography. Ophthalmol 2017;124:8:1120-5.